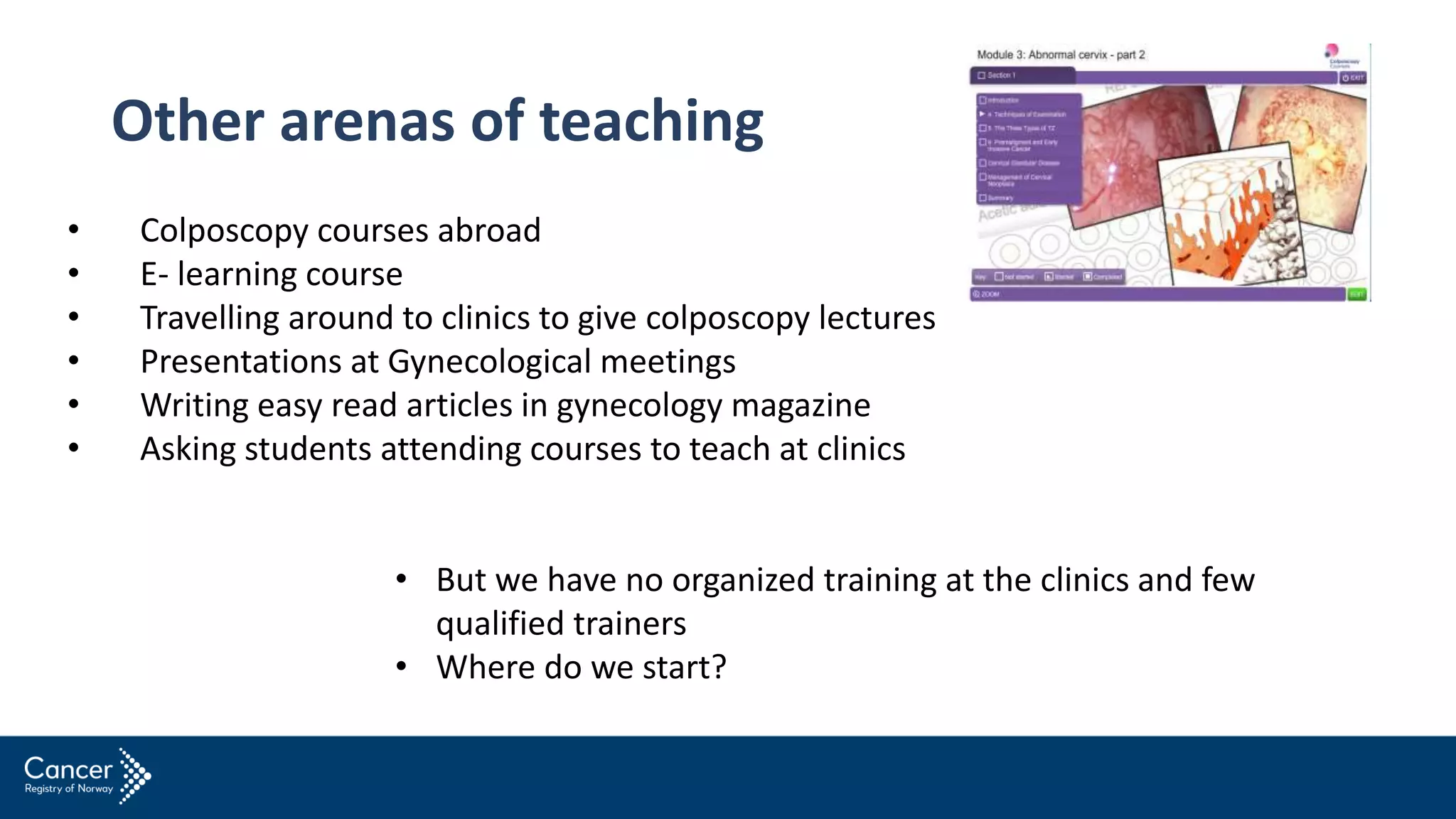
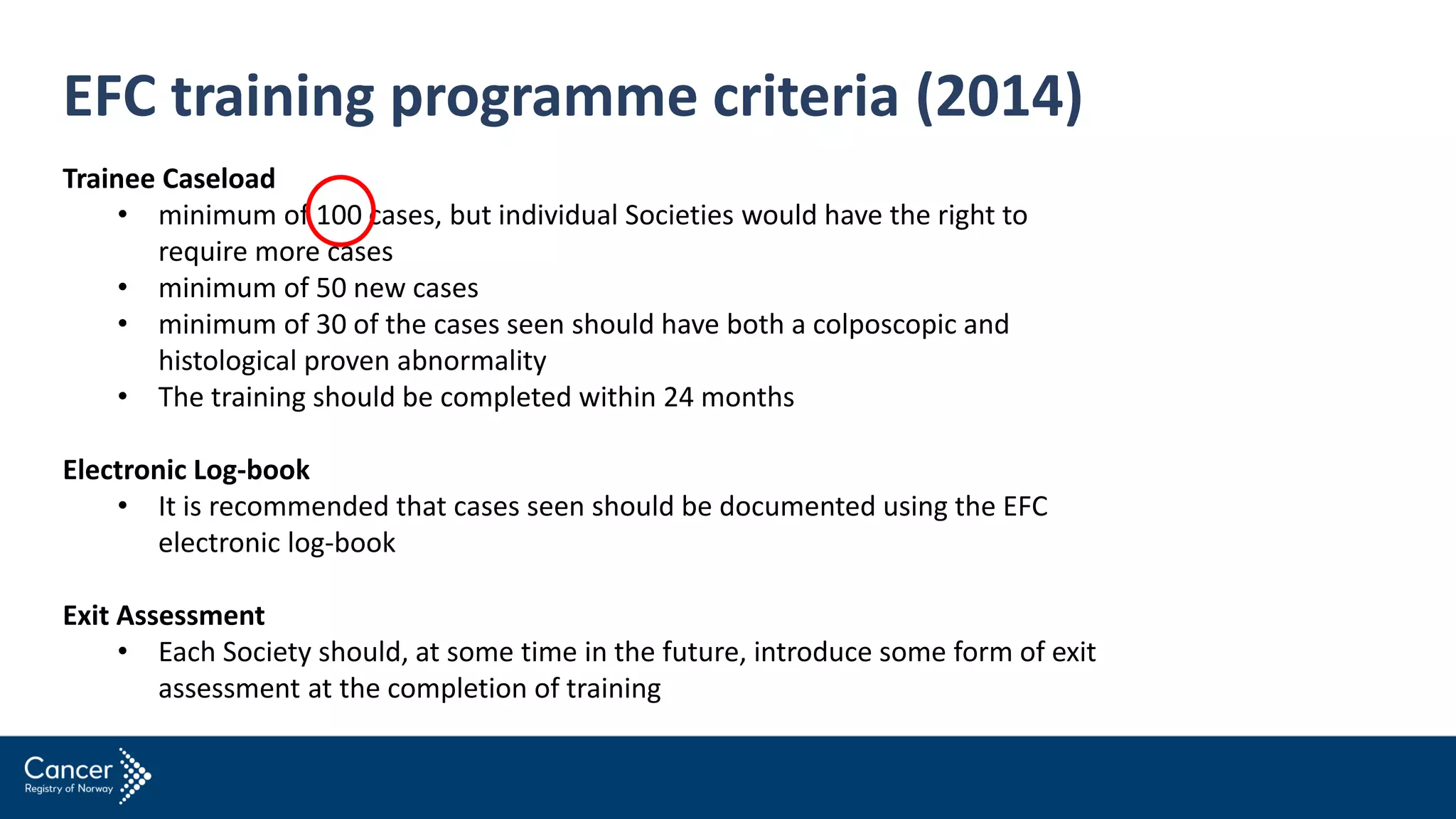
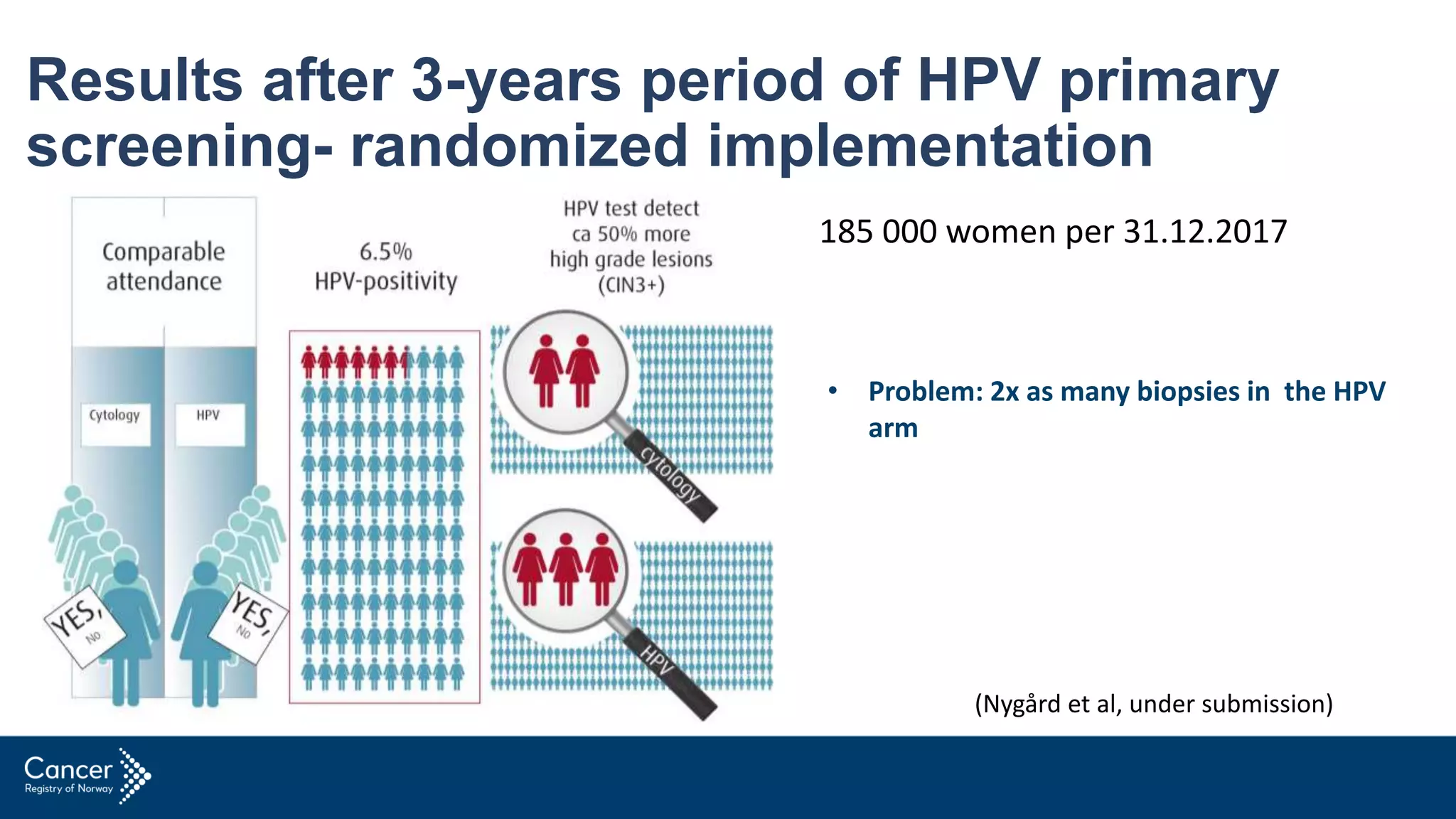
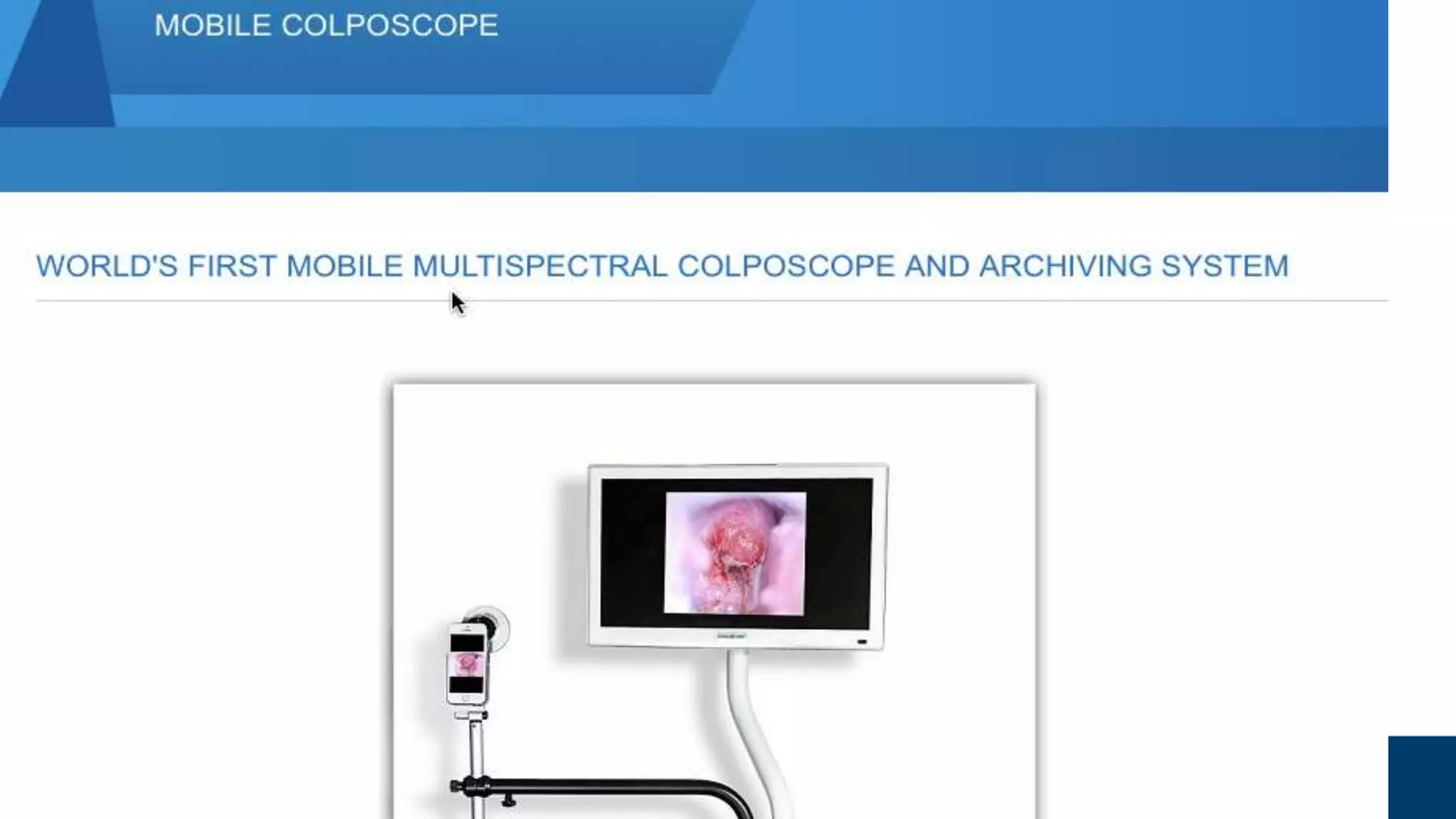
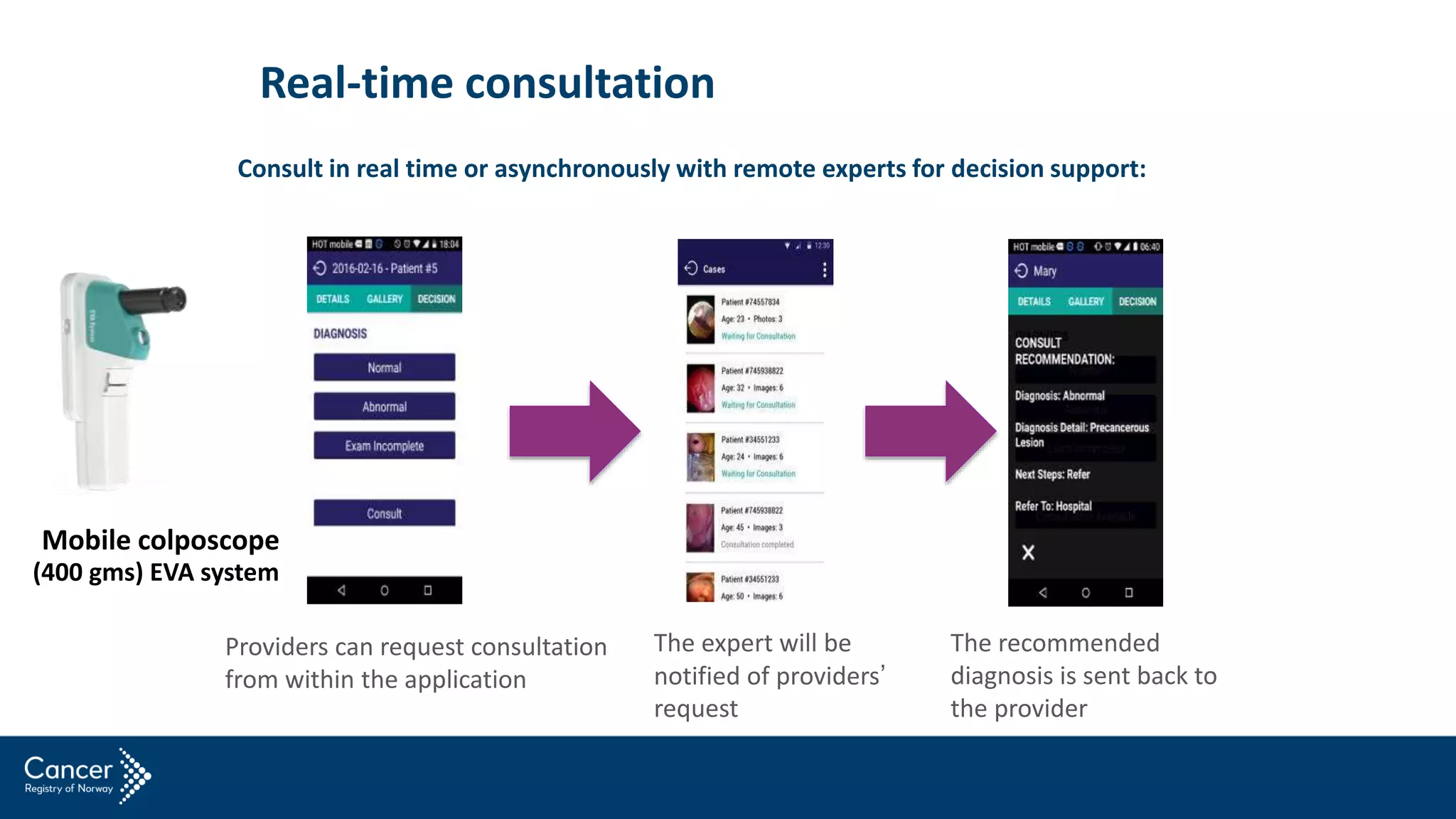
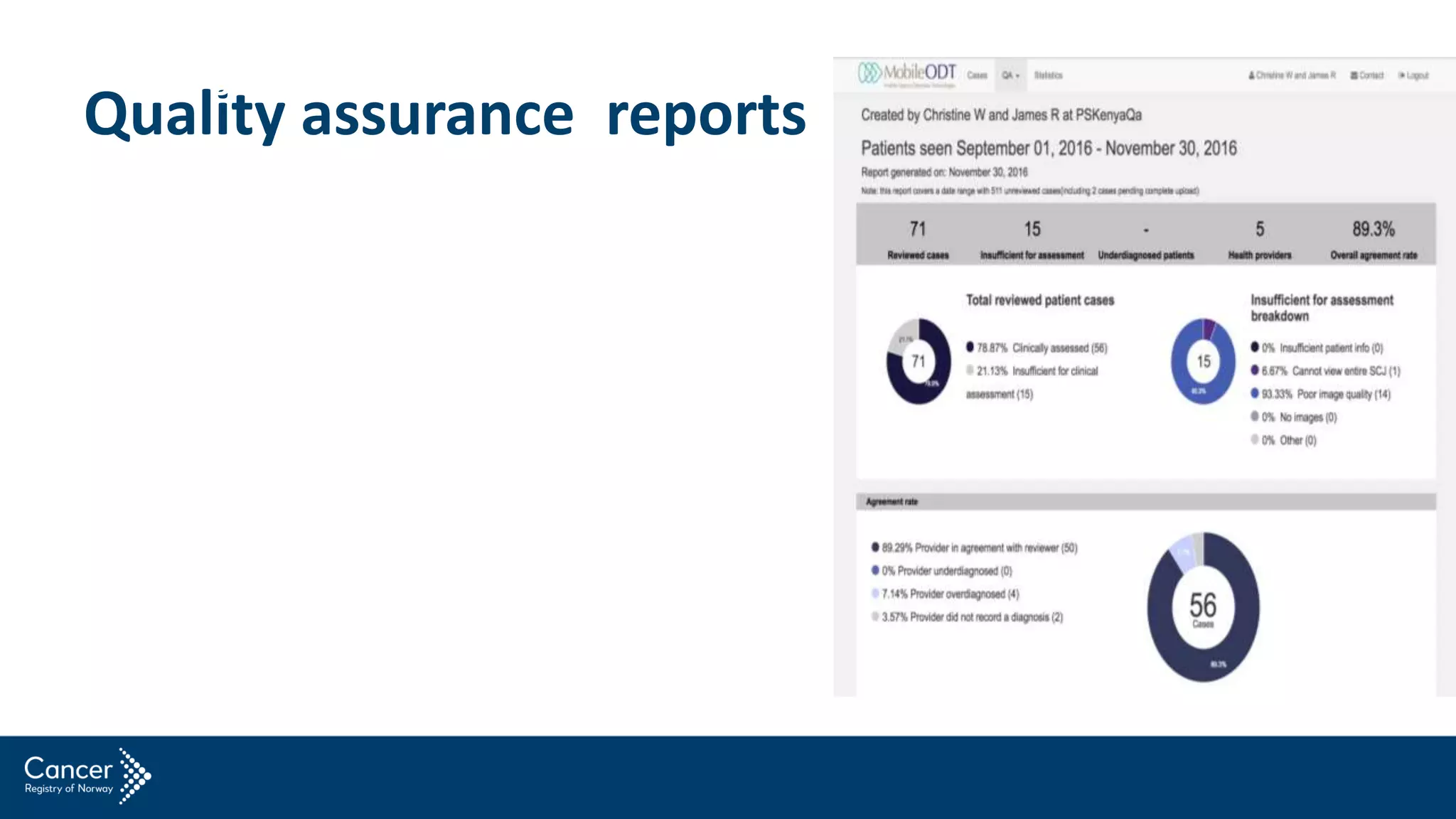
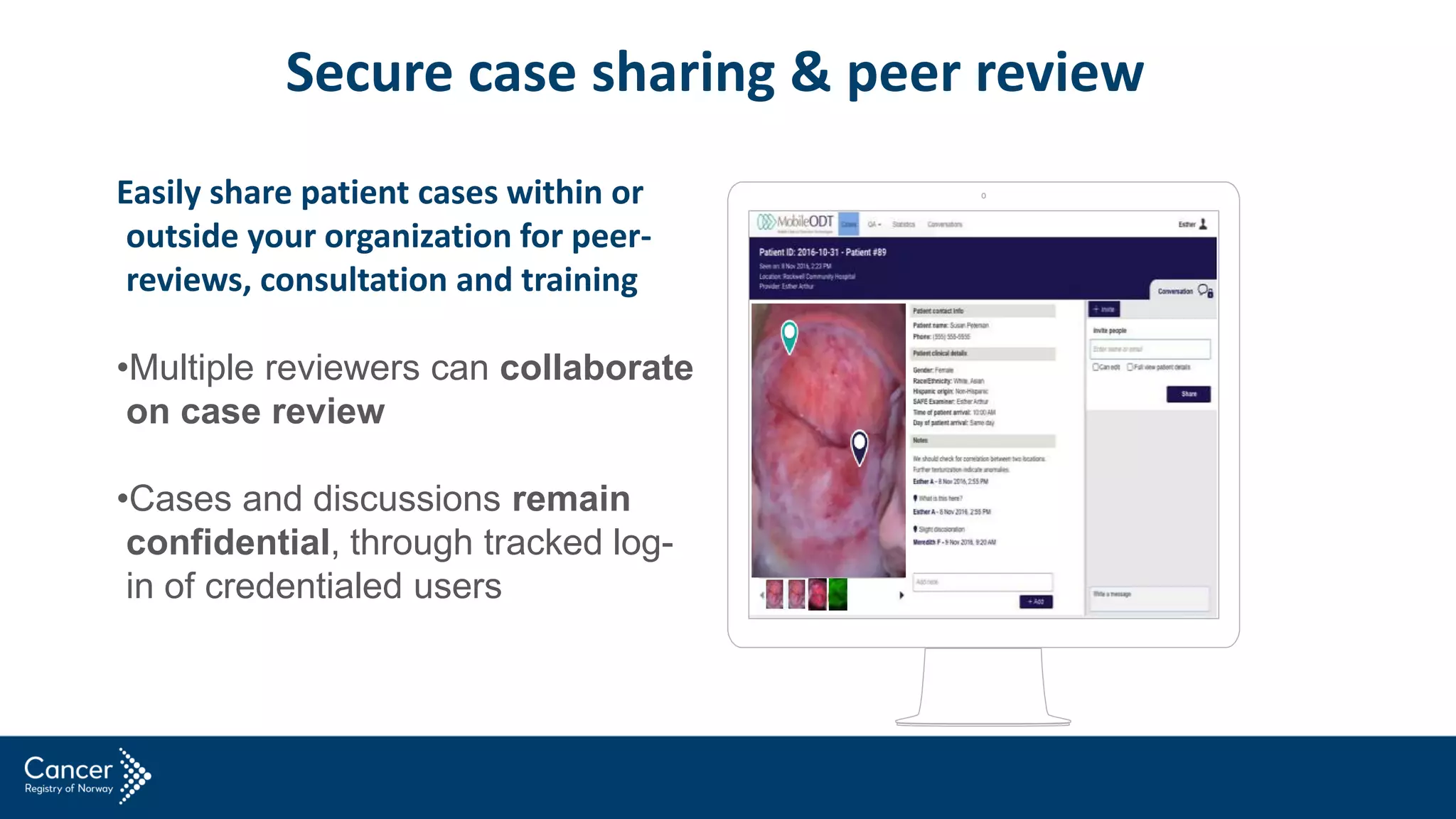
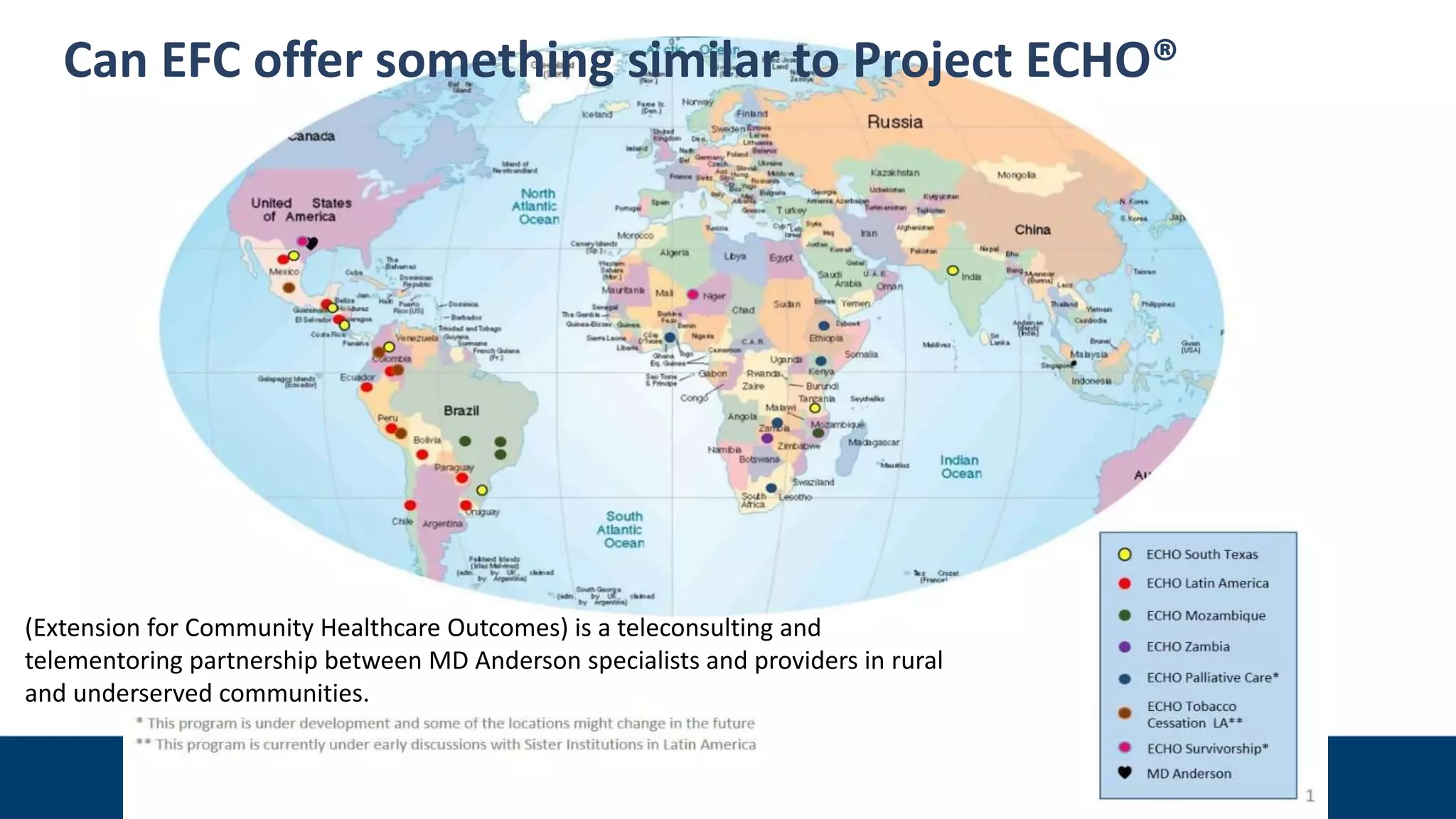
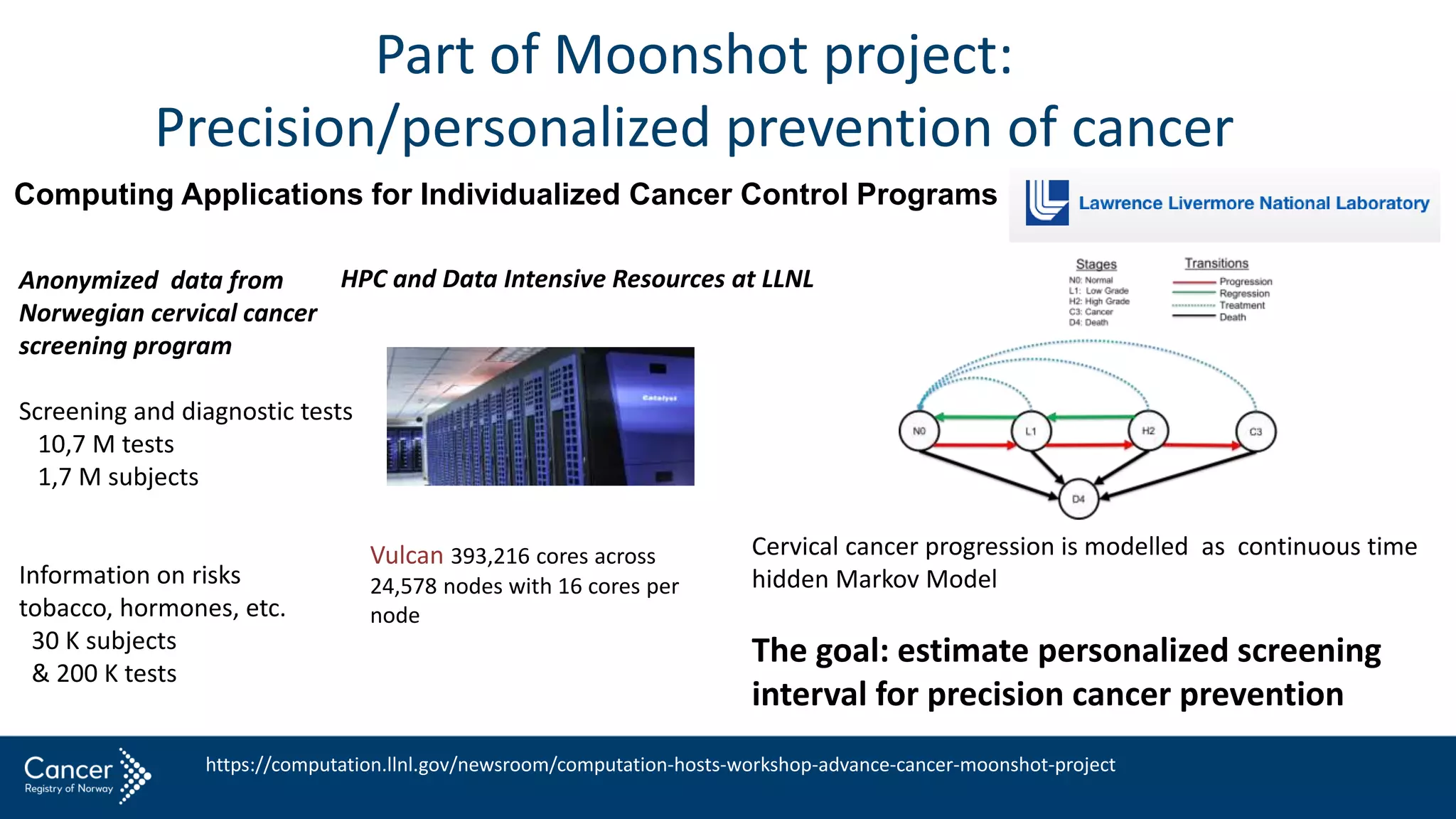
This document discusses using new image capturing and sharing systems to improve colposcopy training. It notes that training in Norway currently lacks organization and qualified trainers. Mobile technologies like smartphones with specialized applications could allow trainees to capture high-quality colposcopy images and share them securely with remote experts for consultation and training. This may help qualify more trainees more quickly and improve quality assurance. The document proposes a pilot project using mobile colposcopy units to train gynecologists abroad, with follow-up evaluation and mentoring via mobile communication.