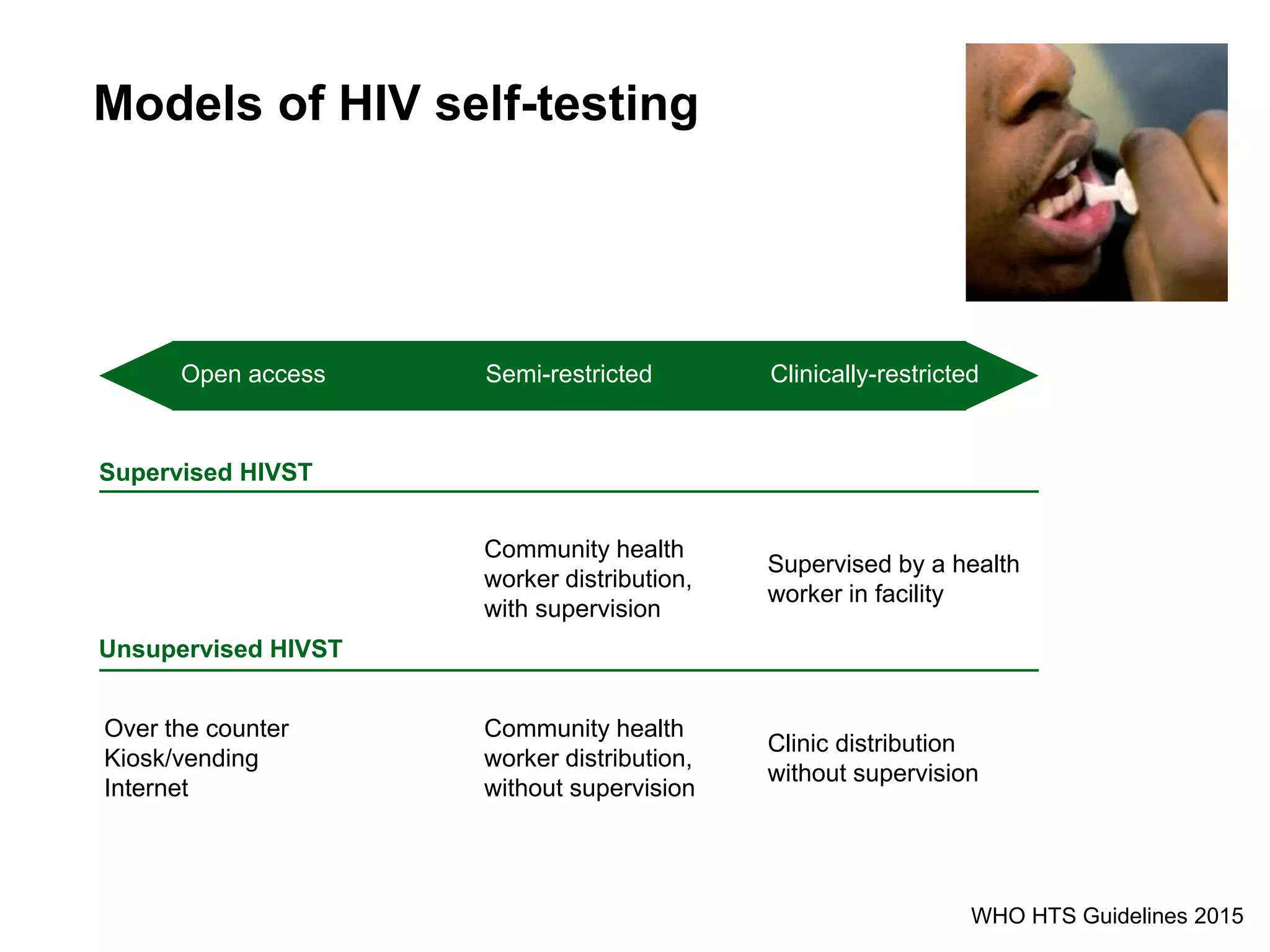
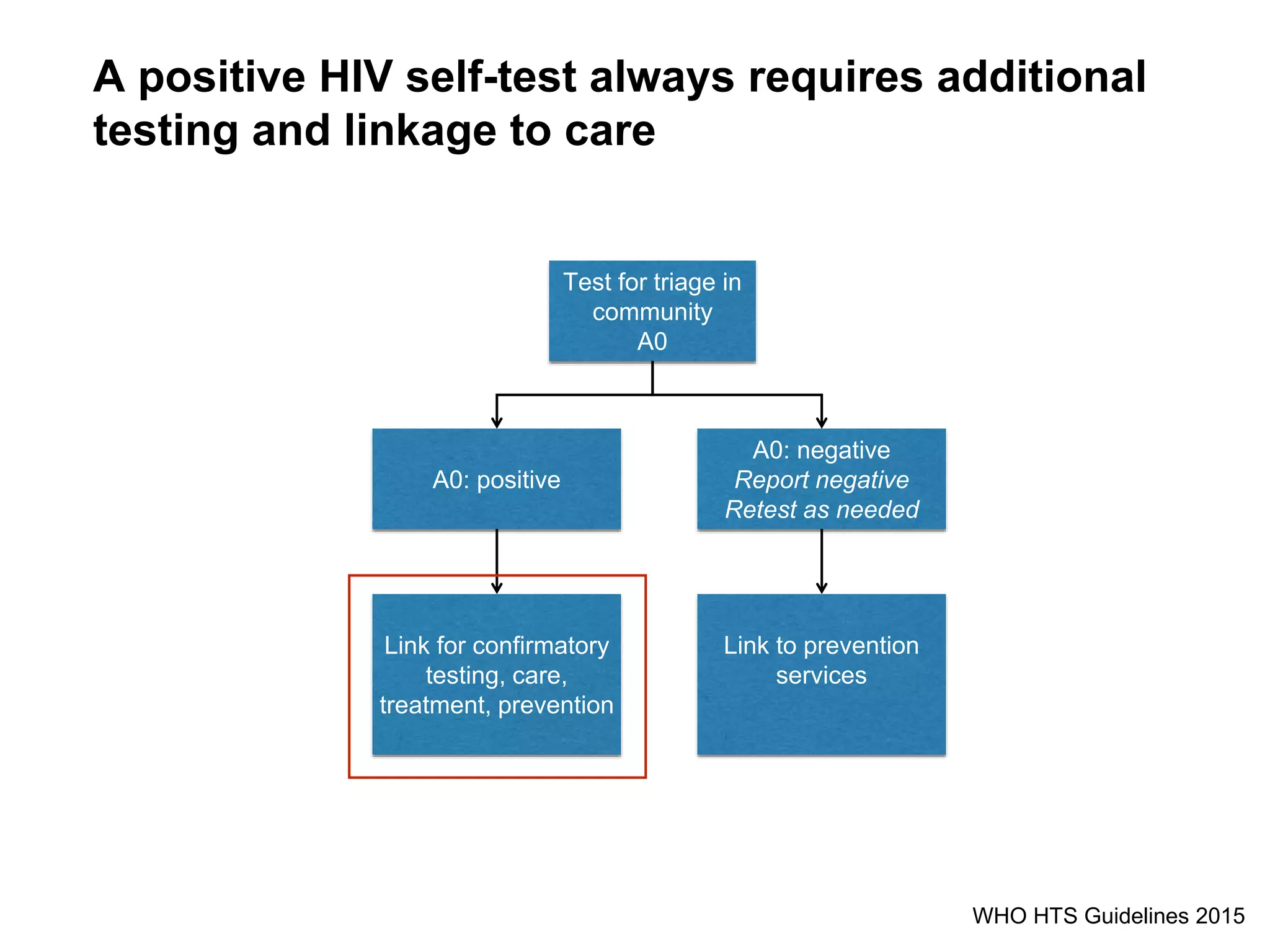
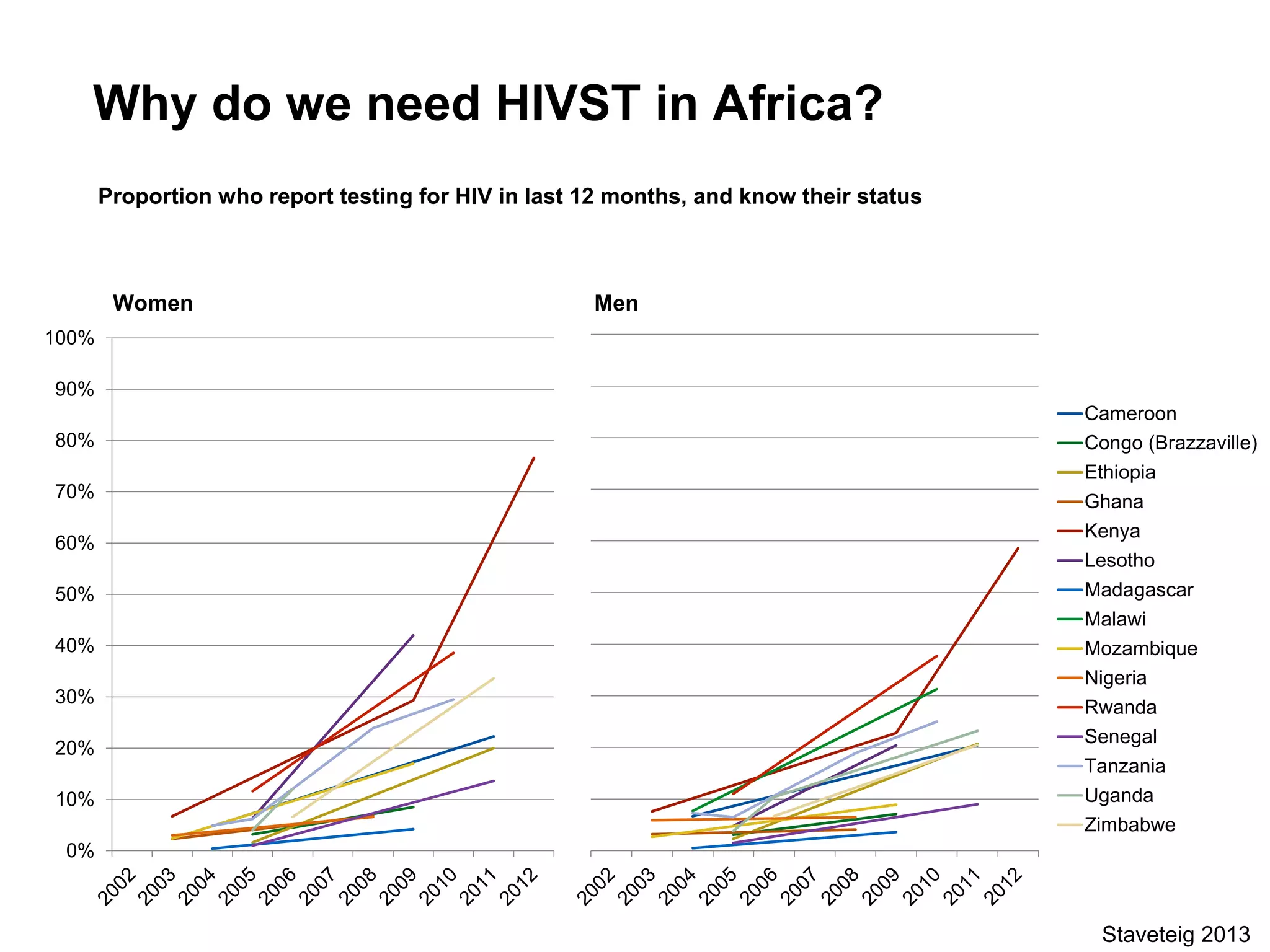
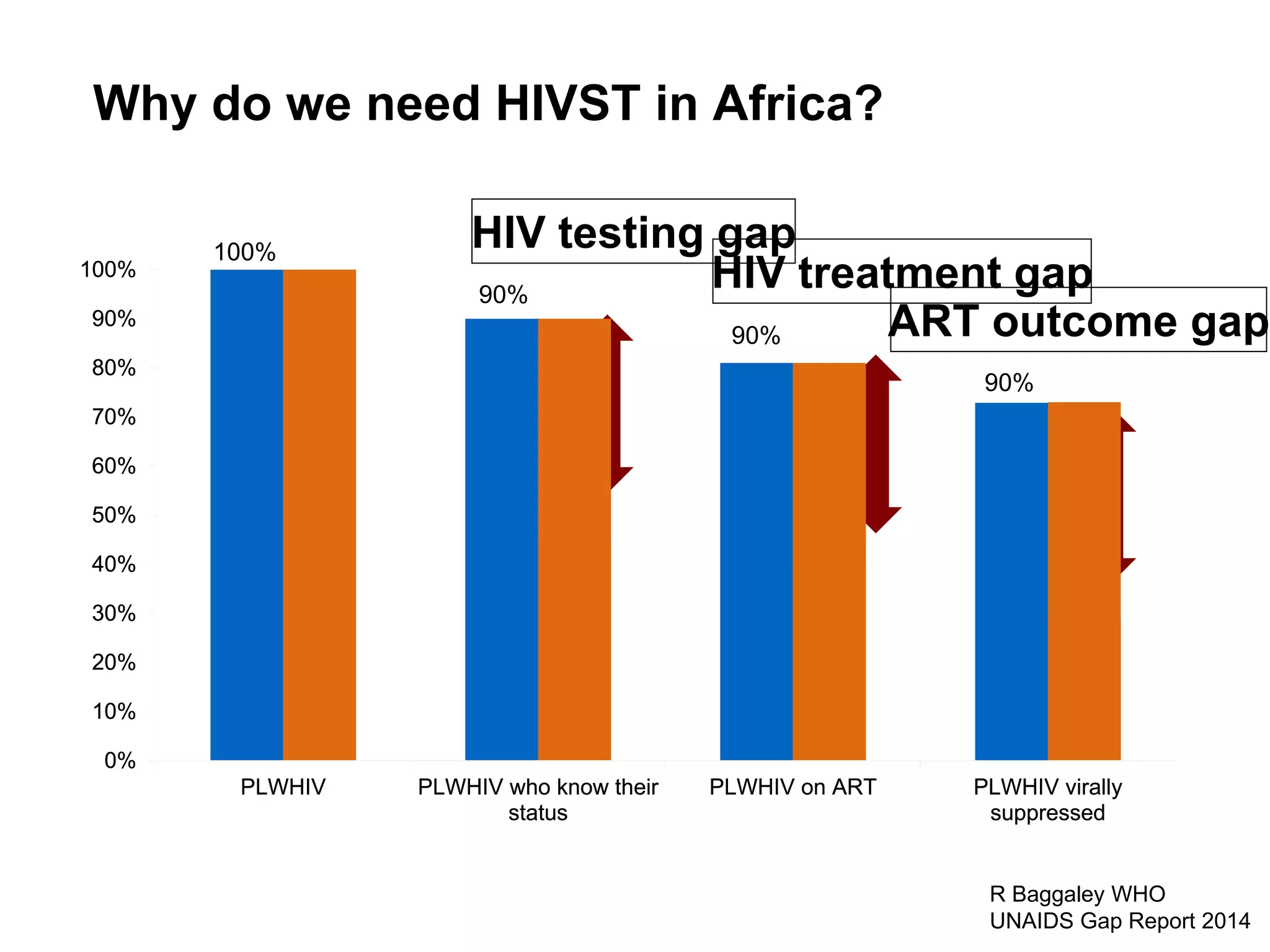
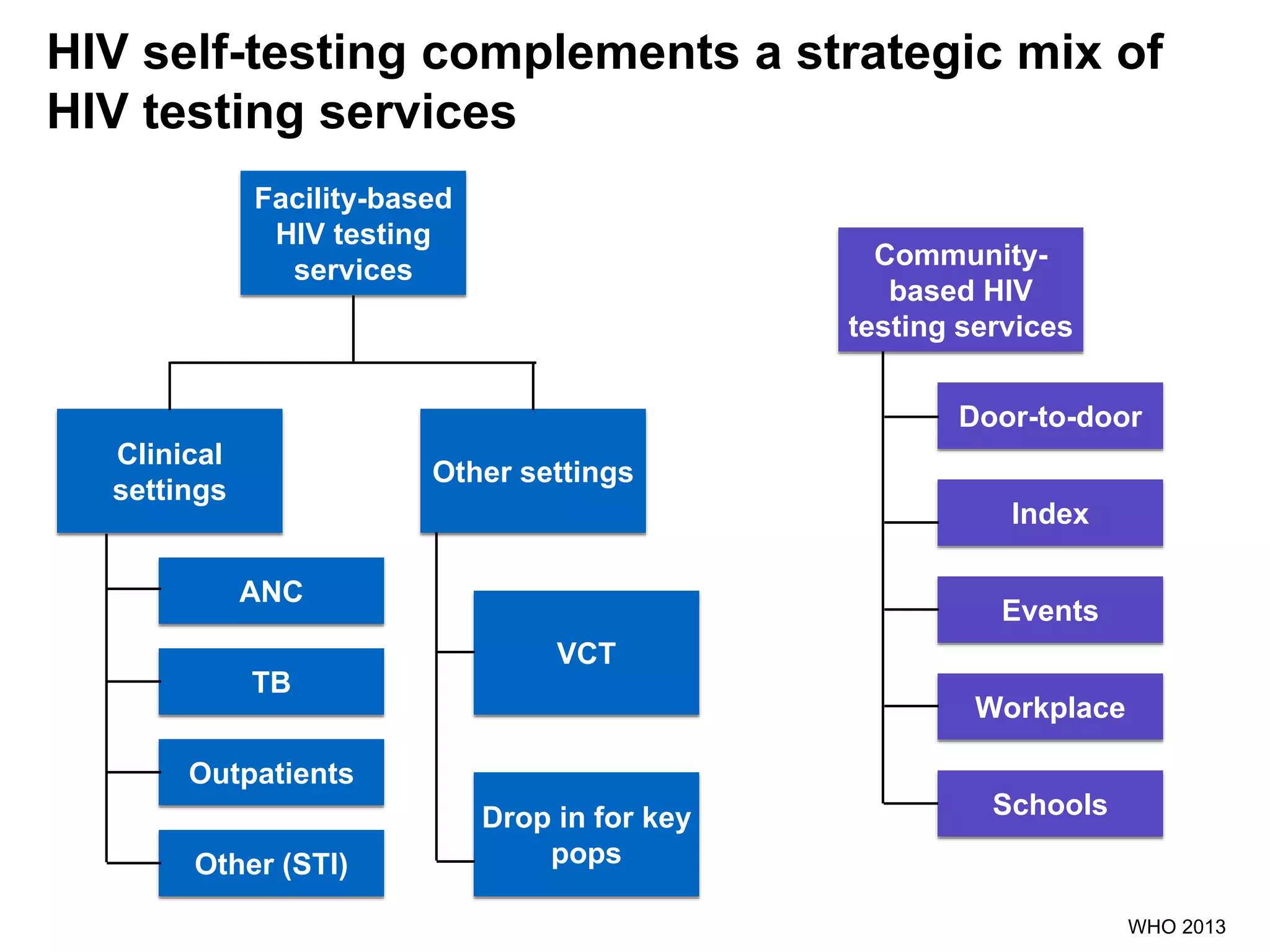
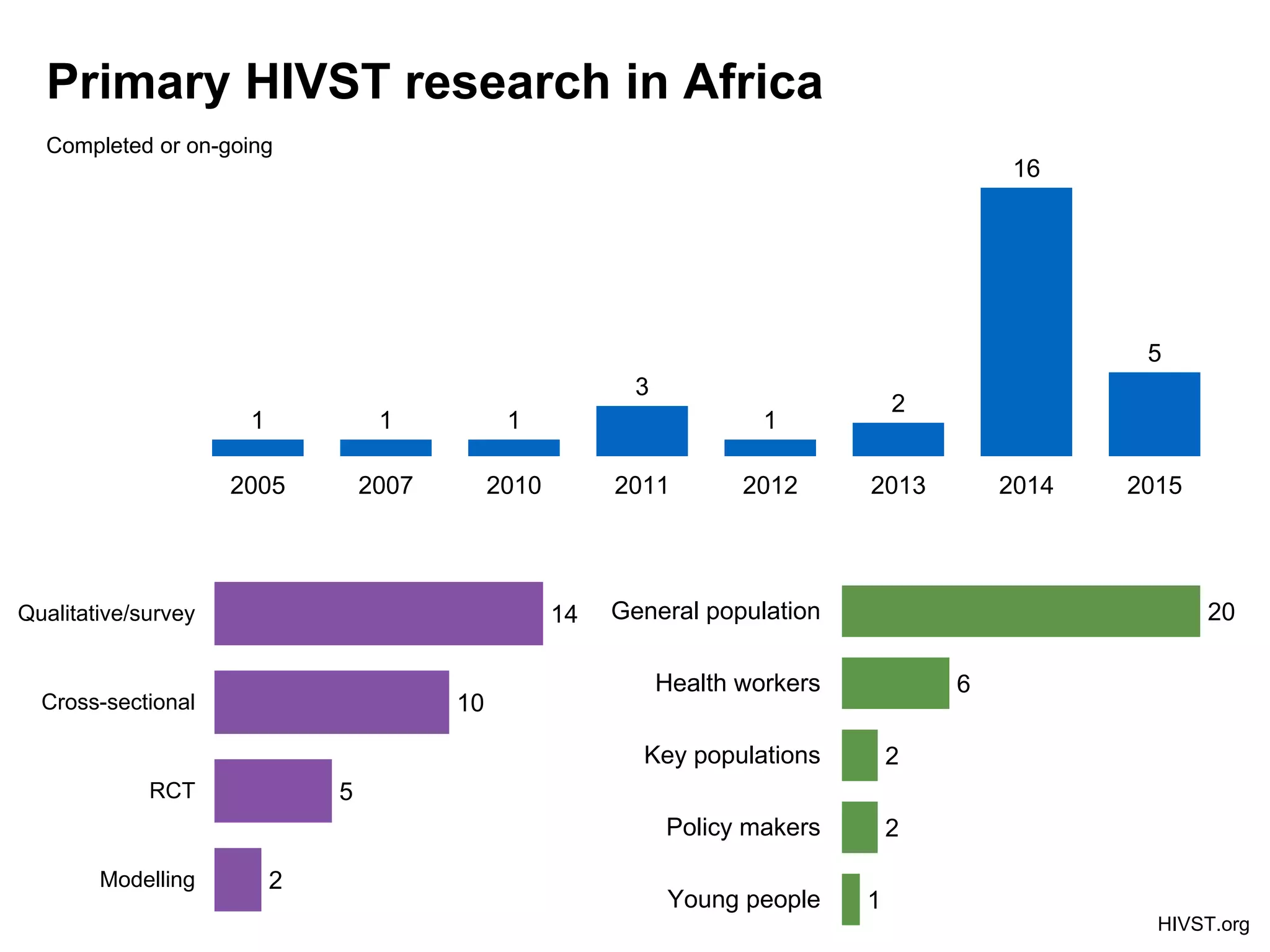
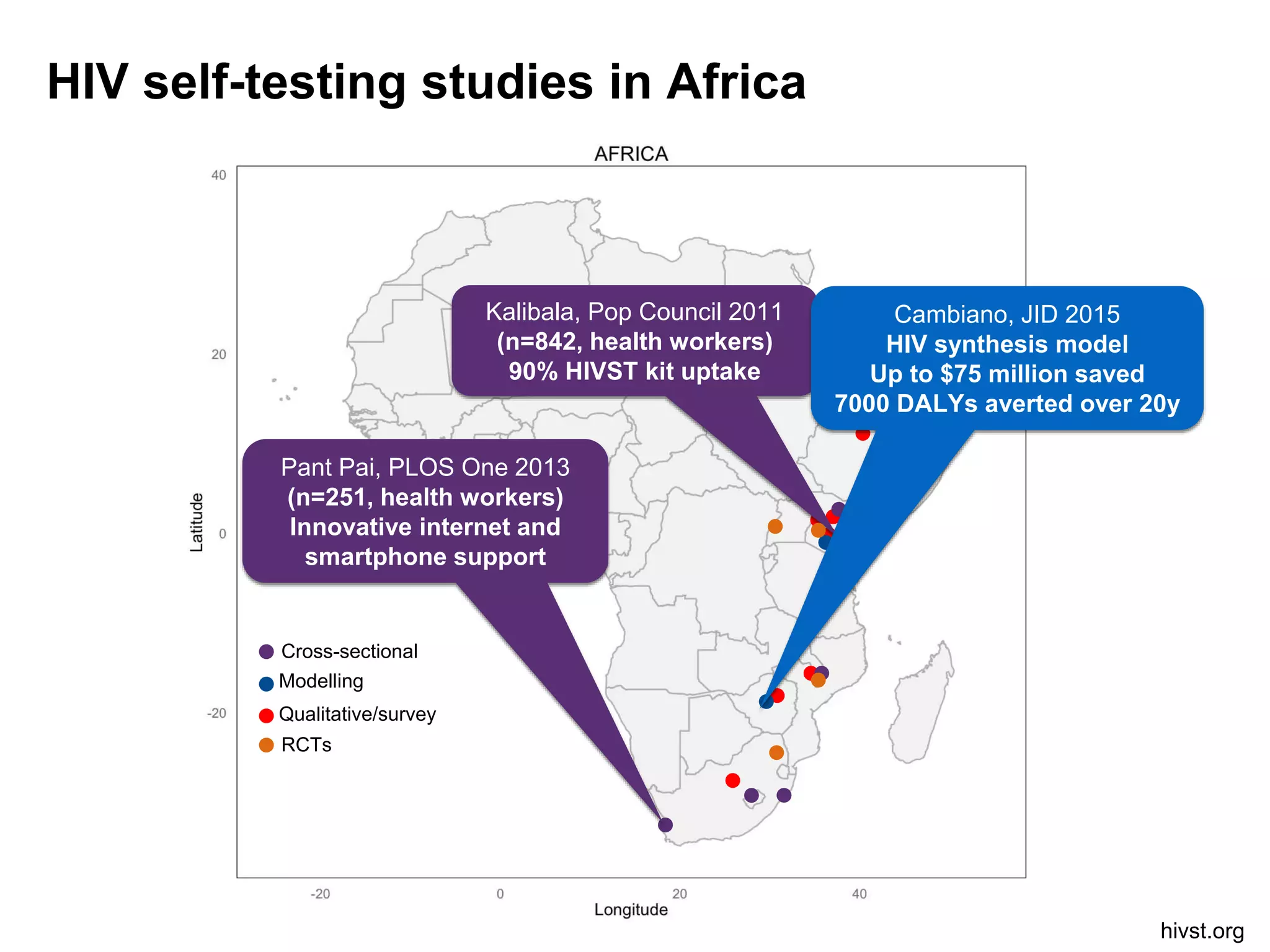
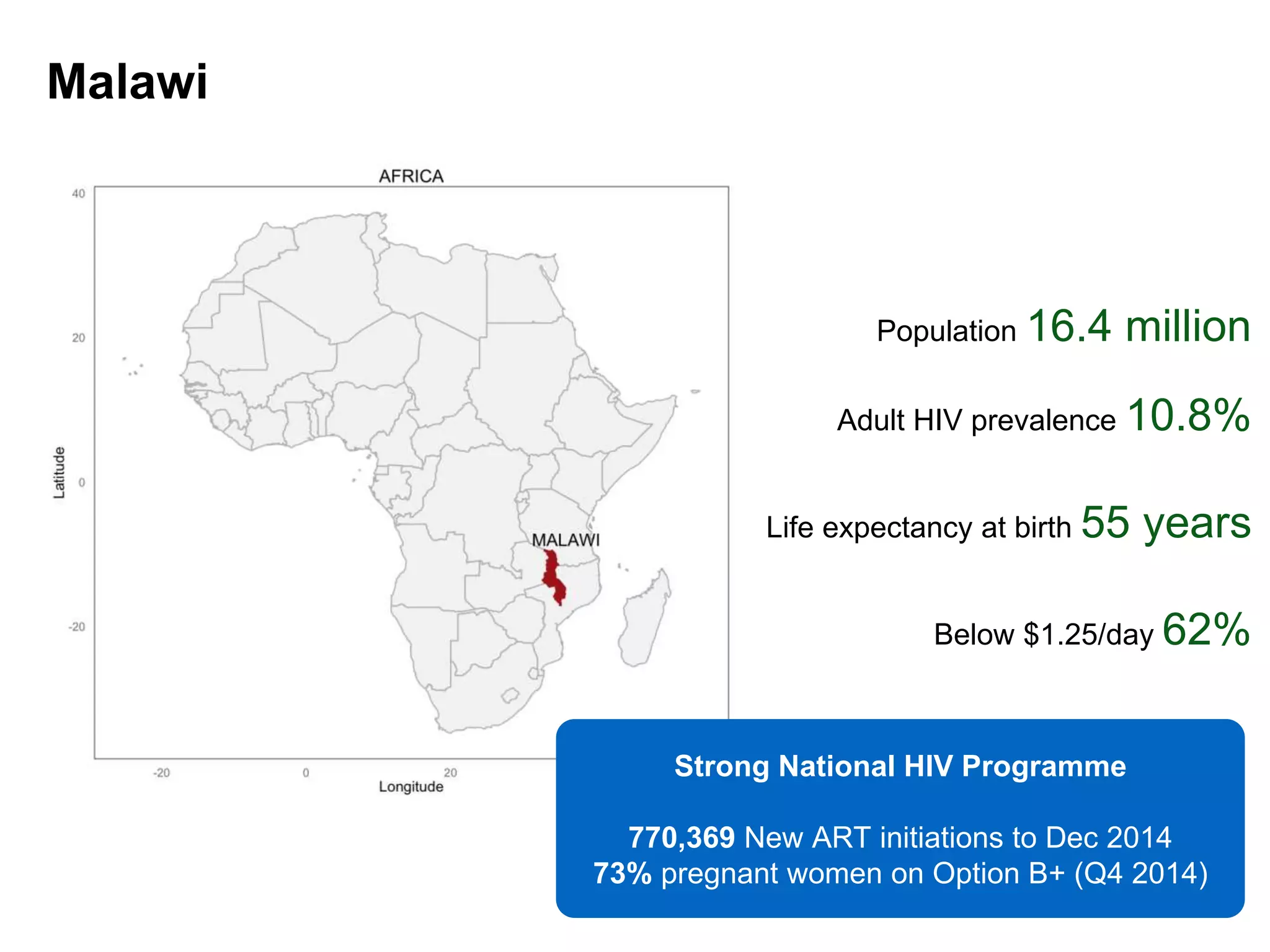
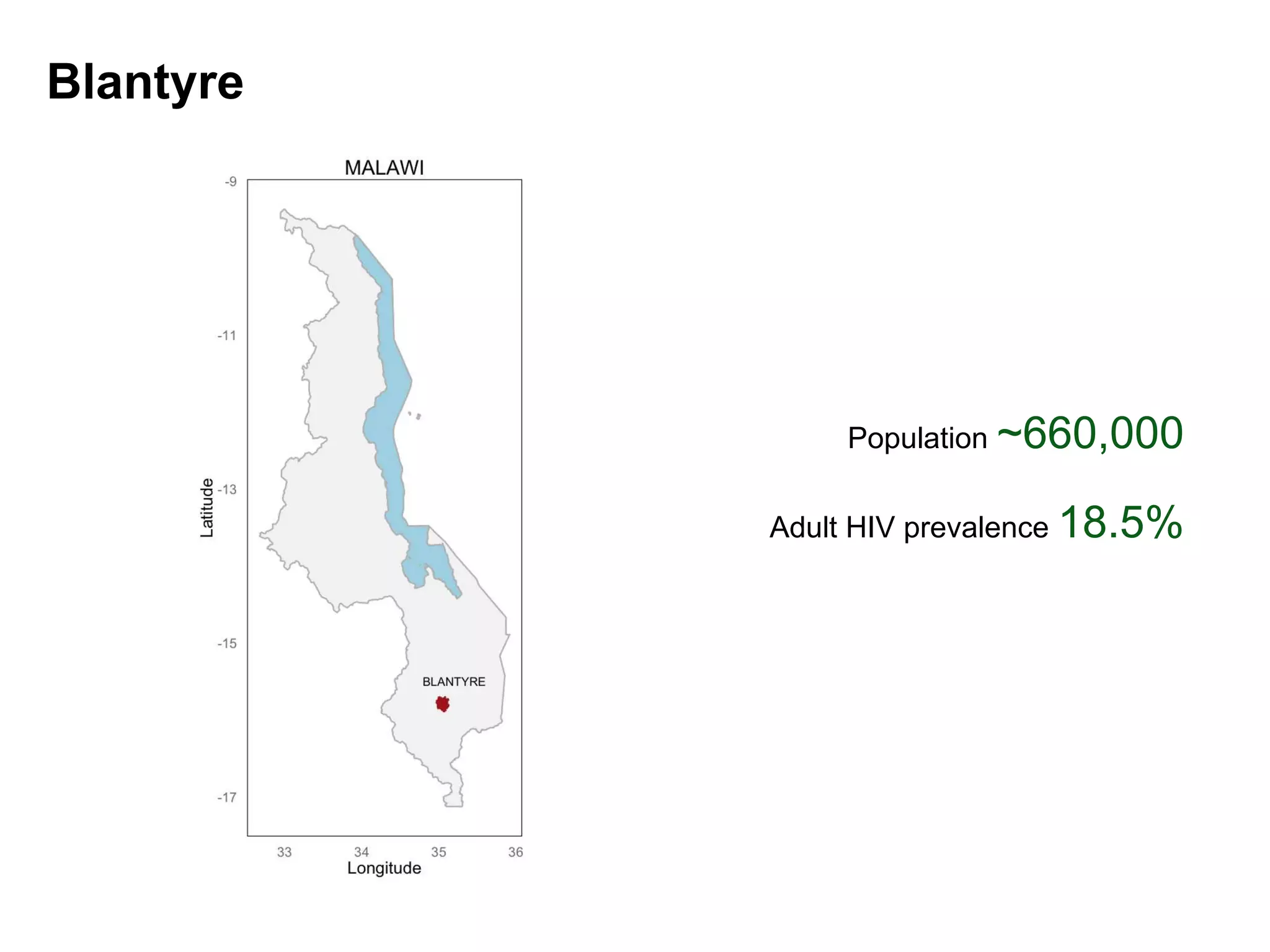
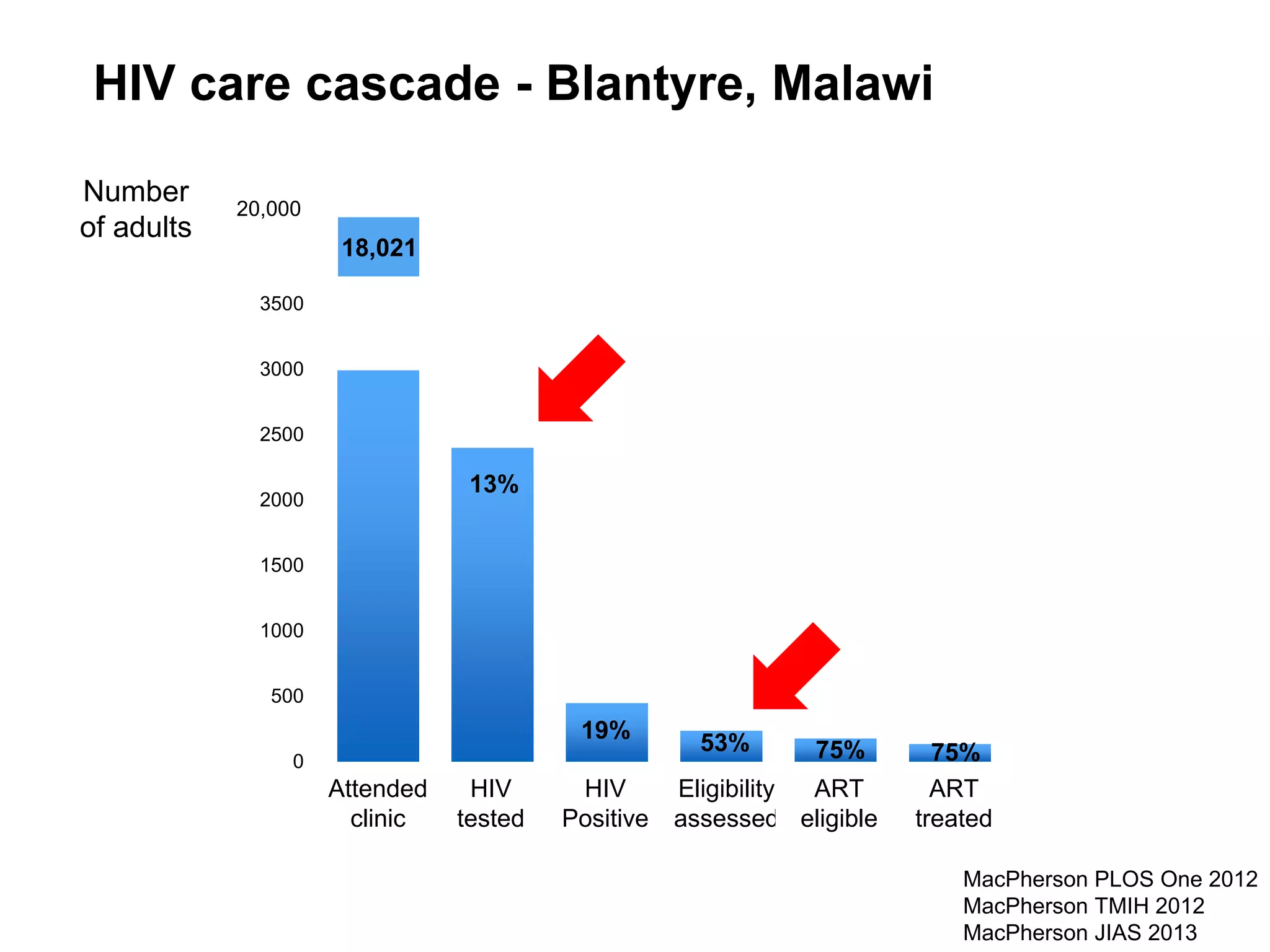
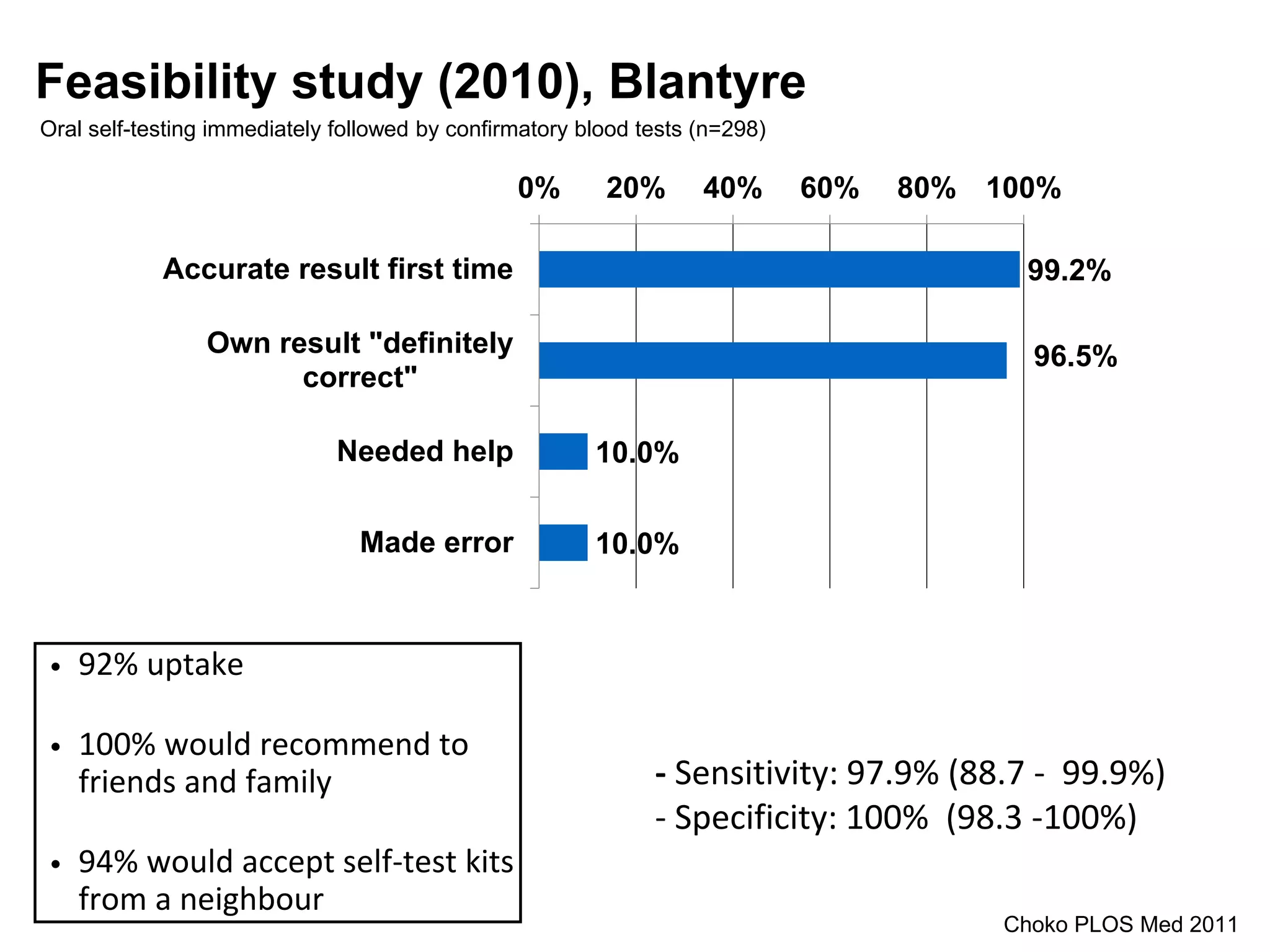
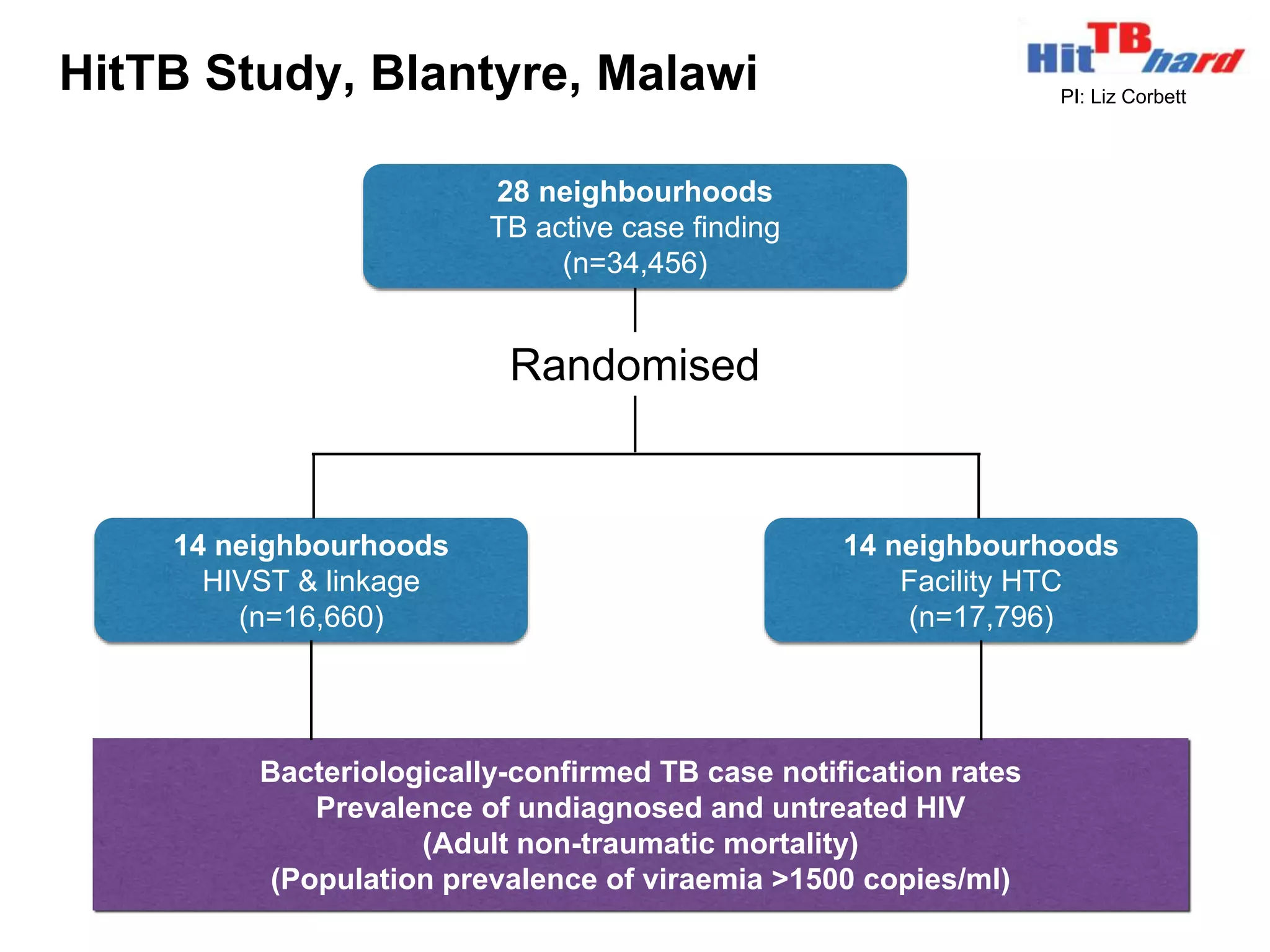
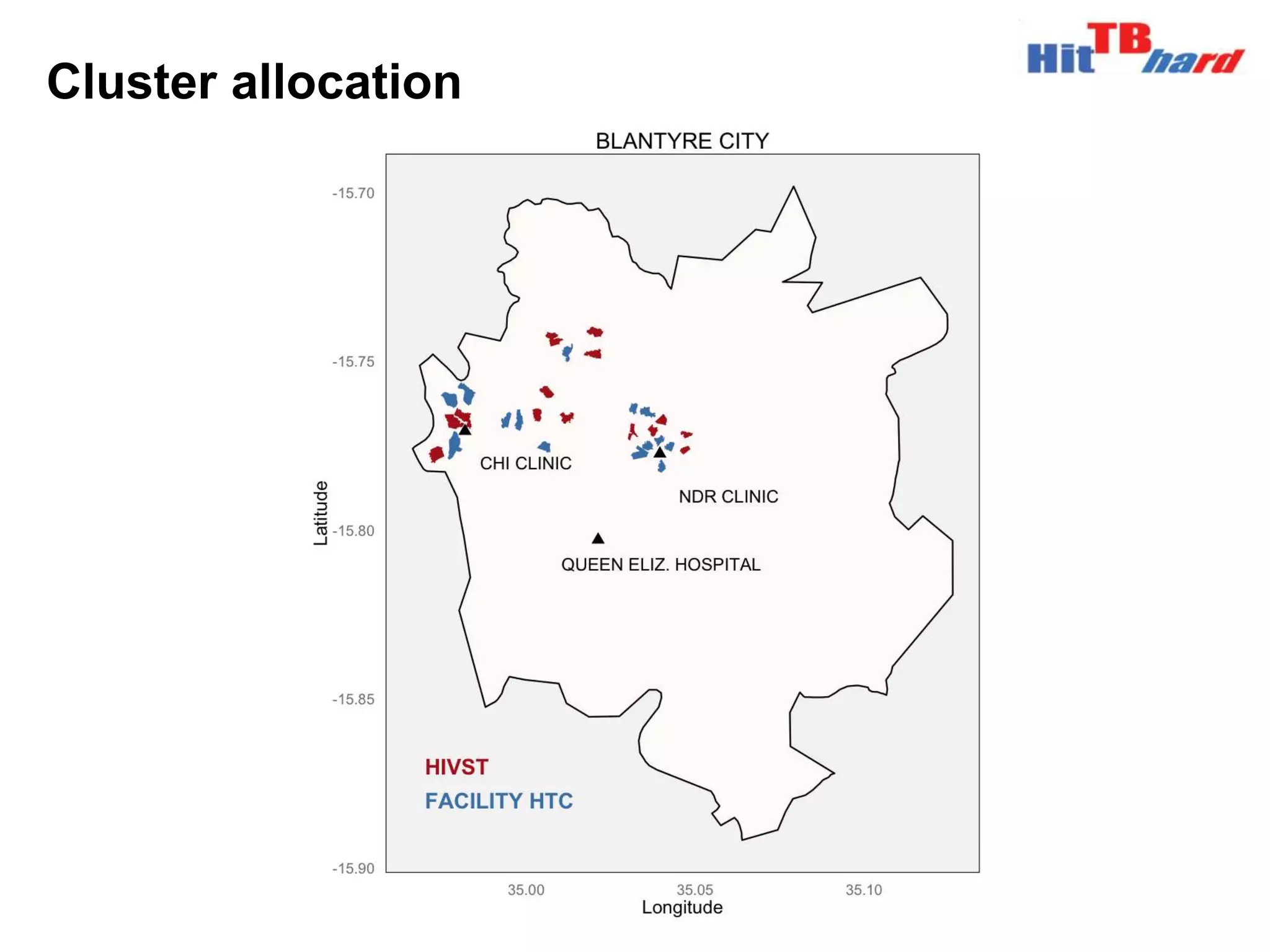
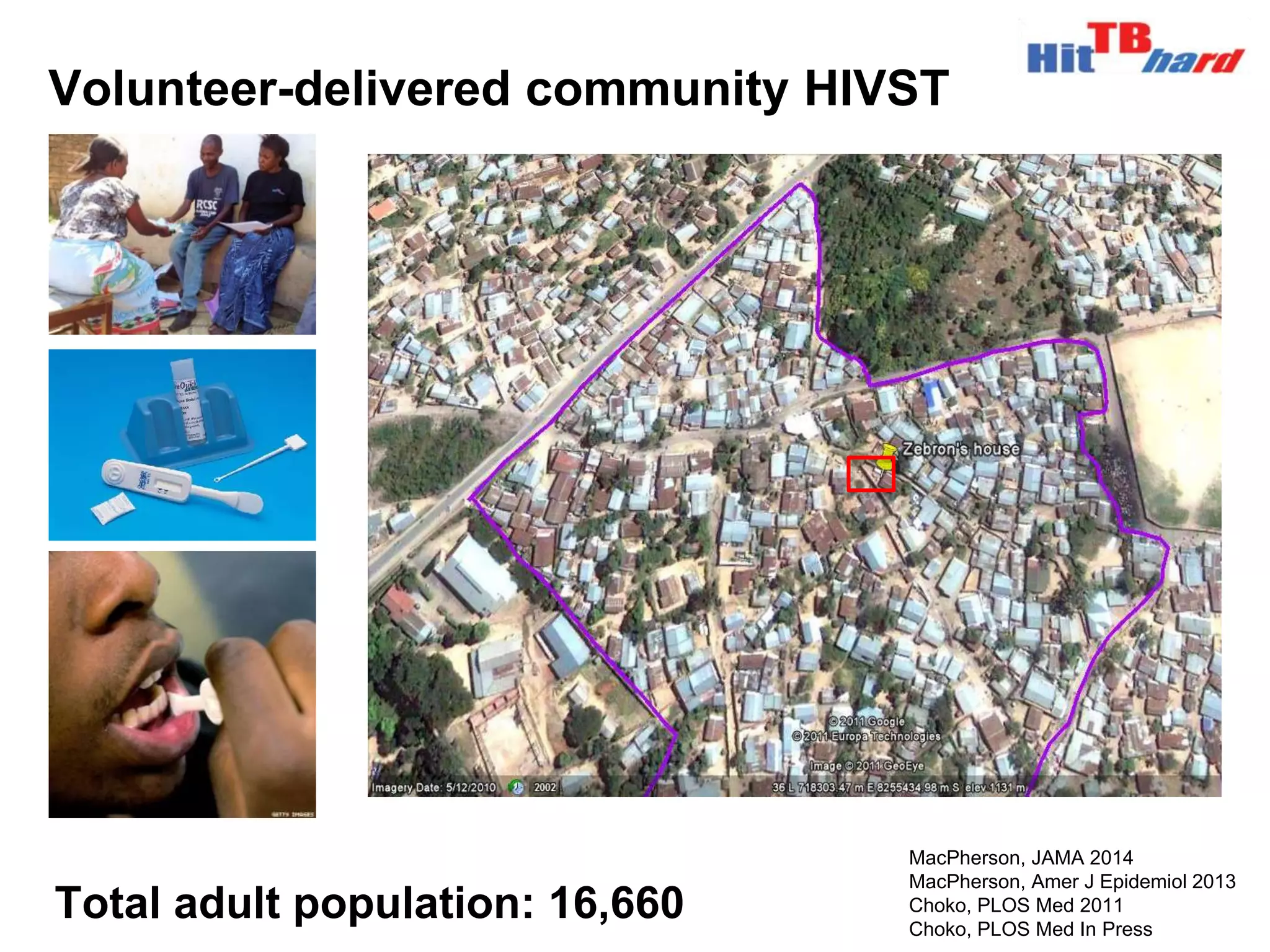
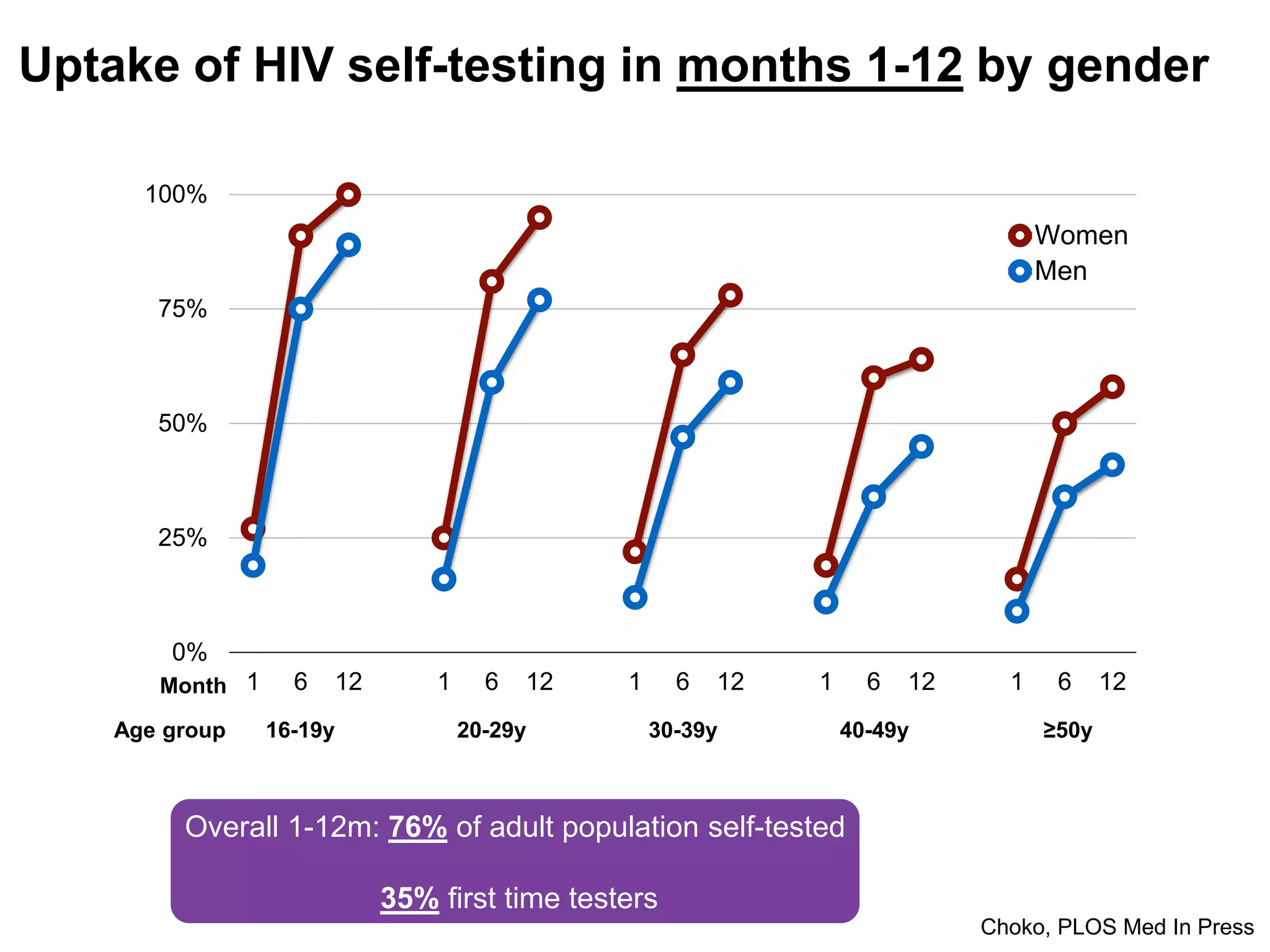
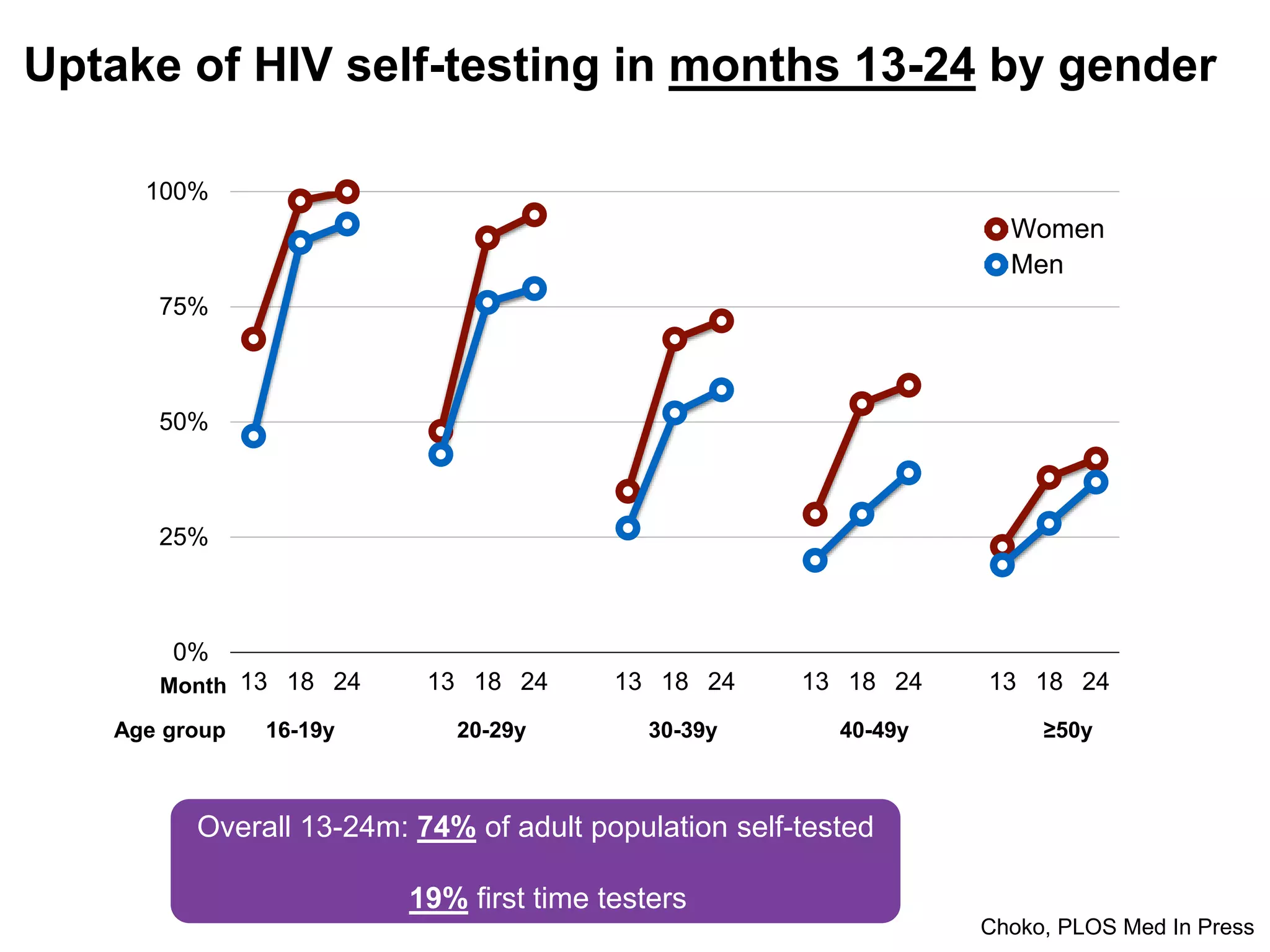
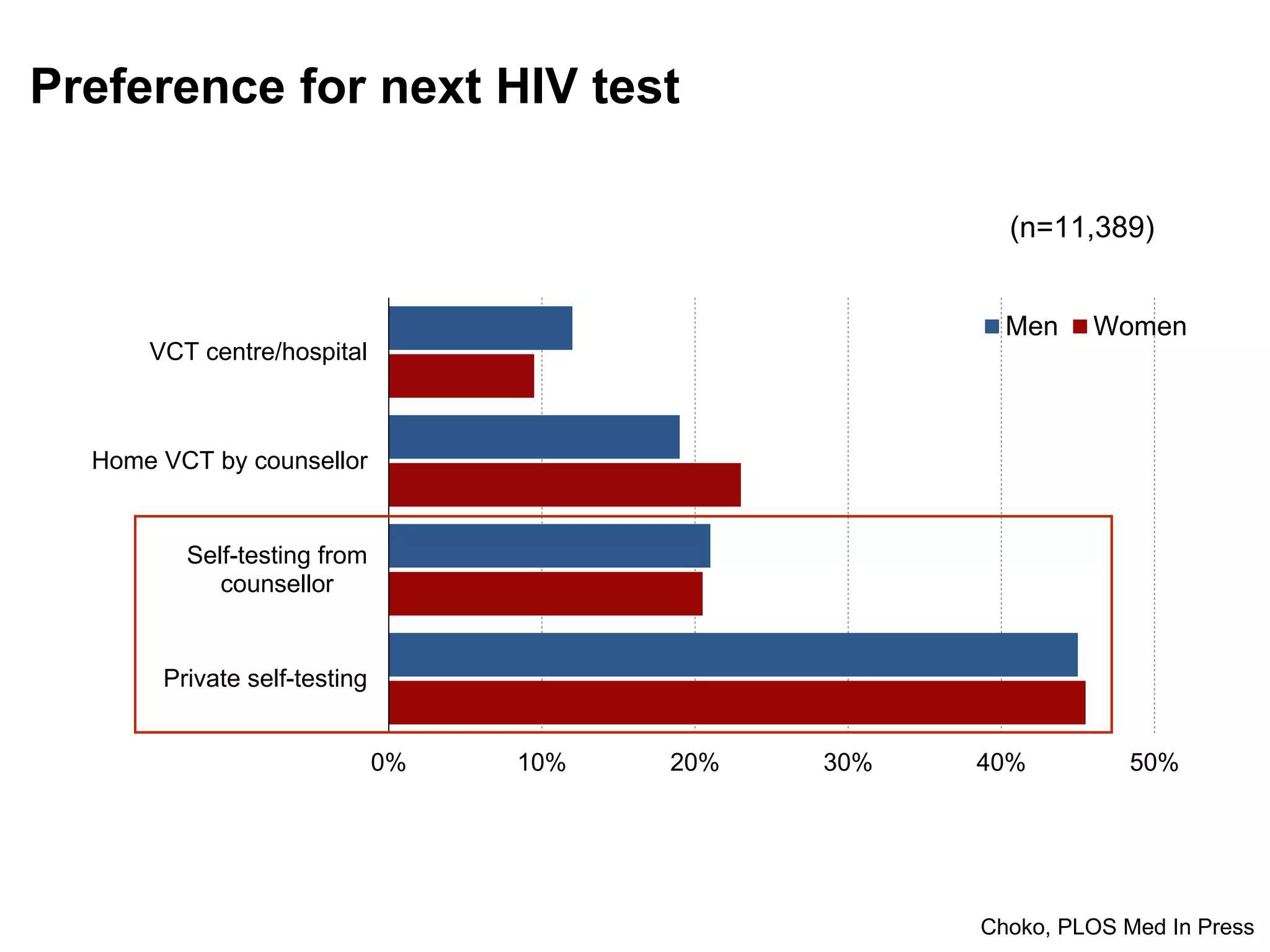
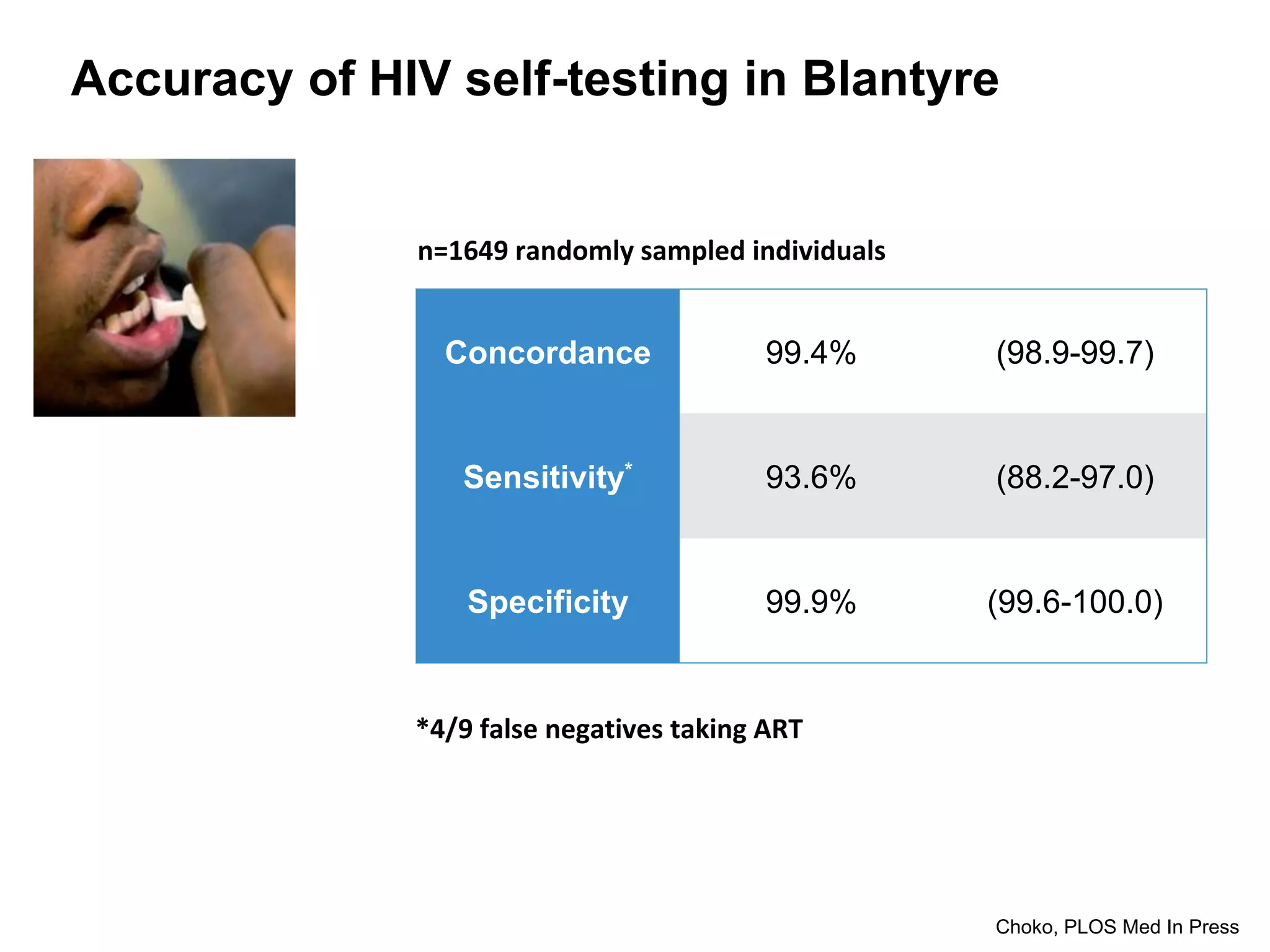
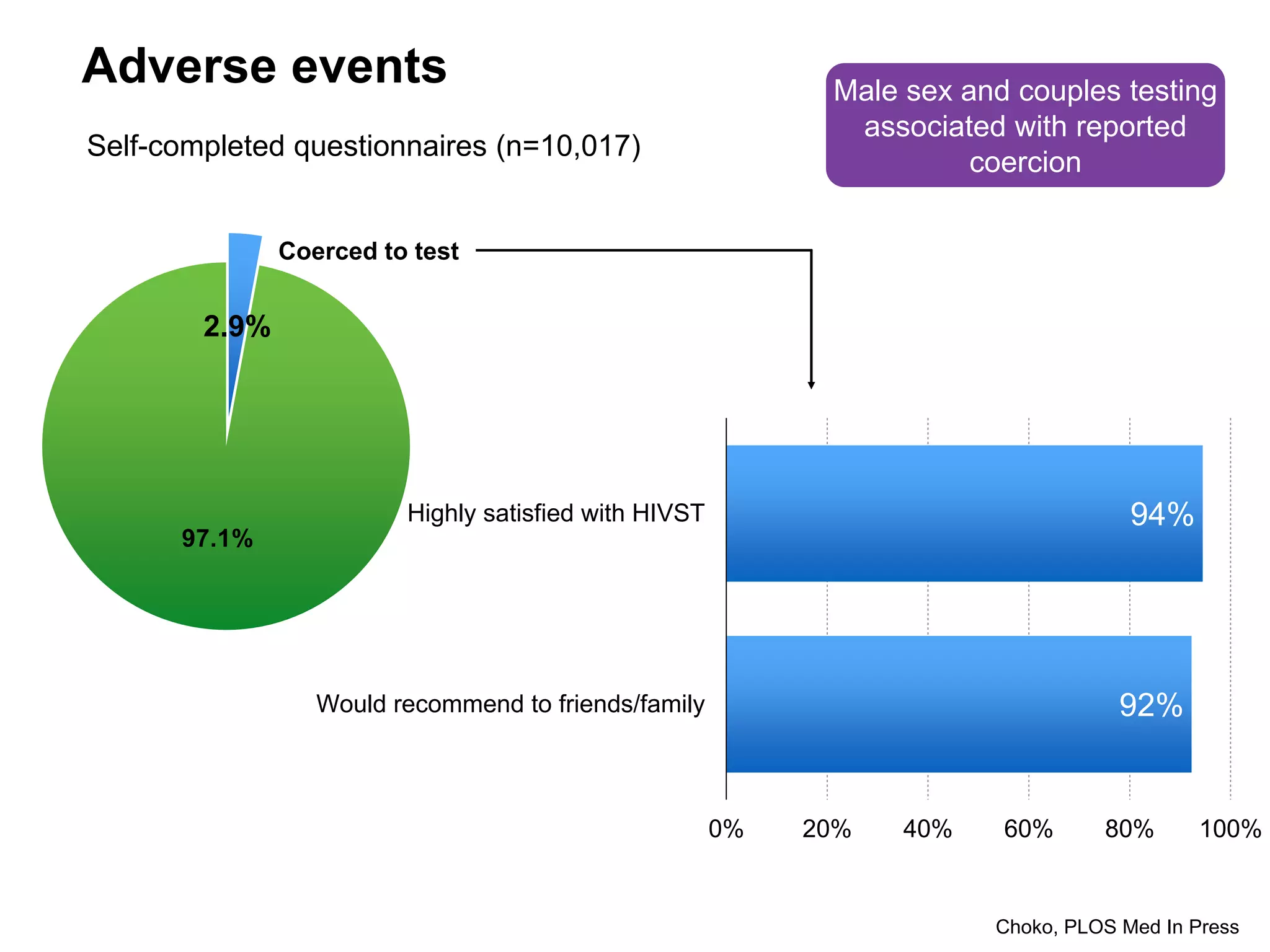
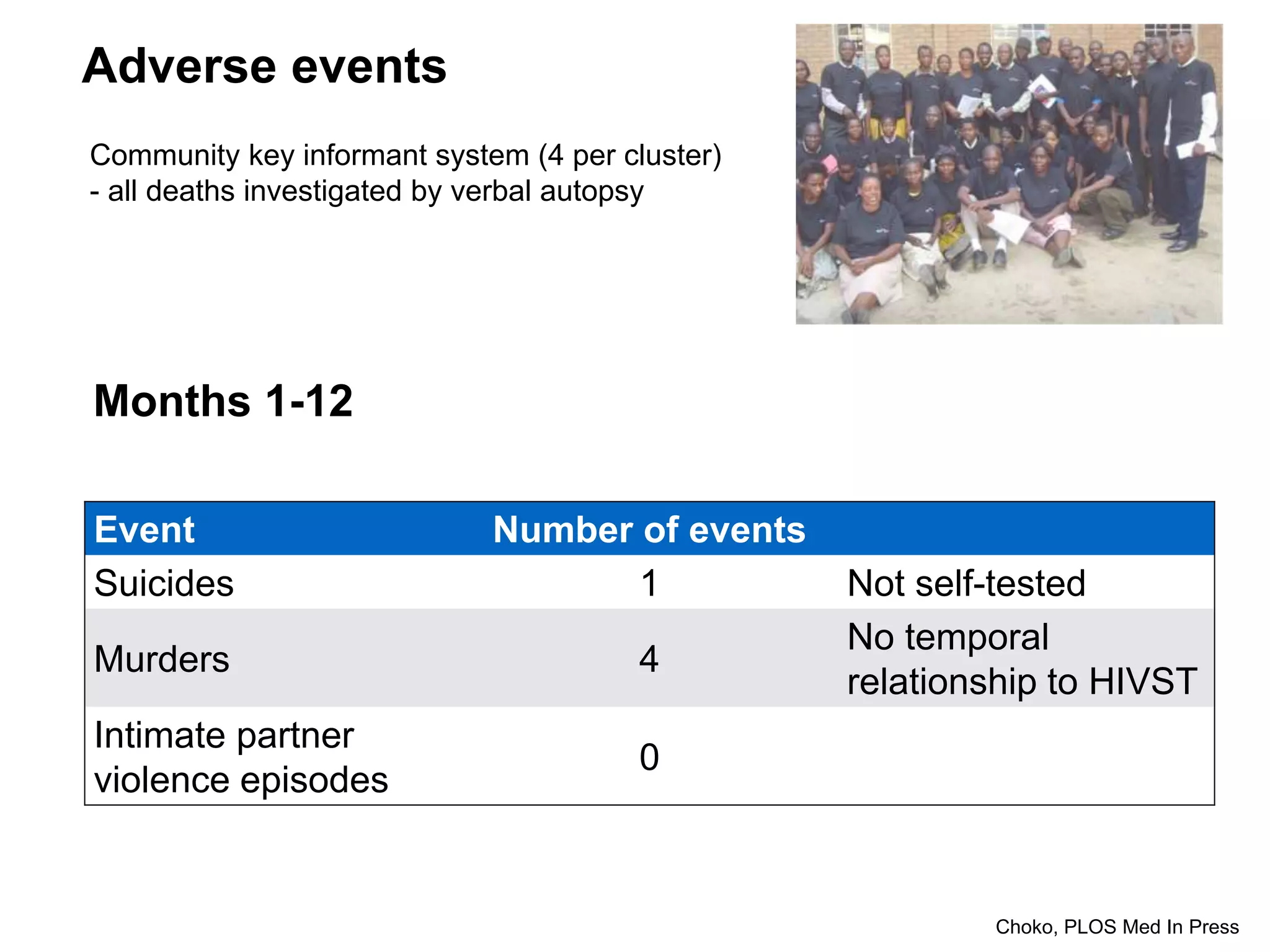
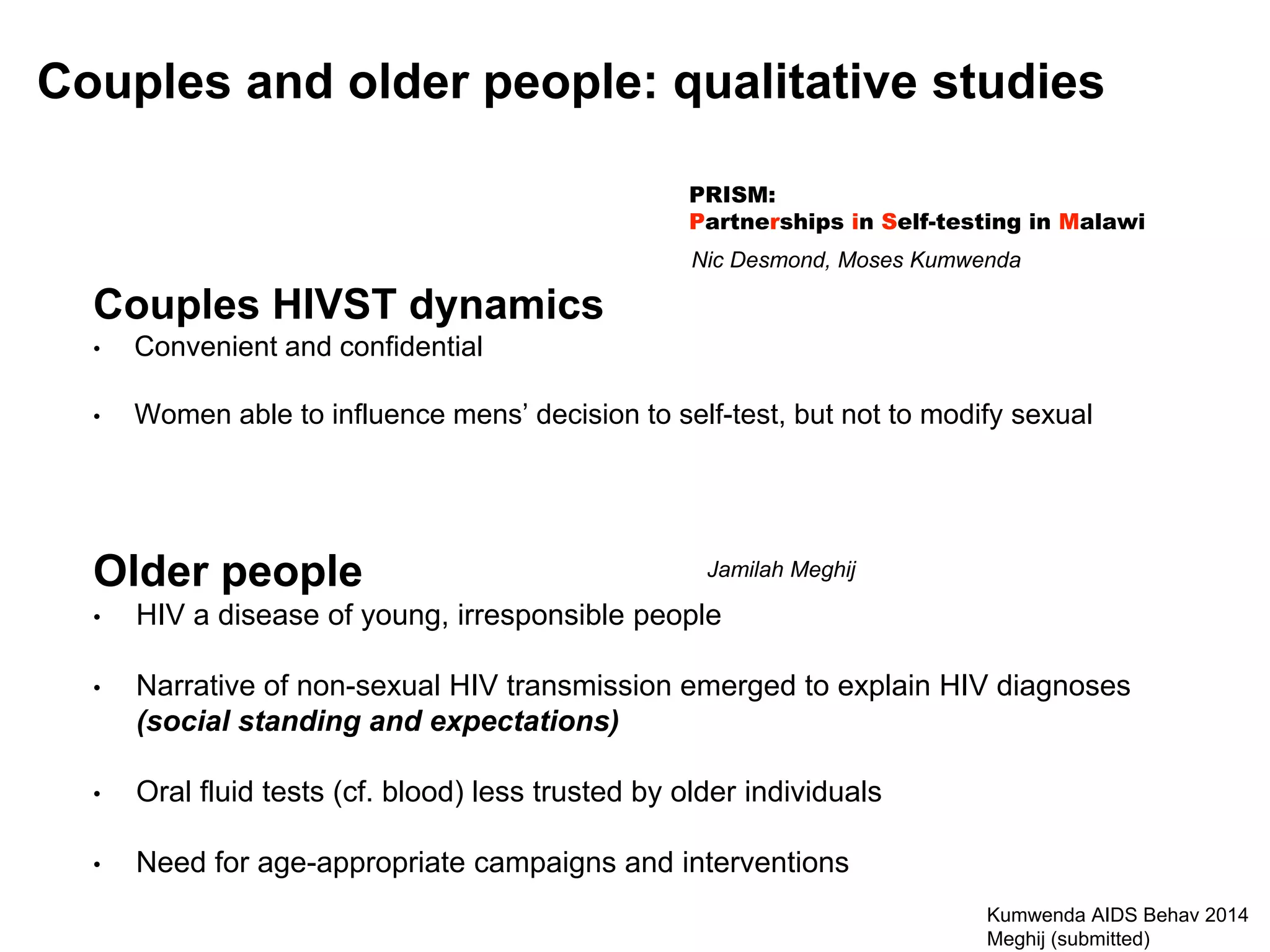
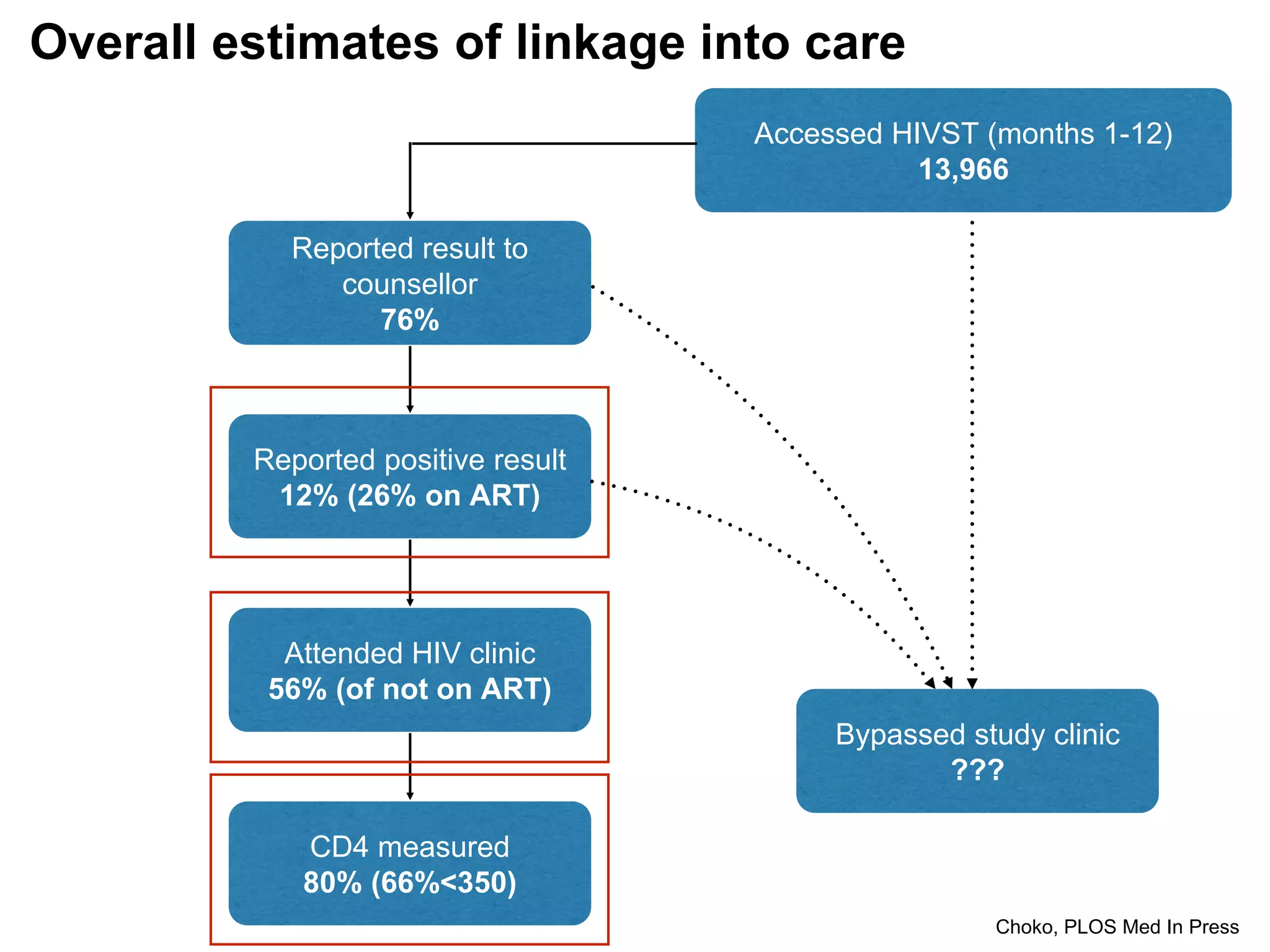
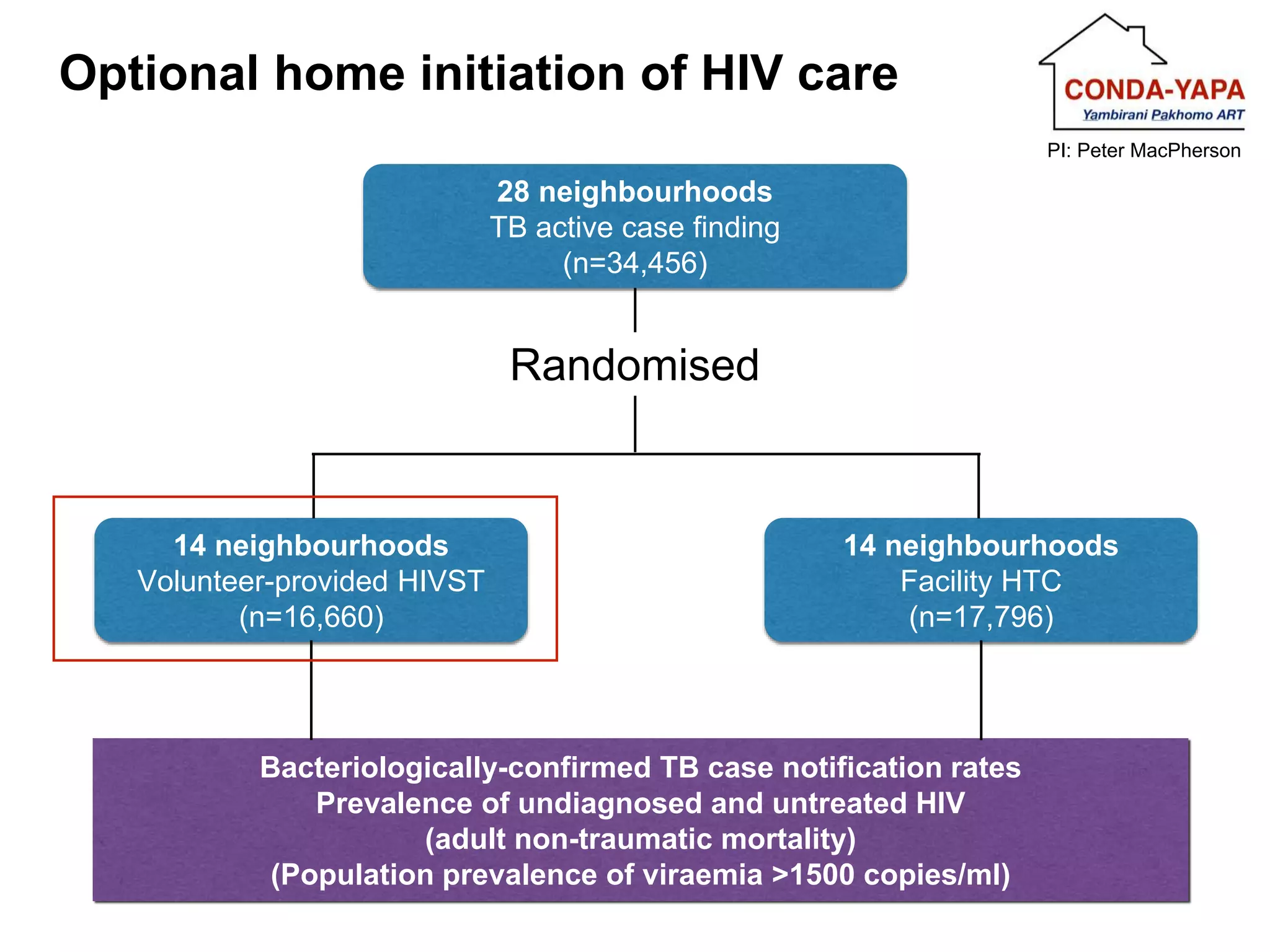
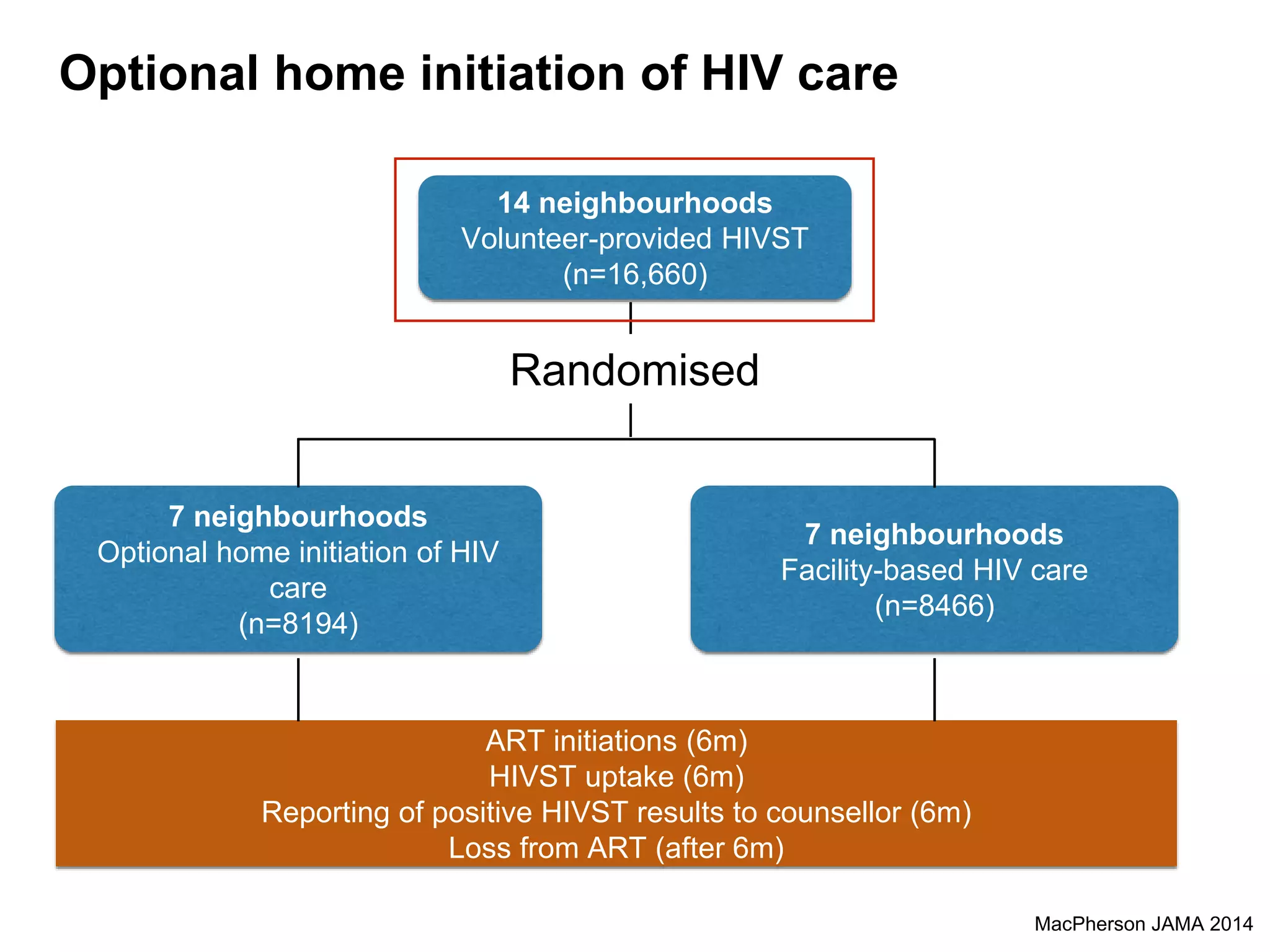
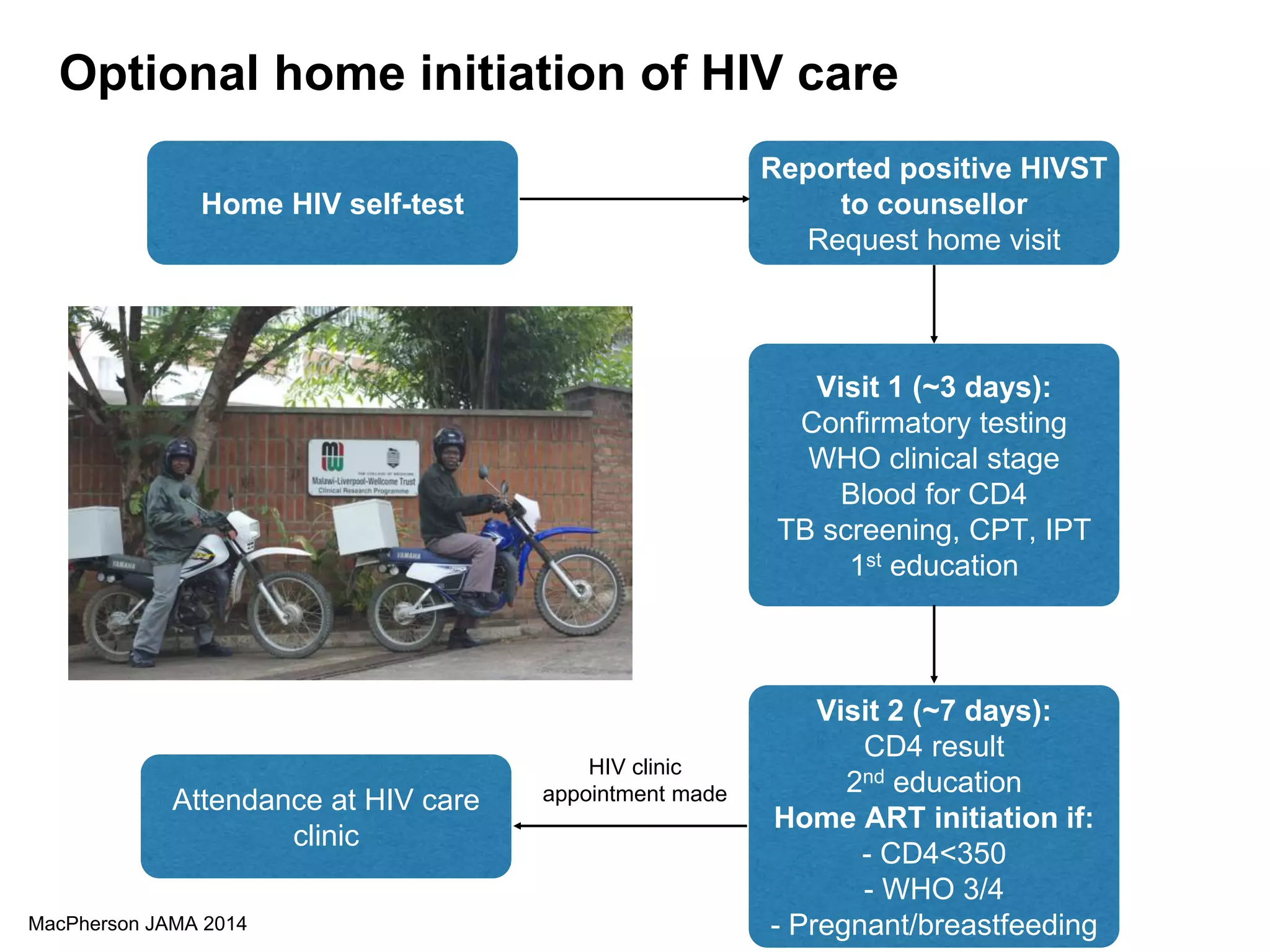
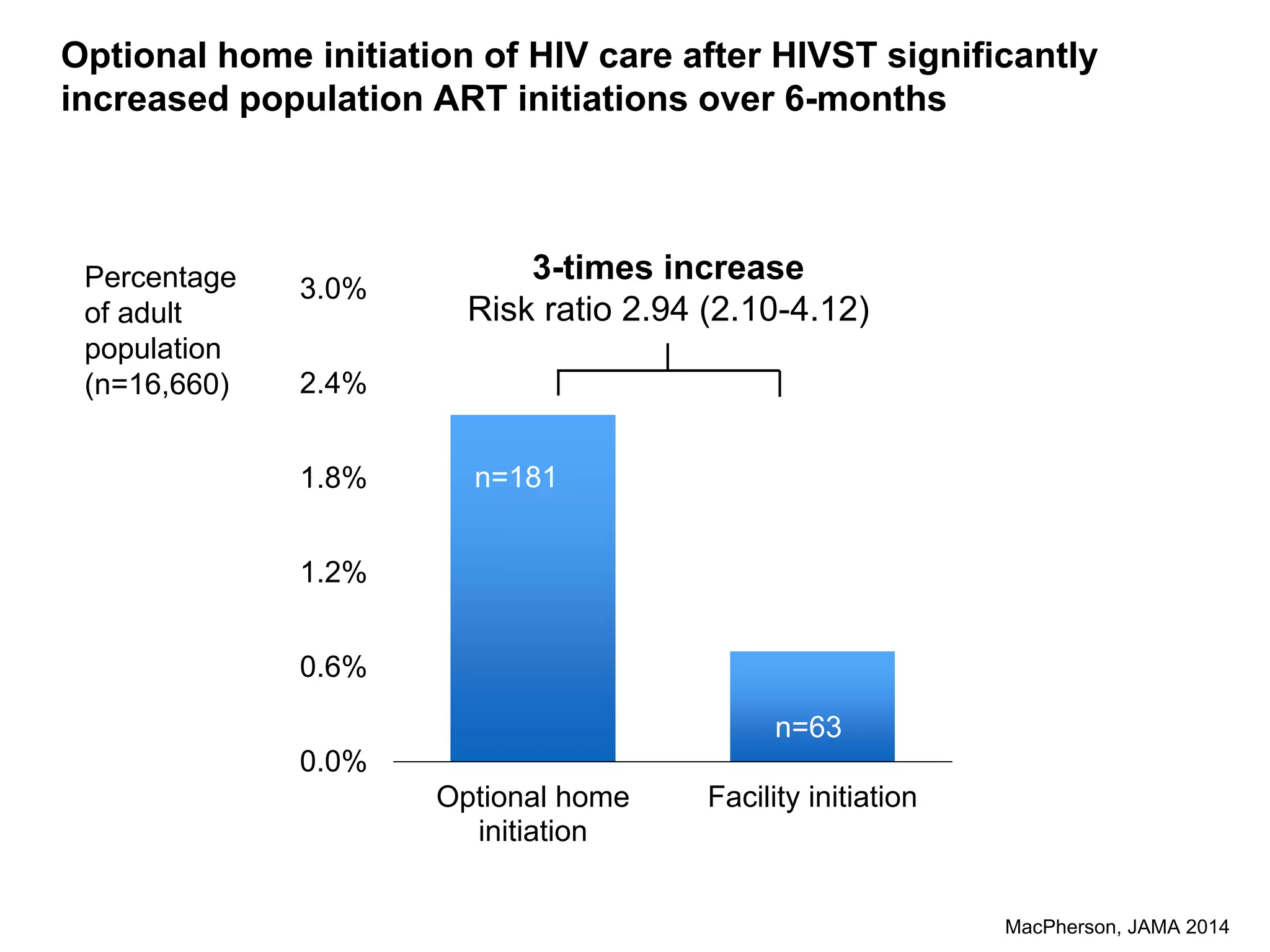
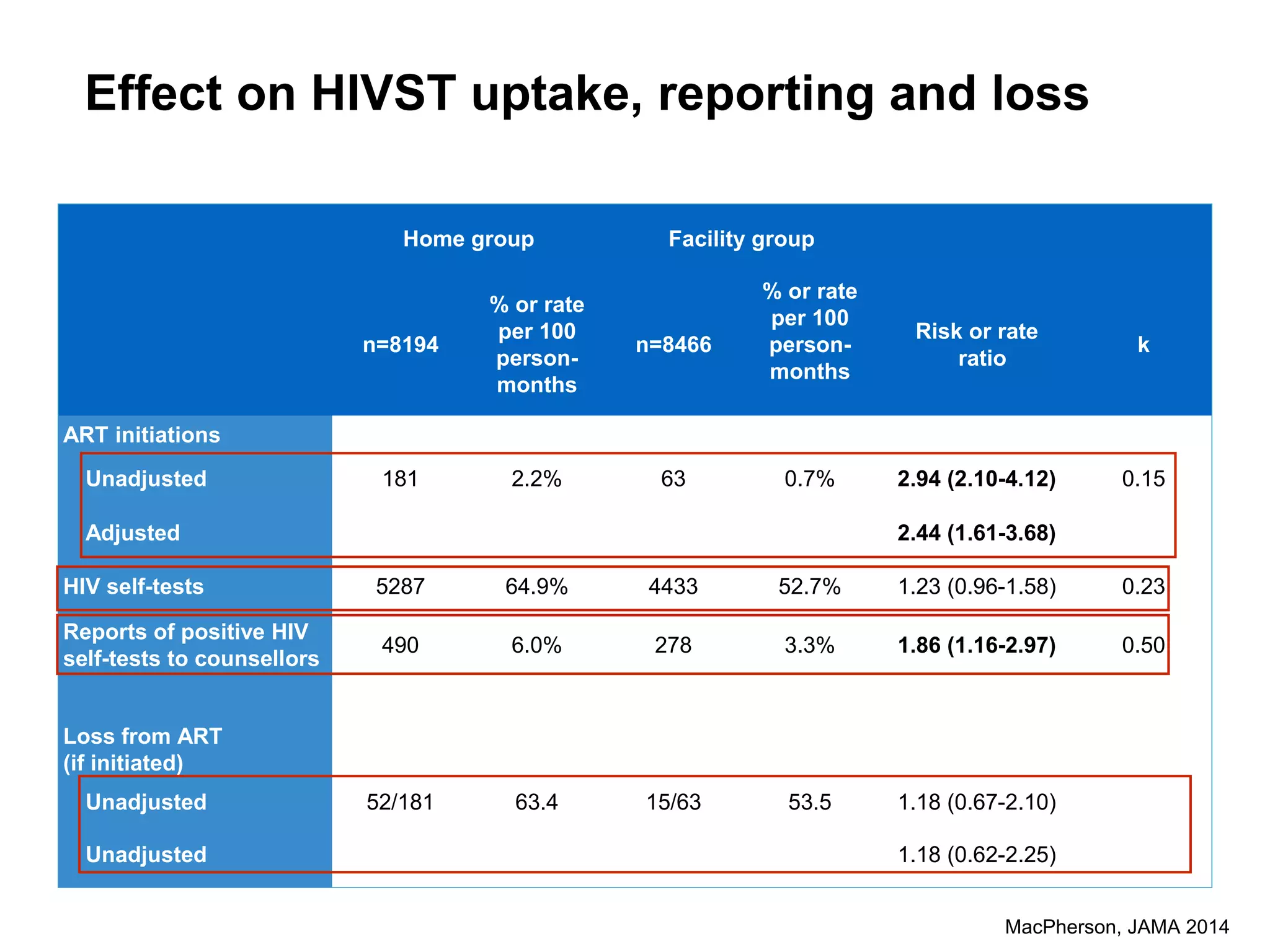
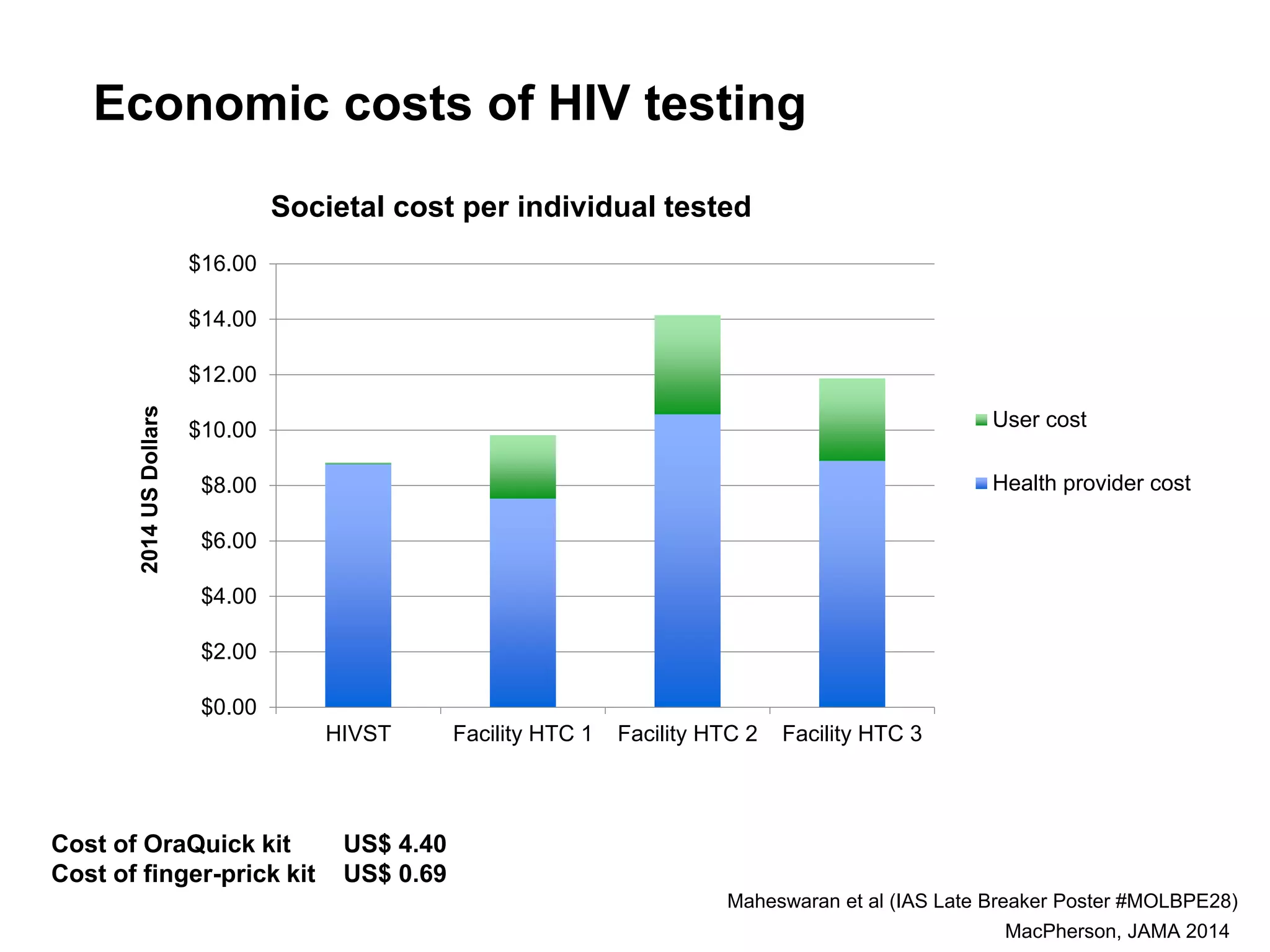
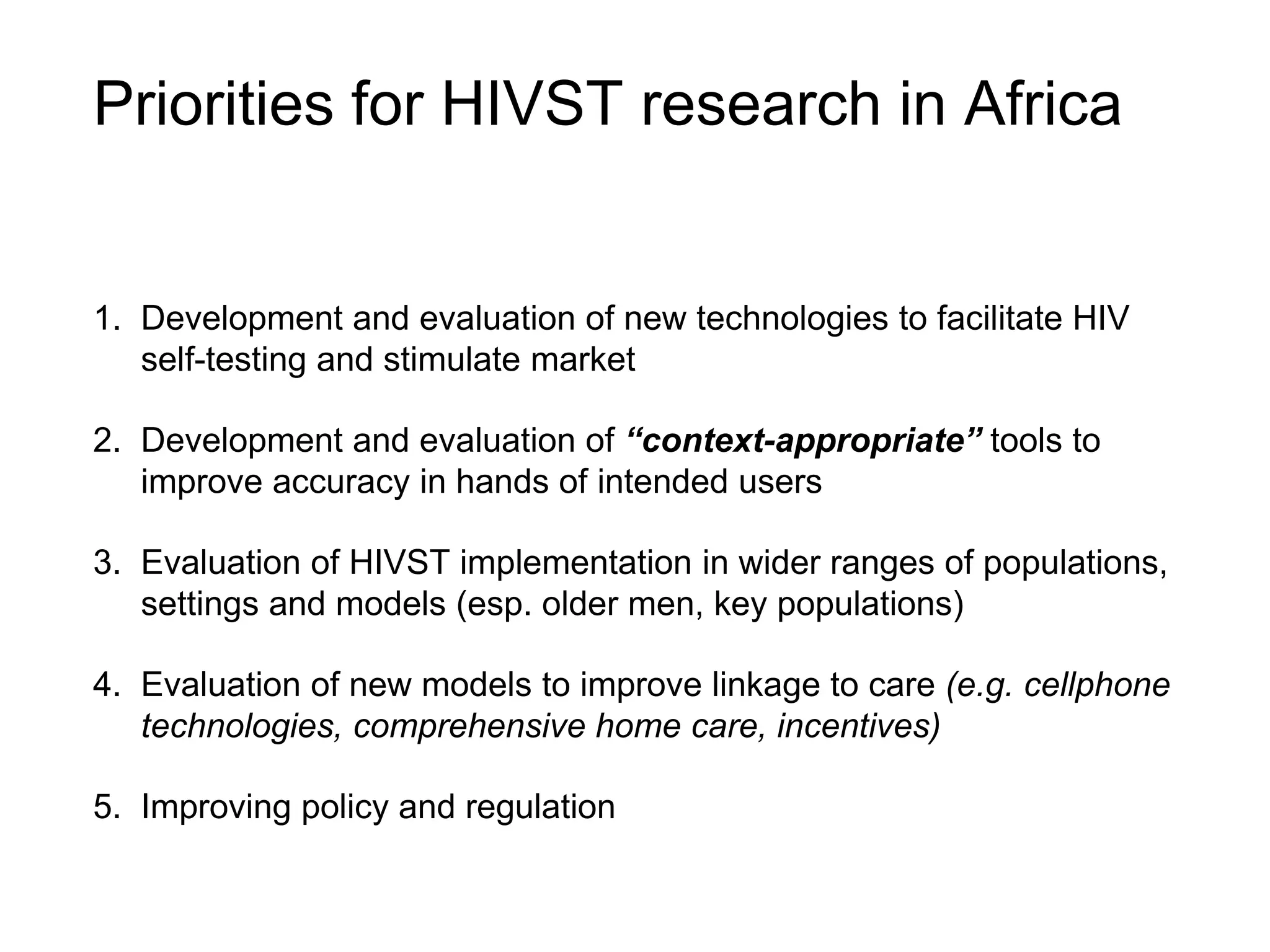
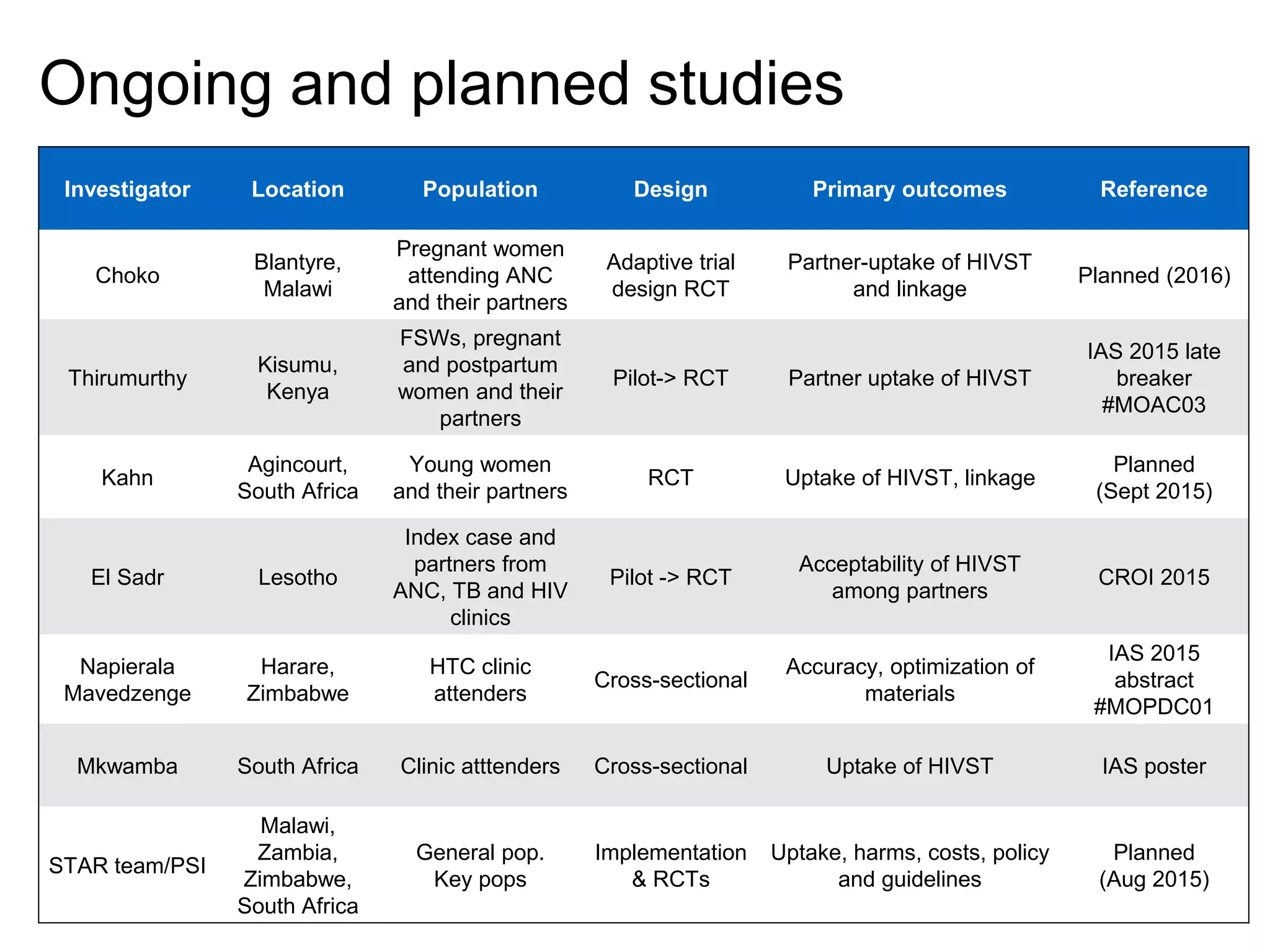
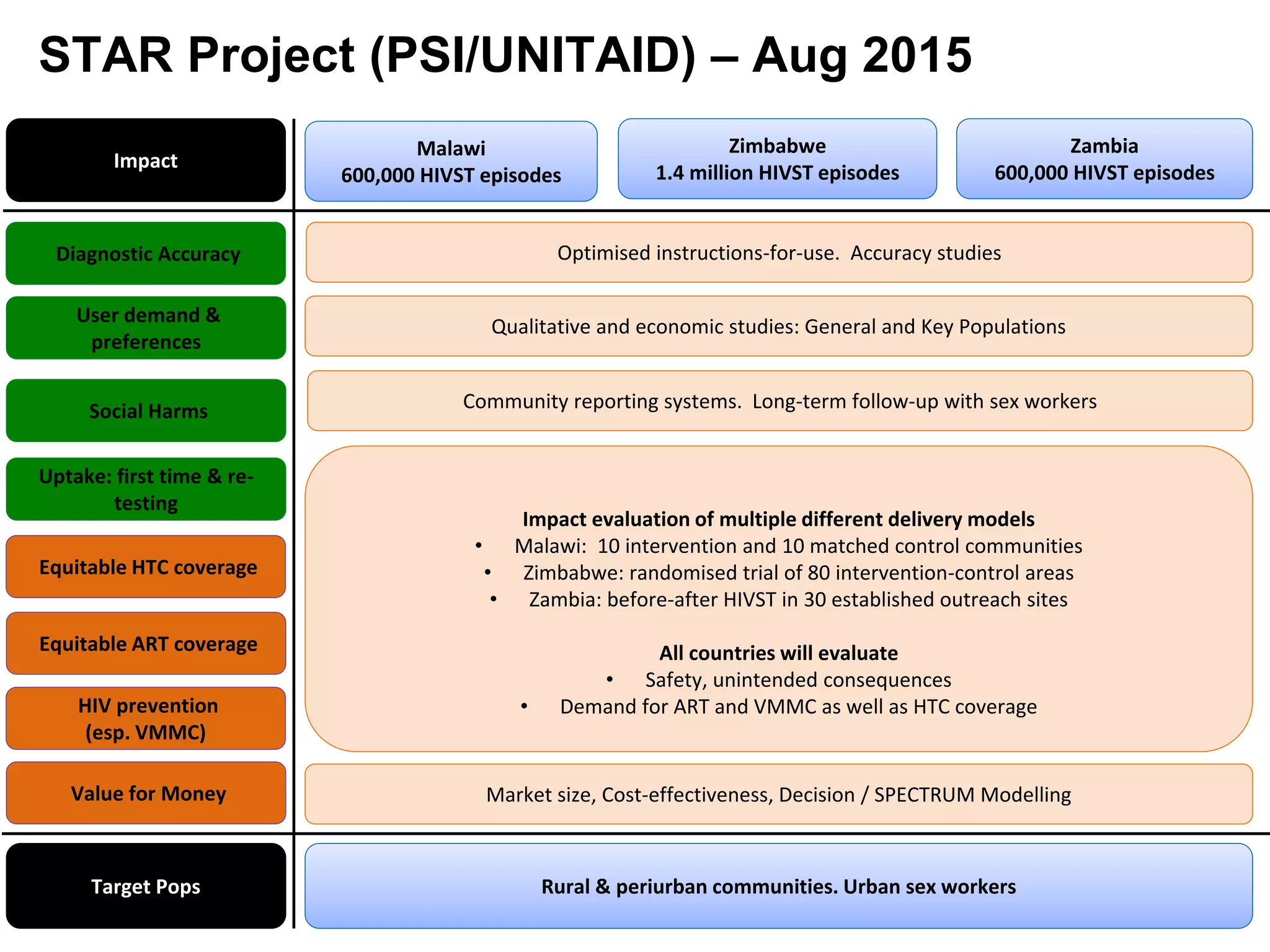
HIV self-testing and linkage in Africa. The document summarizes a presentation on HIV self-testing research in Africa. It discusses (1) the need for HIV self-testing in Africa due to low testing rates and knowledge of HIV status, (2) completed and ongoing studies of HIV self-testing in various African countries, and (3) priorities for future research including improving accuracy, evaluating new models for linkage to care, and assessing implementation in different populations and settings.