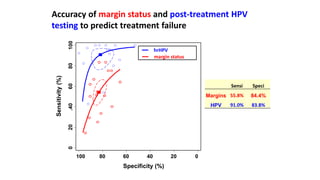
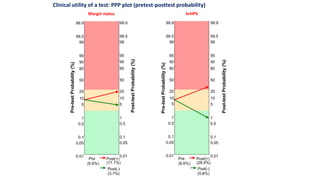
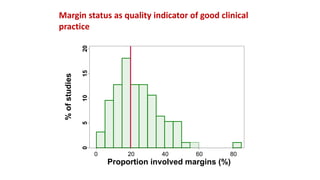
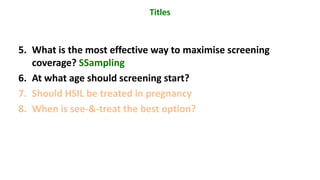
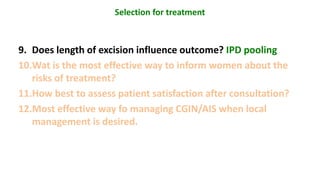
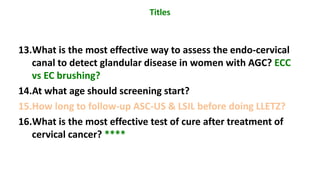
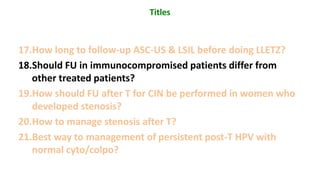
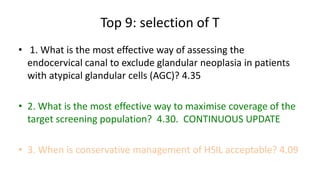
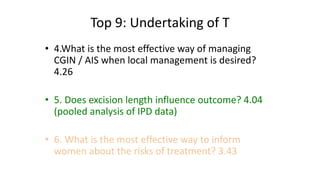
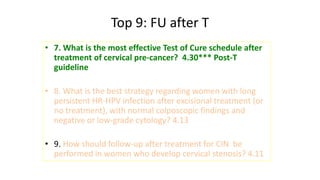
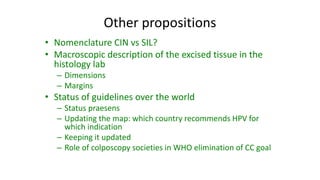
This document discusses potential topics for systematic reviews to inform EFC/ESGO guidelines on HPV-related precancer prevention and treatment. It lists 22 topics that were proposed for review, including evaluating diagnostic technologies, management of HSIL in different populations, treatment follow-up, and quality indicators. The top 9 priority topics were selected and cover issues related to assessing endocervical disease, treatment methods, conservative management, treatment risks, and follow-up after treatment. Other proposed topics included nomenclature, data pooling from European centers, and registry studies.