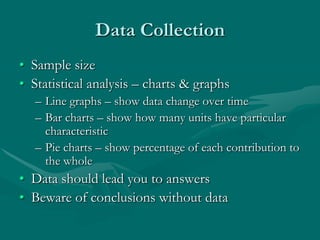
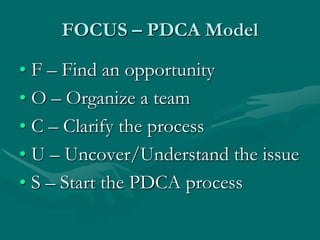
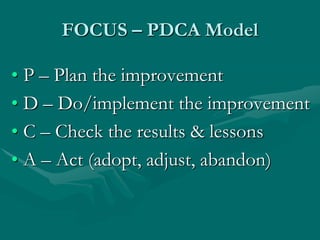
This document discusses quality management and process improvement in addiction treatment organizations. It outlines various quality improvement frameworks and explains why ongoing monitoring and evaluation is important as providers become more accountable for outcomes. The responsibilities of leadership in establishing a culture of safety, performance improvement, and outcome measurement are described. Effective quality management requires collecting and analyzing data to identify problem areas and opportunities for improvement. The PDCA (Plan-Do-Check-Act) cycle provides a model for ongoing quality improvement efforts.