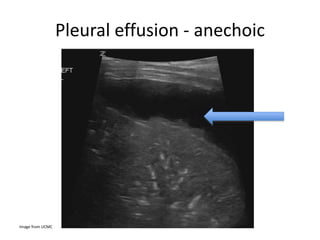
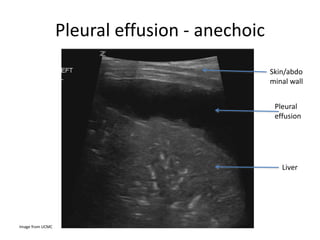
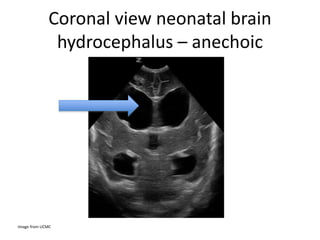
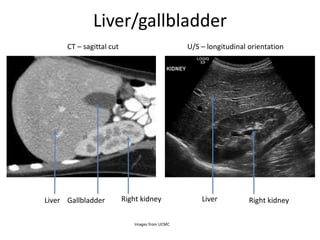
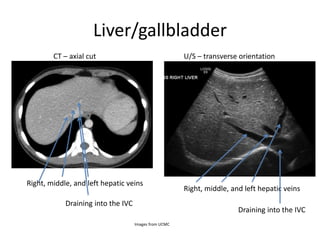
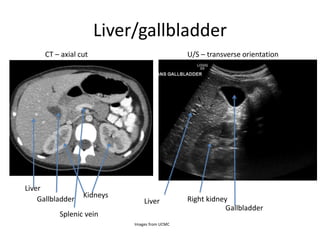
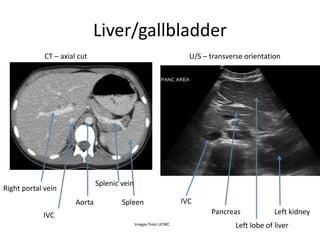
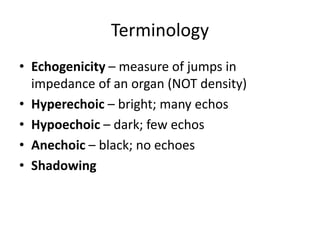
Ultrasound uses high-frequency sound waves to produce images of structures inside the body. It has several advantages over other imaging techniques, including lack of radiation exposure, low cost, portability, and ability to image different tissue planes. This document provides an introduction to ultrasound physics, terminology, machine components, and basic abdominal ultrasound imaging and interpretation for medical students. It discusses how ultrasound images are formed from sound wave reflections and demonstrates common ultrasound appearances of anatomical structures and pathologies.




![Frequencies
• Higher frequencies – better resolution but less
penetration [useful for thyroid, testes,
superficial blood vessels]
• Lower frequencies – better penetration but
worse resolution [useful for the abdomen,
aorta]](https://image.slidesharecdn.com/ultrasoundbasics-230301211327-a69fd18b/85/Ultrasound-Basics-ppt-17-320.jpg)