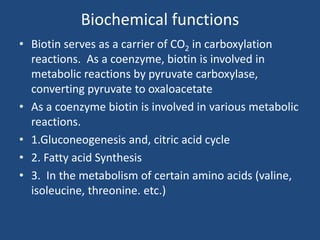
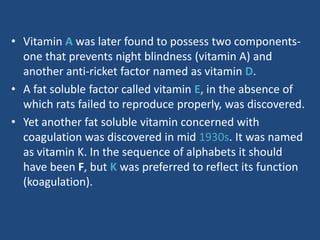
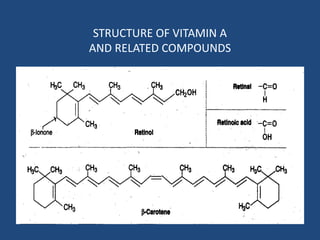
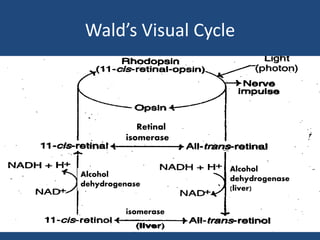
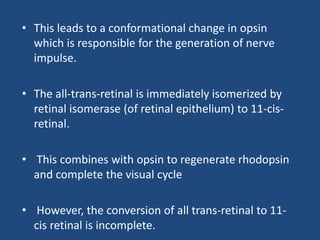
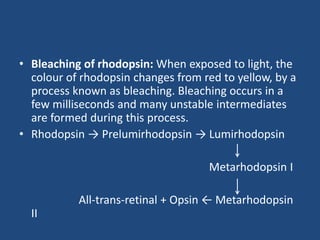
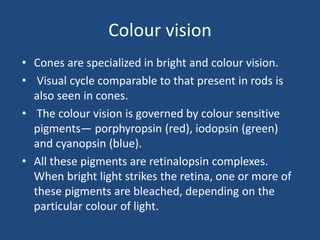
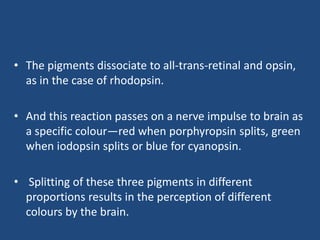
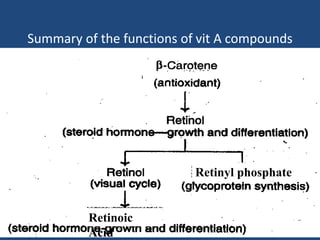
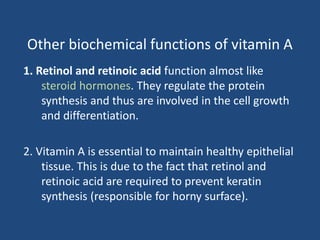
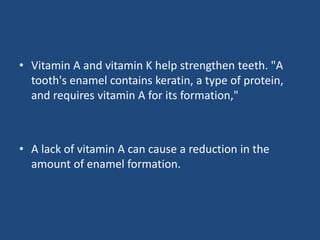
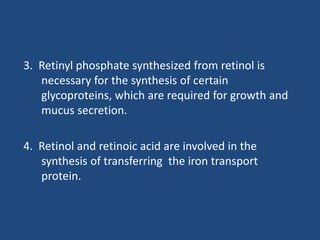
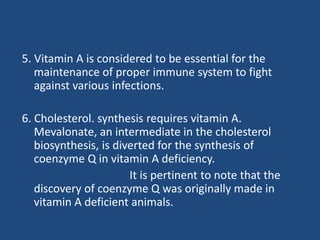
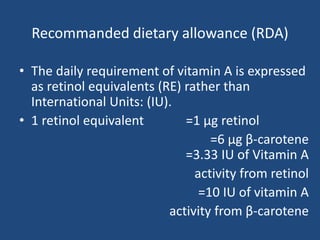
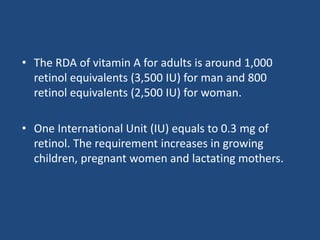
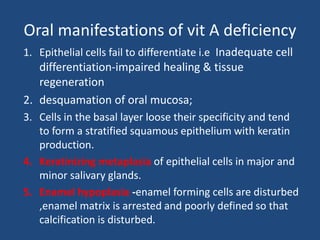
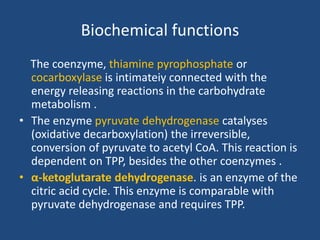
This document provides an overview of vitamins, including vitamin A. It discusses the history and classification of vitamins. Vitamin A, also known as retinol, is a fat-soluble vitamin found in animal foods and plant provitamins called carotenes. Vitamin A plays an important role in vision, cell growth, reproduction, and maintaining epithelial tissues. It is involved in the visual cycle in rods and cones within the retina and helps regenerate the light-sensitive pigment rhodopsin. The recommended daily allowance of vitamin A is expressed in retinol equivalents and is around 1,000 RE for men and 800 RE for women.
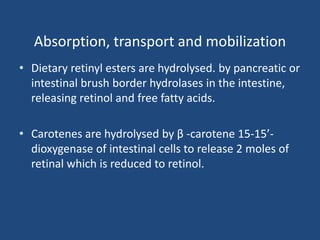


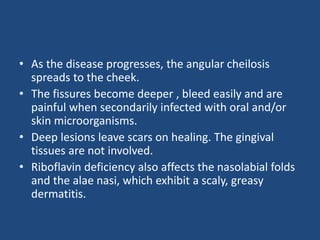
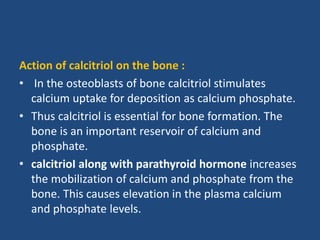
![• ]Some countries where vitamin A deficiency is a
public health problem address its elimination by
including vitamin A supplements available in capsule
form with National Immunization Days (NIDs) for
polio eradication or measles.
• Maternal high supplementation benefits both
mother and breast-fed infant: high dose vitamin A
supplementation of the lactating mother in the first
month postpartum can provide the breast-fed infant
with an appropriate amount of vitamin A through her
milk.](https://image.slidesharecdn.com/vitamins-200618100341/85/Vitamins-78-320.jpg)



![Deficiency symptoms
• The deficiency of vitamin B1 results in a condition
called beri-beri [Sinhalese : I cannot(said twice)].
• Ben-beri is mostly seen in populations consuming
exclusively polished rice as staple food.
The early symptoms of thiamine deficiency are
• loss of appetite (anorexia),
• weakness,
• constipation,
• nausea,](https://image.slidesharecdn.com/vitamins-200618100341/85/Vitamins-159-320.jpg)