Embed presentation
Download to read offline
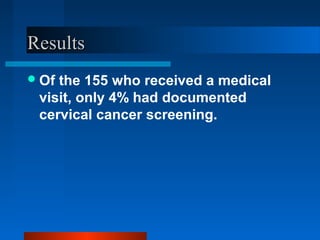
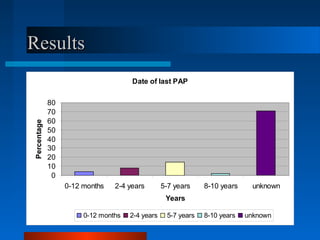
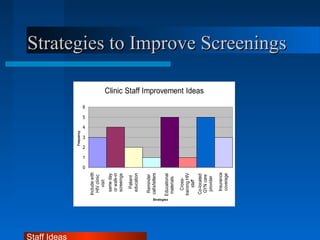
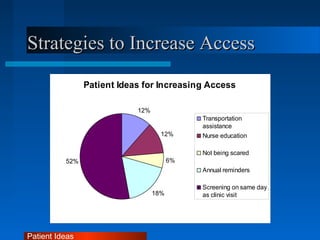
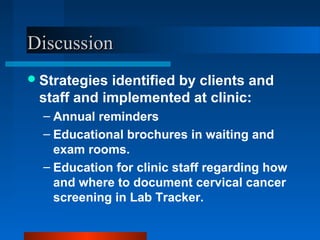
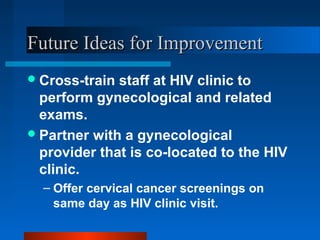

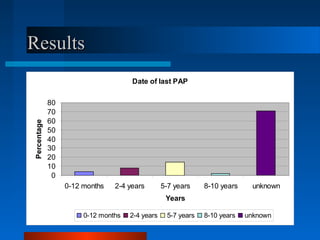
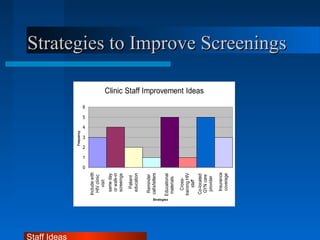
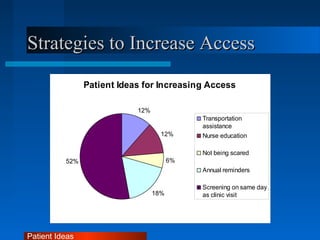
The document discusses a project aimed at improving cervical cancer screening rates at an HIV clinic using the PDCA model. Data collected showed that only 4% of women had documented cervical cancer screenings, highlighting issues with documentation in electronic records. Strategies for improvement included patient education, reminder calls, and co-locating gynecological services with HIV care.