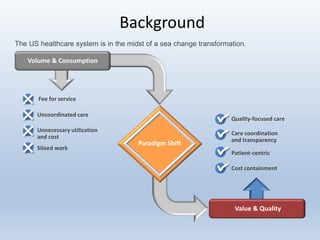
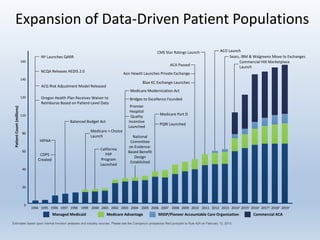
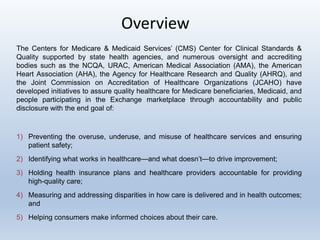
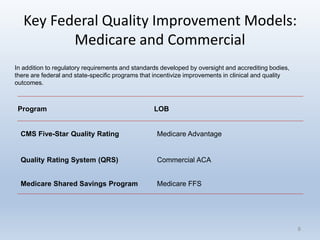
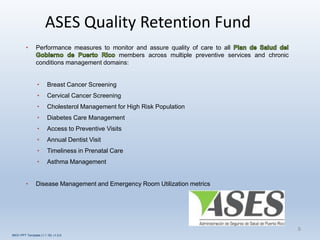
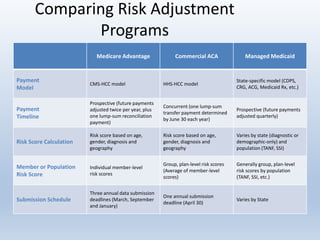
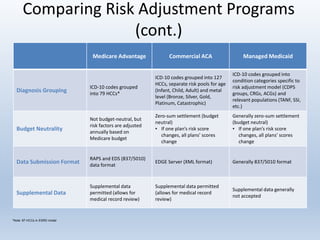
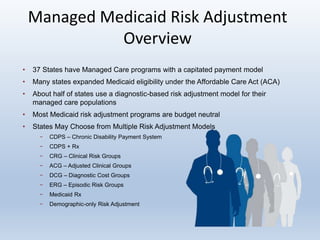
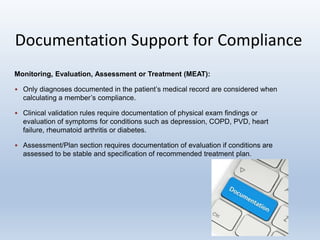
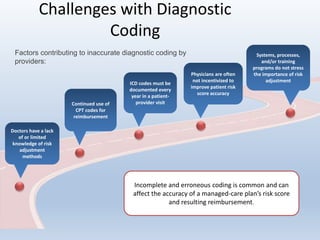
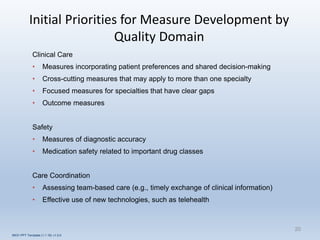
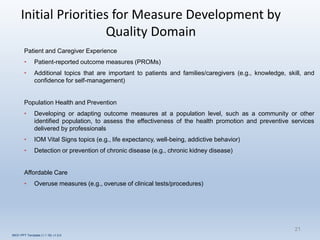
This document provides an overview and summary of quality in healthcare initiatives. It discusses the industry background and shift towards quality and value-based care. It outlines key federal quality programs like CMS Star Ratings and accrediting entities like NCQA. It also summarizes Puerto Rico's quality retention fund and examples of clinical quality measures like breast cancer screening and diabetes management. Finally, it reviews risk adjustment programs in Medicare Advantage, Commercial ACA, and Managed Medicaid.