This document discusses vocal cord palsy, including:
1. It describes the anatomy and innervation of the vocal cords and surrounding structures.
2. It outlines various causes of vocal cord palsy and discusses clinical features and evaluations used to diagnose the condition.
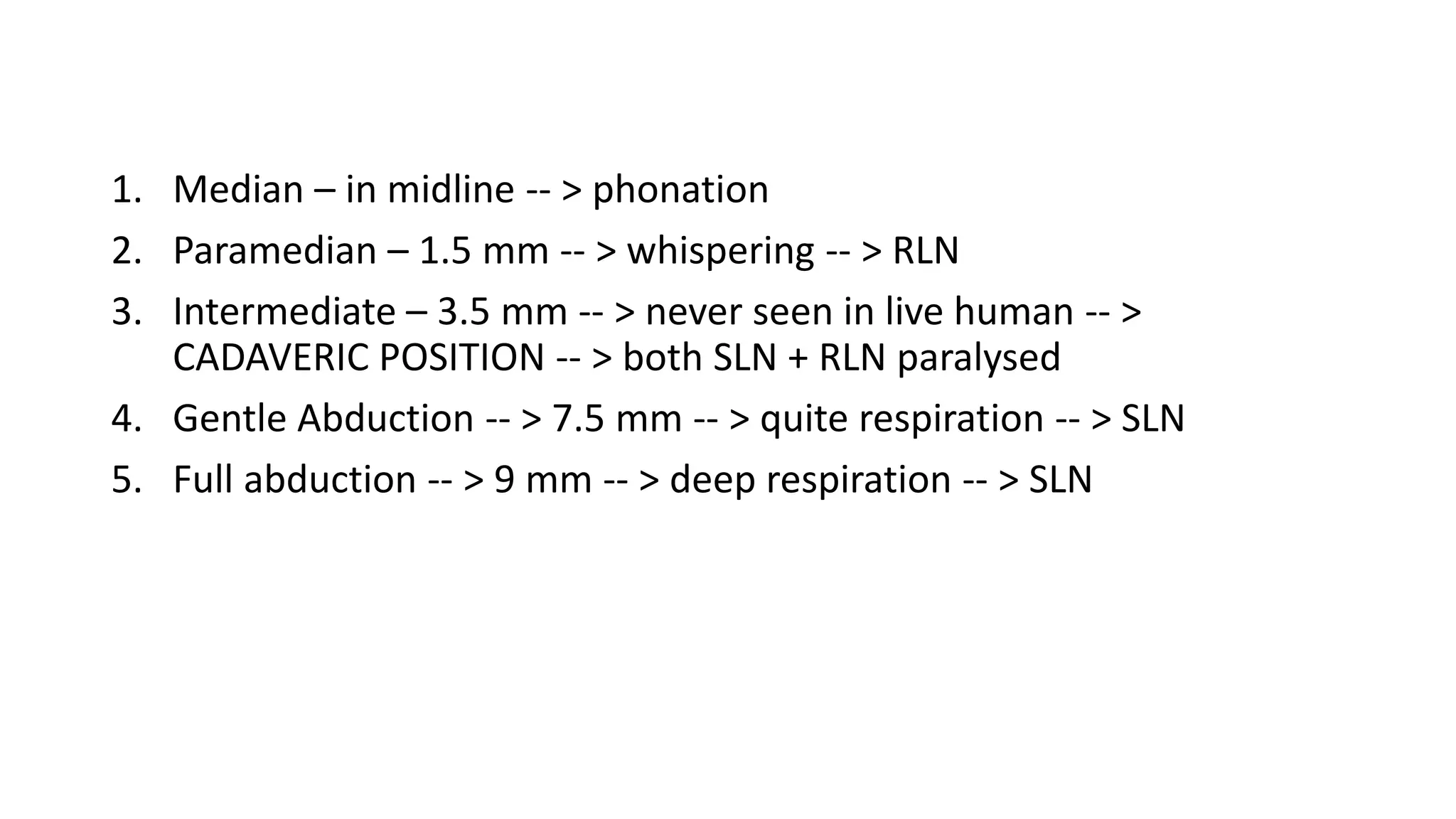
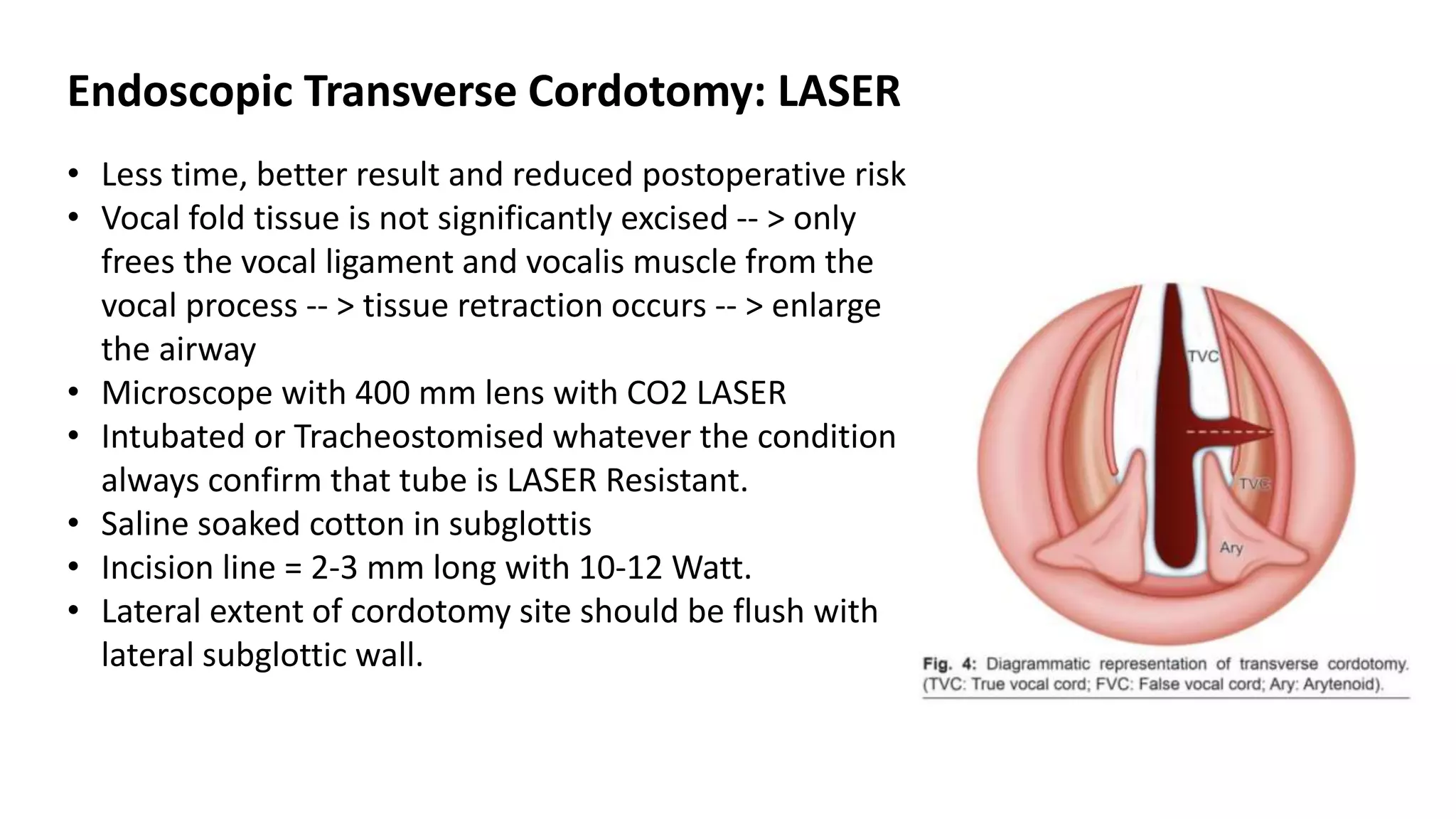
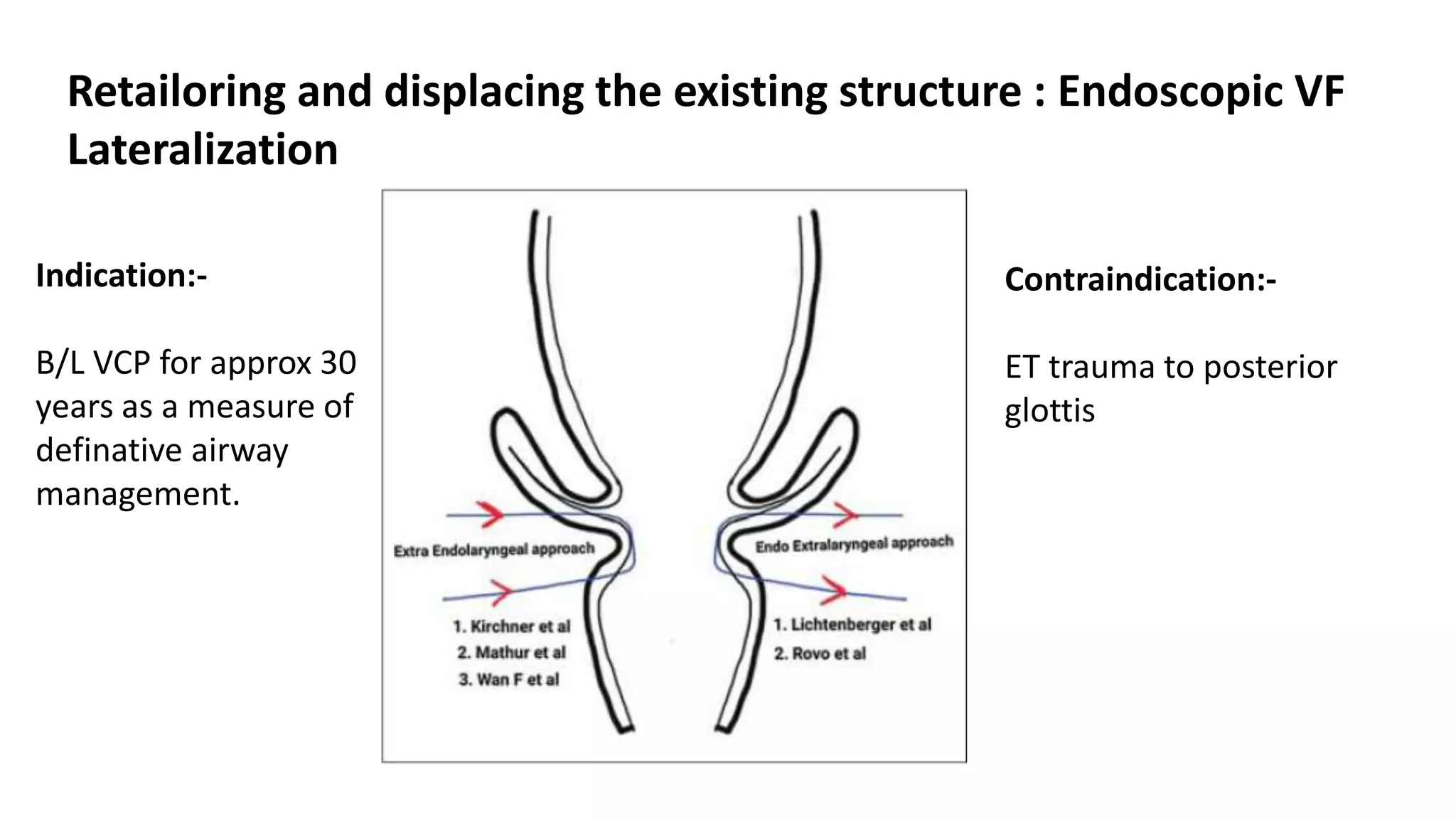
3. It provides an overview of management strategies for unilateral and bilateral vocal cord palsy, both non-surgical and surgical options. Surgical procedures discussed include injection augmentation, medialization thyroplasty, and different types of laryngeal framework surgery.






![RLN Left VCP >>>>Right VCP
1)Extensive Course
2)Pressure [Aortic Aneurism,
Intra thoracic Mass]](https://image.slidesharecdn.com/vocalcordpalsy-210323130348/75/Vocal-cord-palsy-7-2048.jpg)