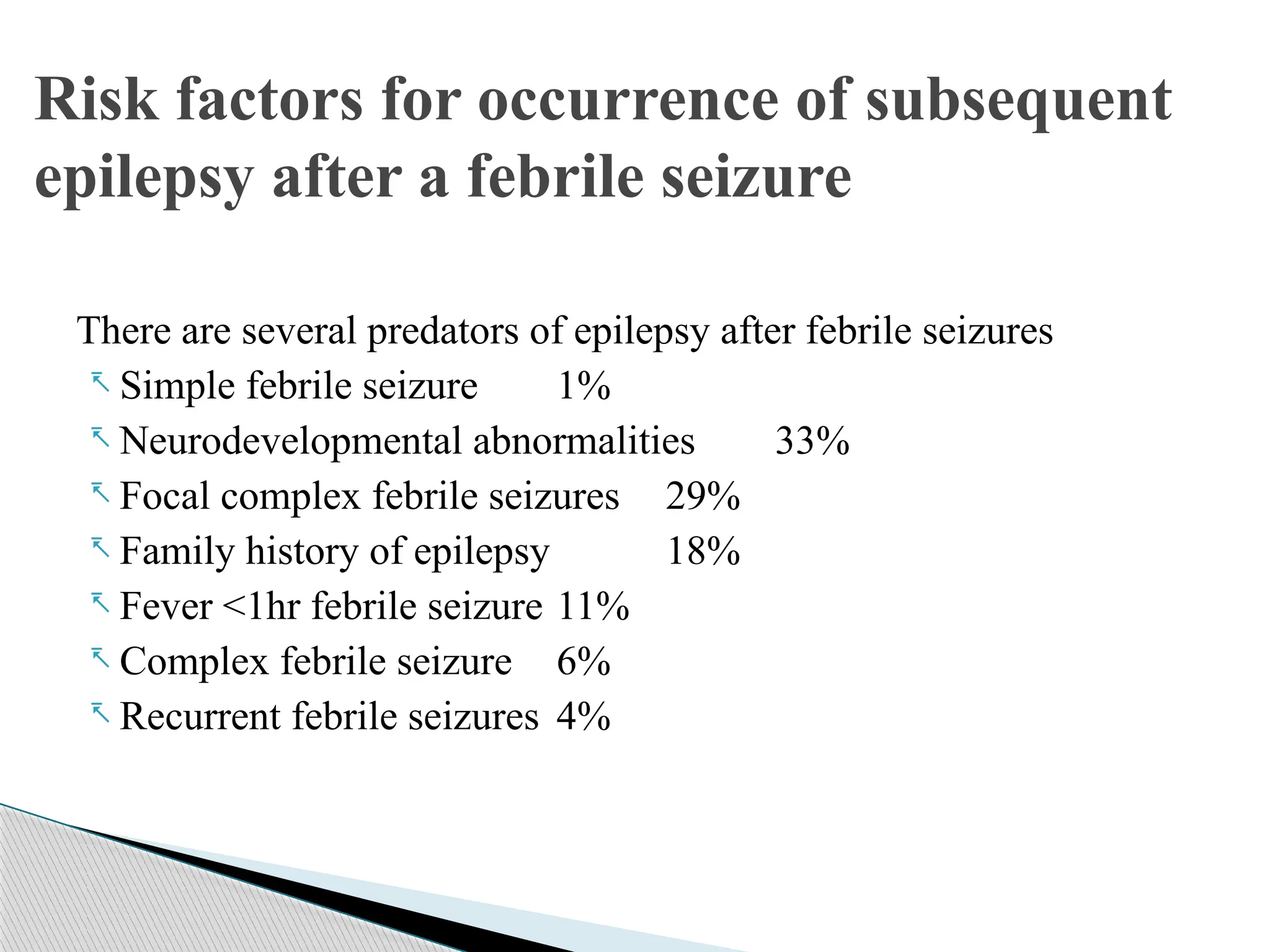
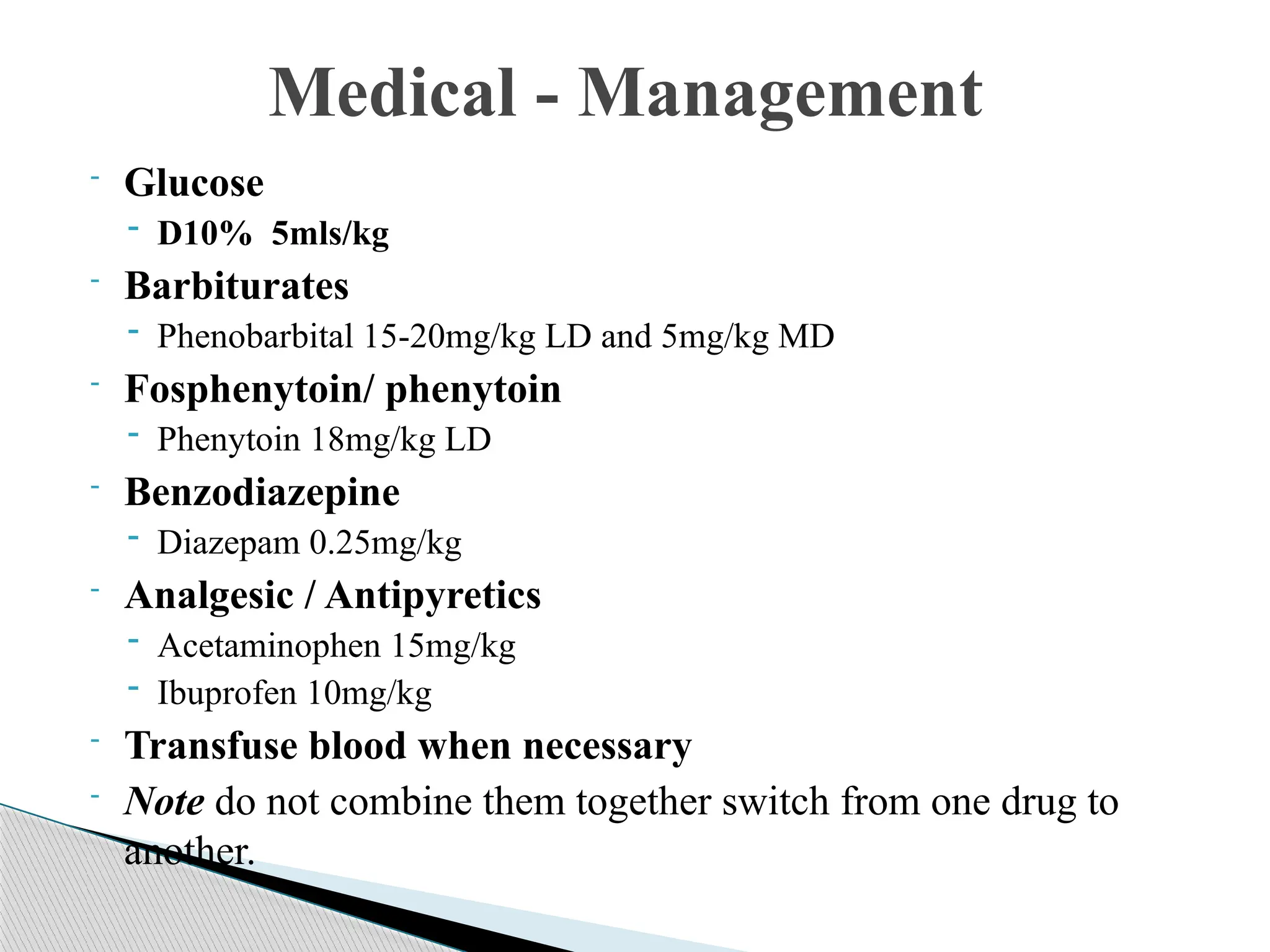
Febrile convulsions, occurring in children aged 6 months to 5 years with a temperature of 38°C or higher, are classified into simple and complex seizures. These seizures are primarily caused by viral infections and involve reactions in the immune system leading to increased neuronal activity due to cytokine release. Management includes maintaining safety, assessing vital signs, and administering medications such as antipyretics and anticonvulsants.