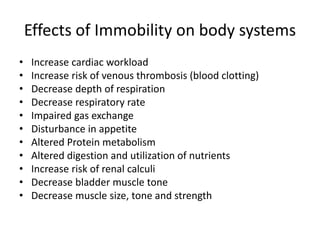
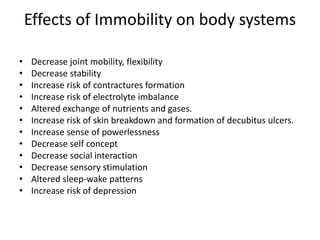
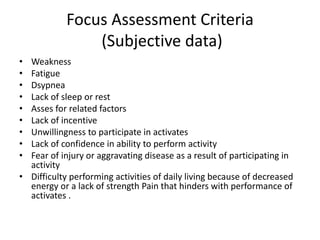
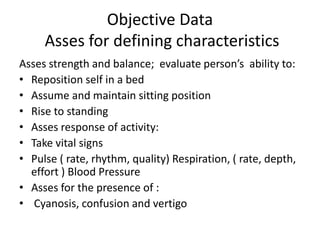
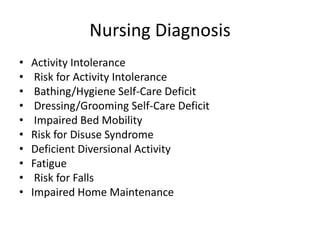
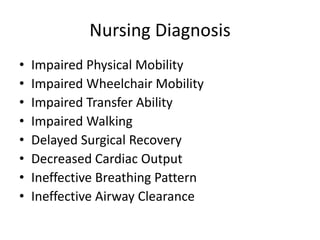
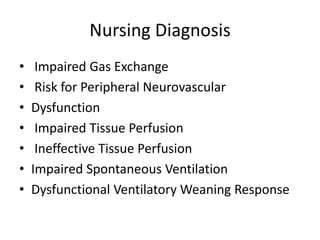
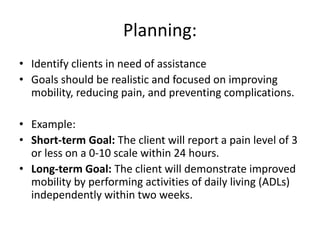
The document discusses the activity and exercise pattern of patients, including the definitions of activity, exercise, and activity tolerance, while highlighting factors affecting mobility. It emphasizes the importance of proper body mechanics and body alignment to prevent injuries and outlines the benefits of exercise and effects of immobility on bodily systems. Additionally, it covers nursing diagnoses related to activity and mobility, planning and implementing strategies for improvement, and evaluating patient progress.