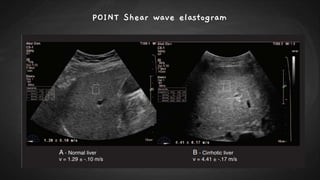
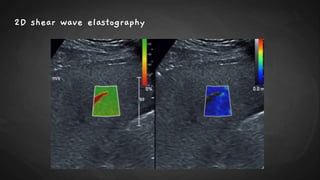
Ultrasound elastography is a noninvasive imaging technique that evaluates tissue stiffness, employing principles similar to manual palpation and relying on the mechanical properties of tissues under stress. It primarily utilizes two methods: strain elastography, which provides qualitative and semi-quantitative data, and shear wave elastography, which offers quantitative assessments of tissue stiffness. Clinical applications extend across various organs, including the liver, prostate, thyroid, and breast, improving diagnostic accuracy in conditions like fibrosis and tumors.


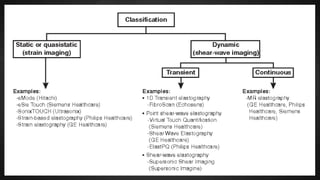
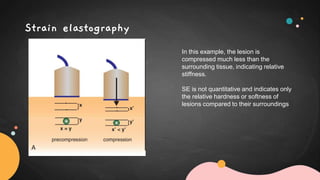
![Elastography uses principally two different approaches
according to the type of compression force (excitation)
and elasticity evaluation:
○ Quasistatic/ Strain
elastography, with its
qualitative (based on
colorimetric maps) and
semiquantitative variants
(strain ratio value); and
○ Dynamic/ Shear wave
elastography [SWE], a
quantitative approach with
transducer-induced high
acoustic pulse and
measures of the speed of the
shear wave generated.](https://image.slidesharecdn.com/ultrasoundelastography-210610085109/85/Ultrasound-elastography-13-320.jpg)
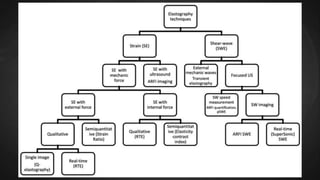

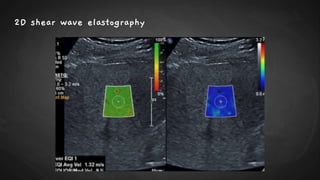
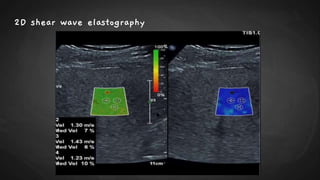
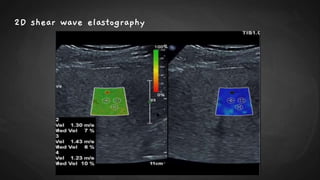
![● SWE can be performed using acoustic radiation force impulse (ARFI) technology either in a
1. Point–shear wave elastography, (p-SWE) small region of interest (ROI) or
2. Two-dimensional shear wave elastography [2D-SWE] over a larger field of view using
color-coding to visually display the stiffness values](https://image.slidesharecdn.com/ultrasoundelastography-210610085109/85/Ultrasound-elastography-23-320.jpg)