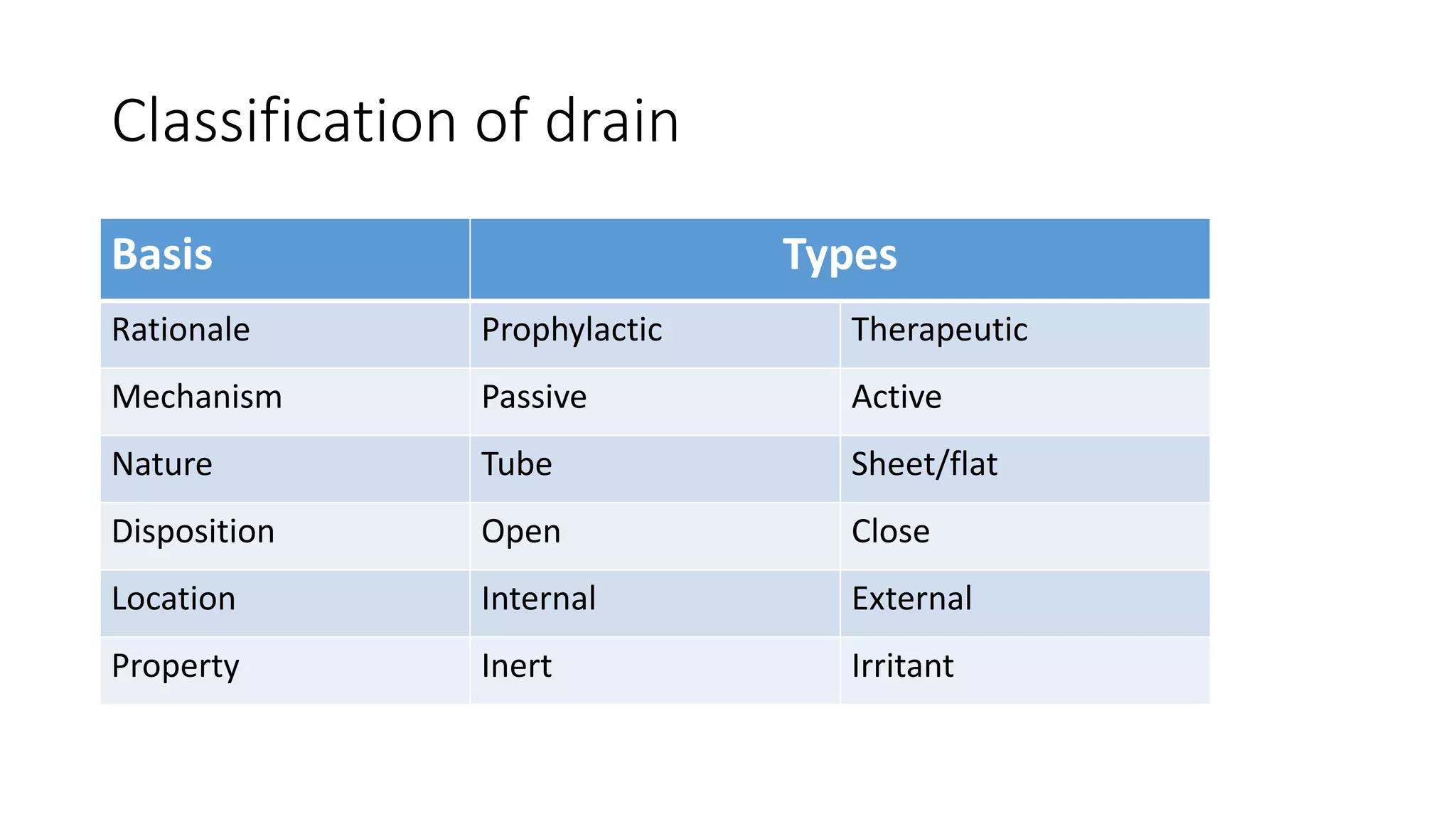
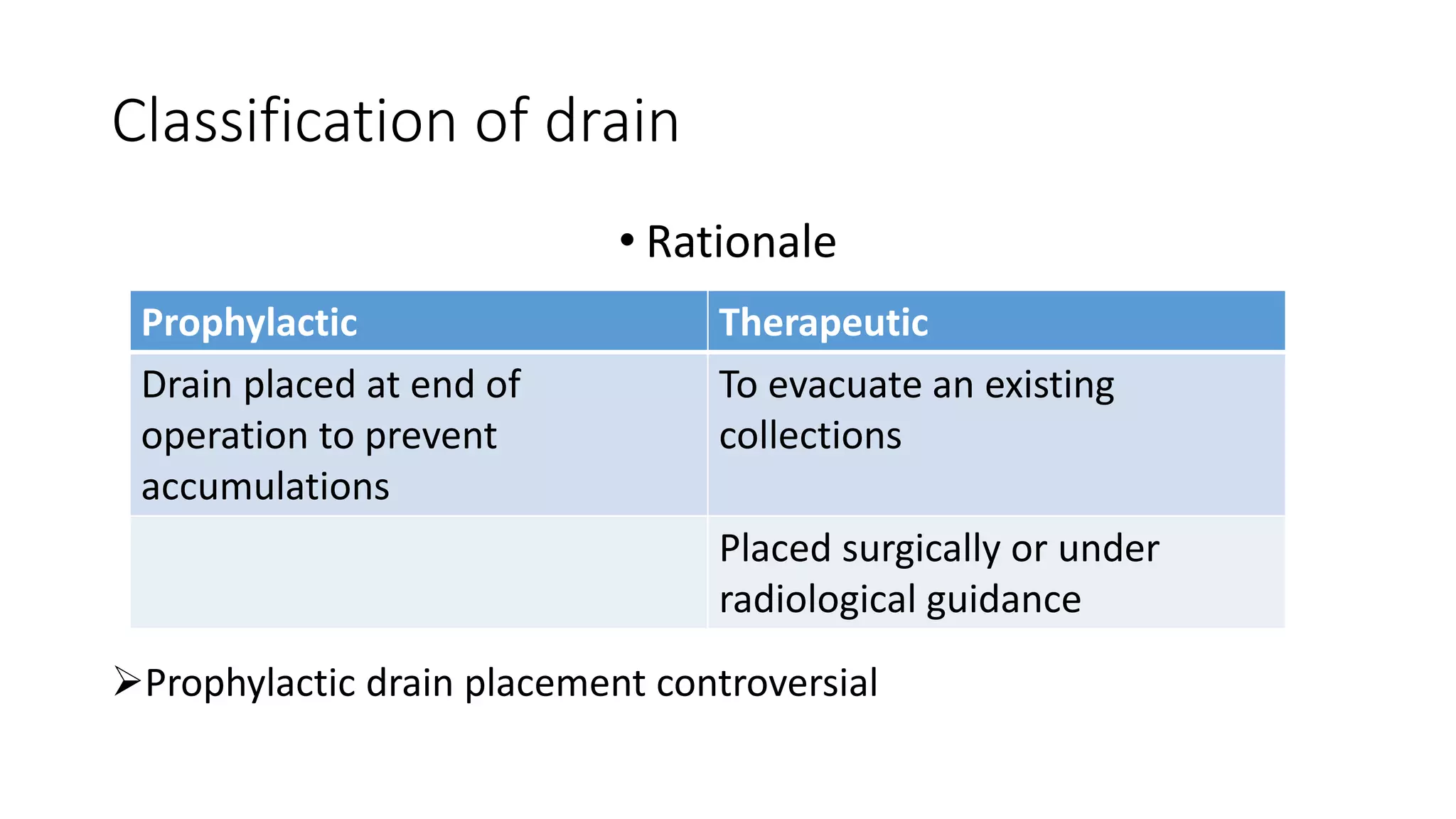
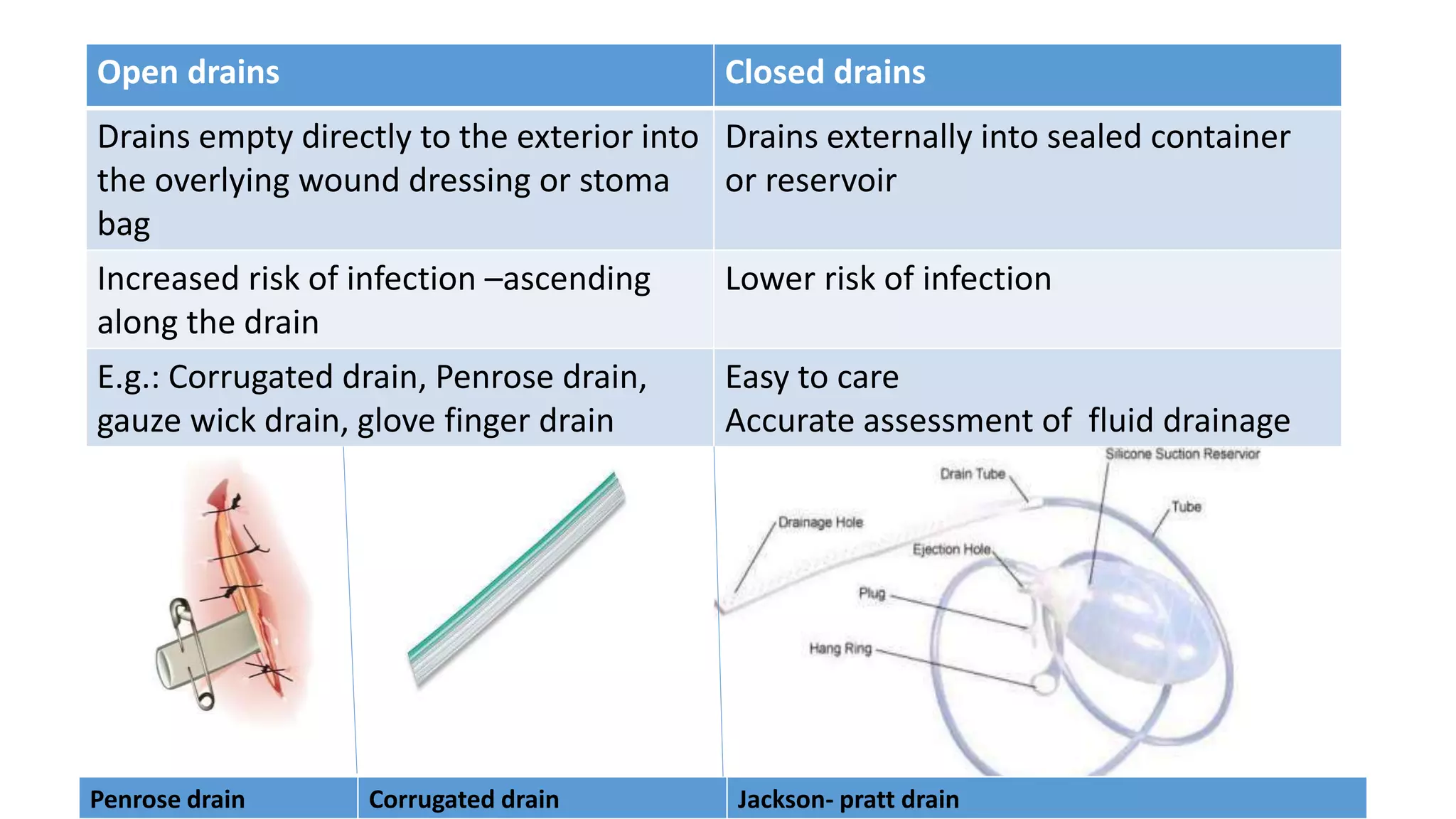
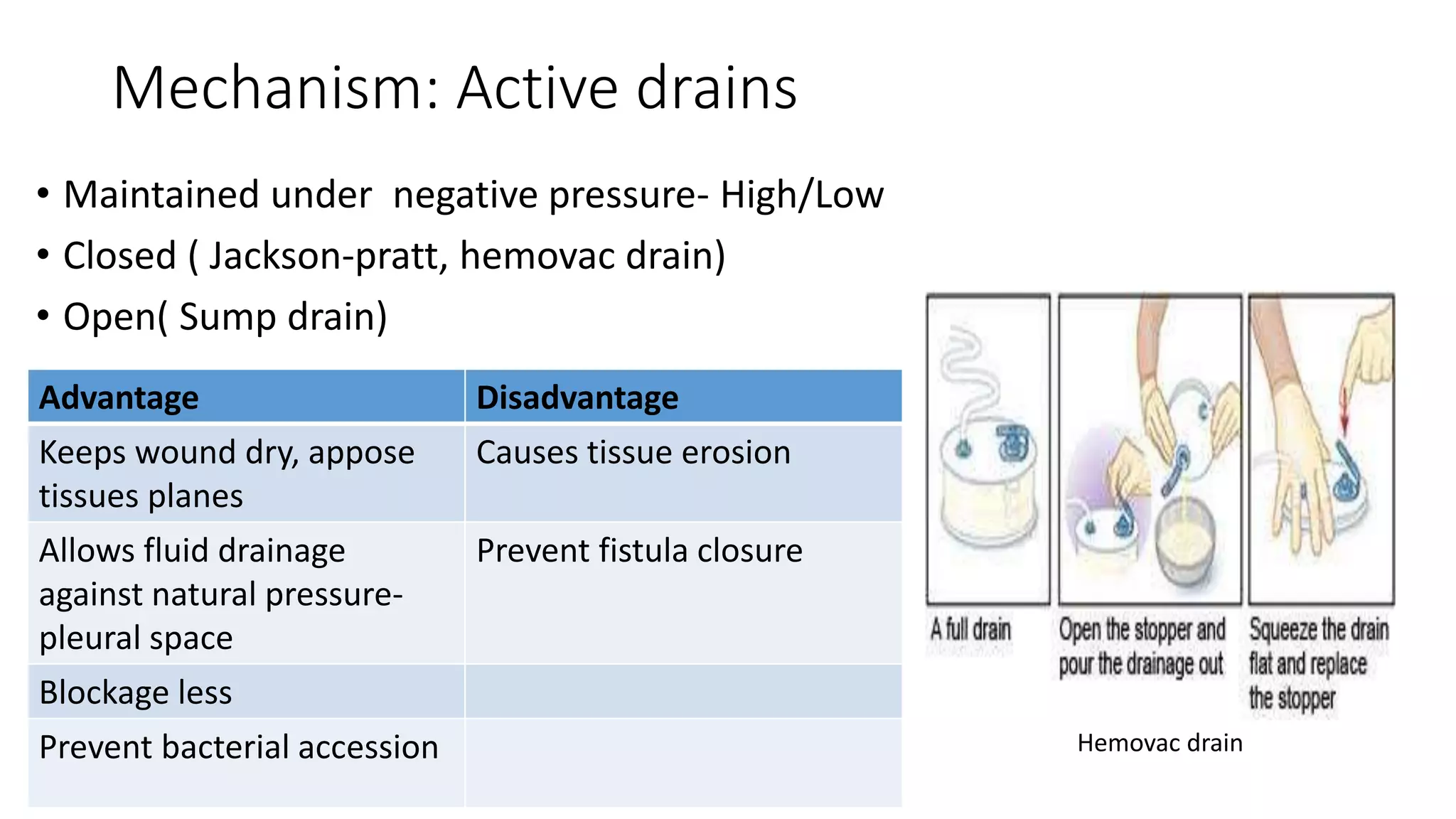
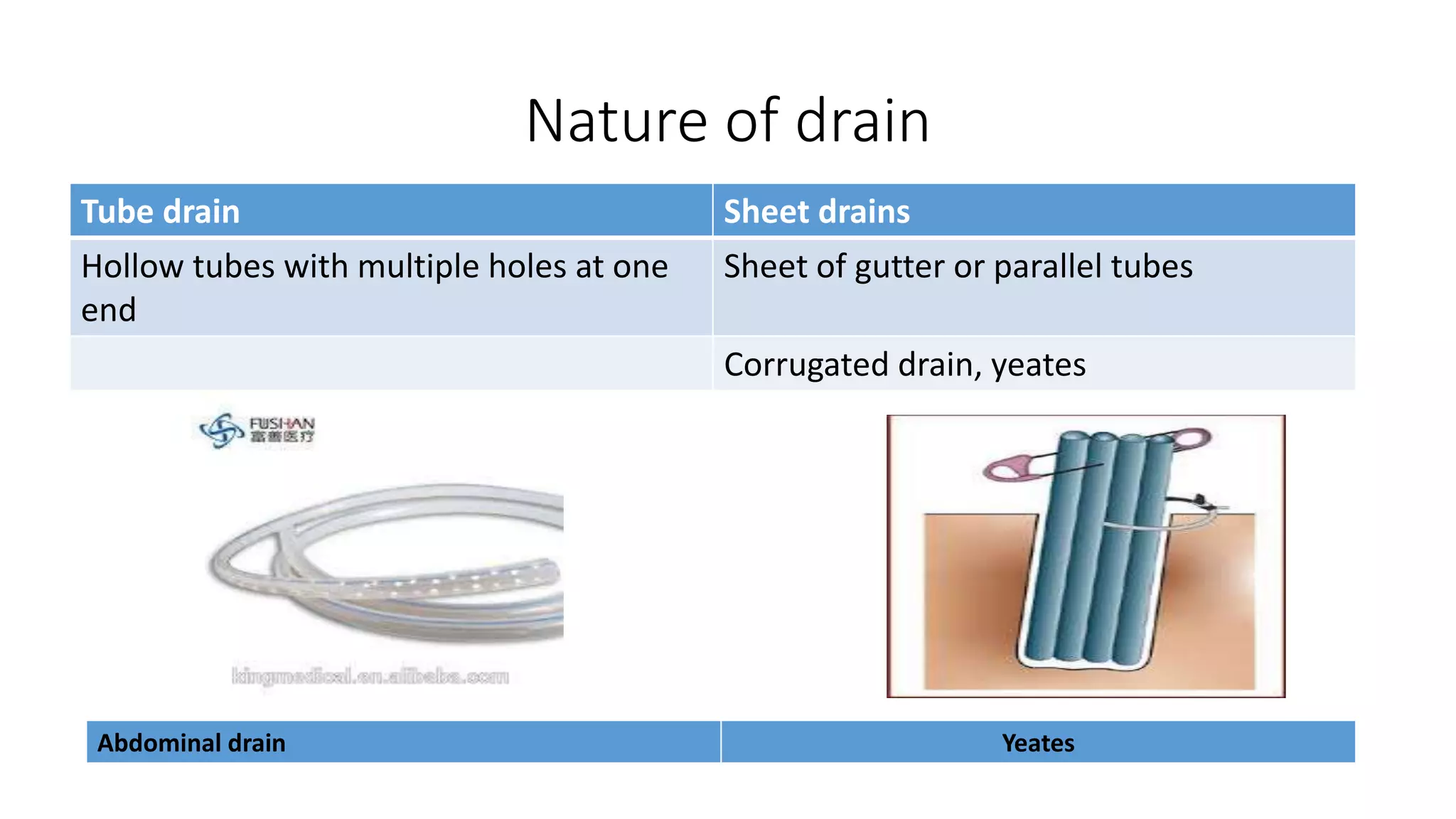
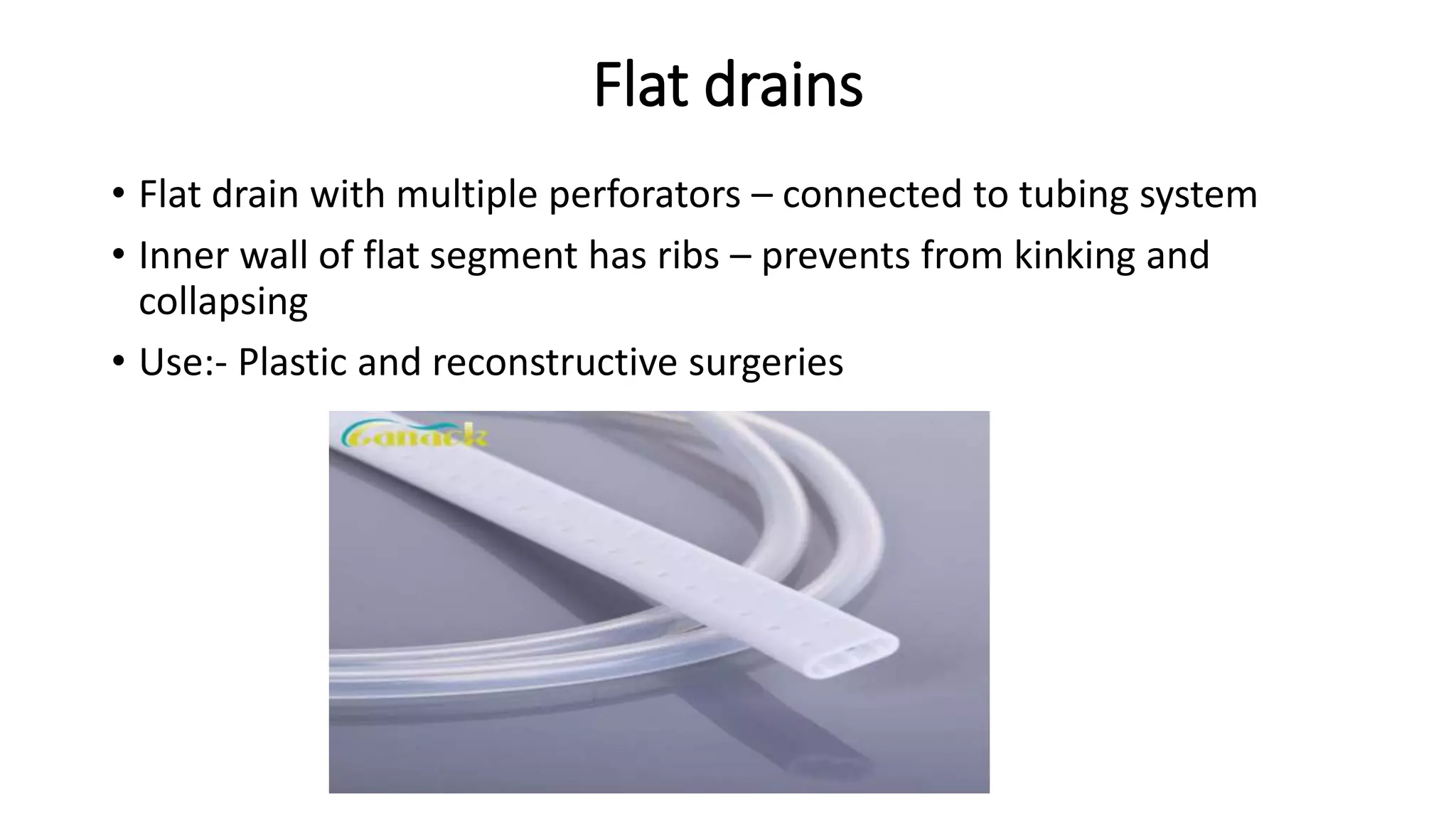
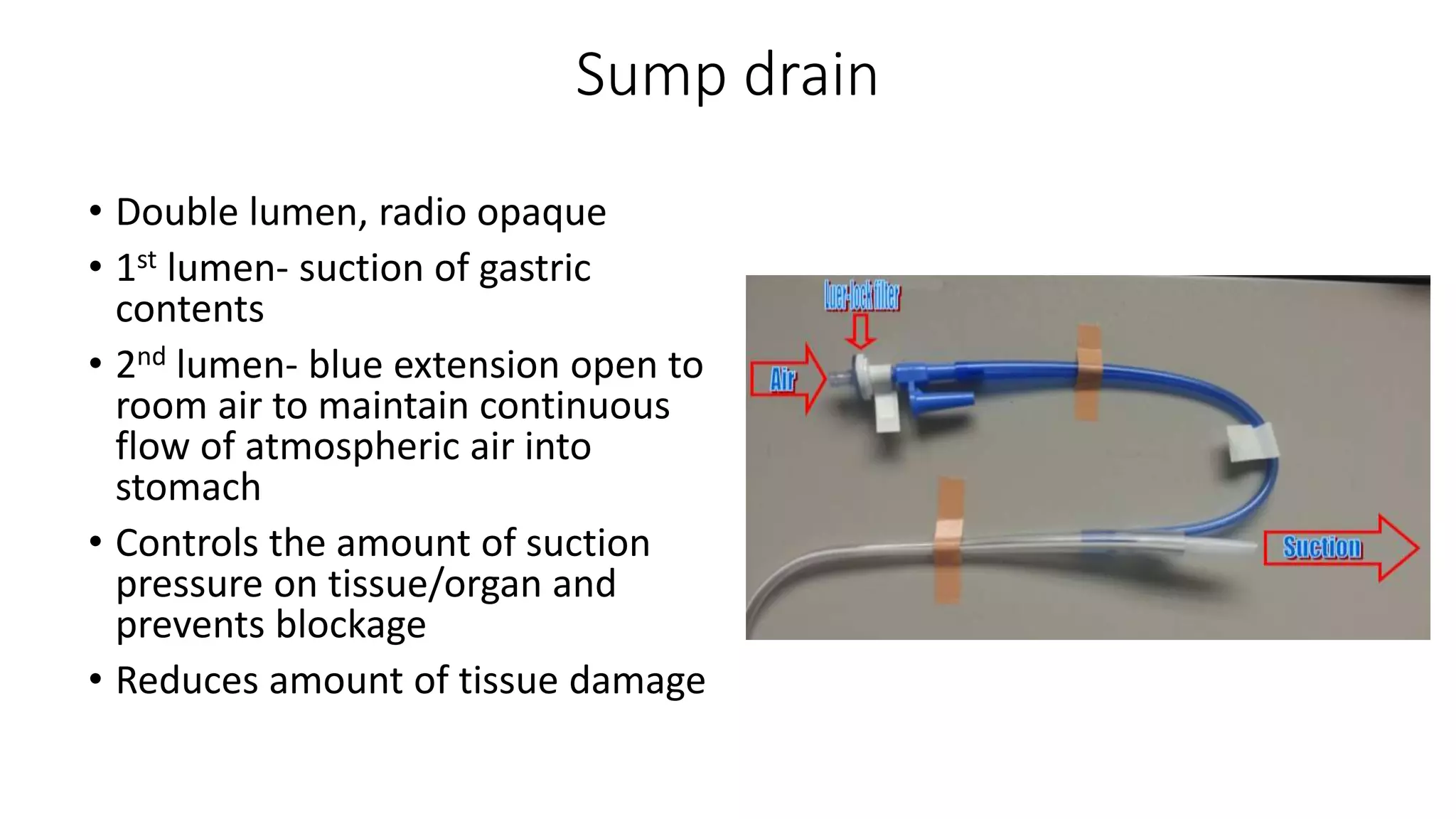
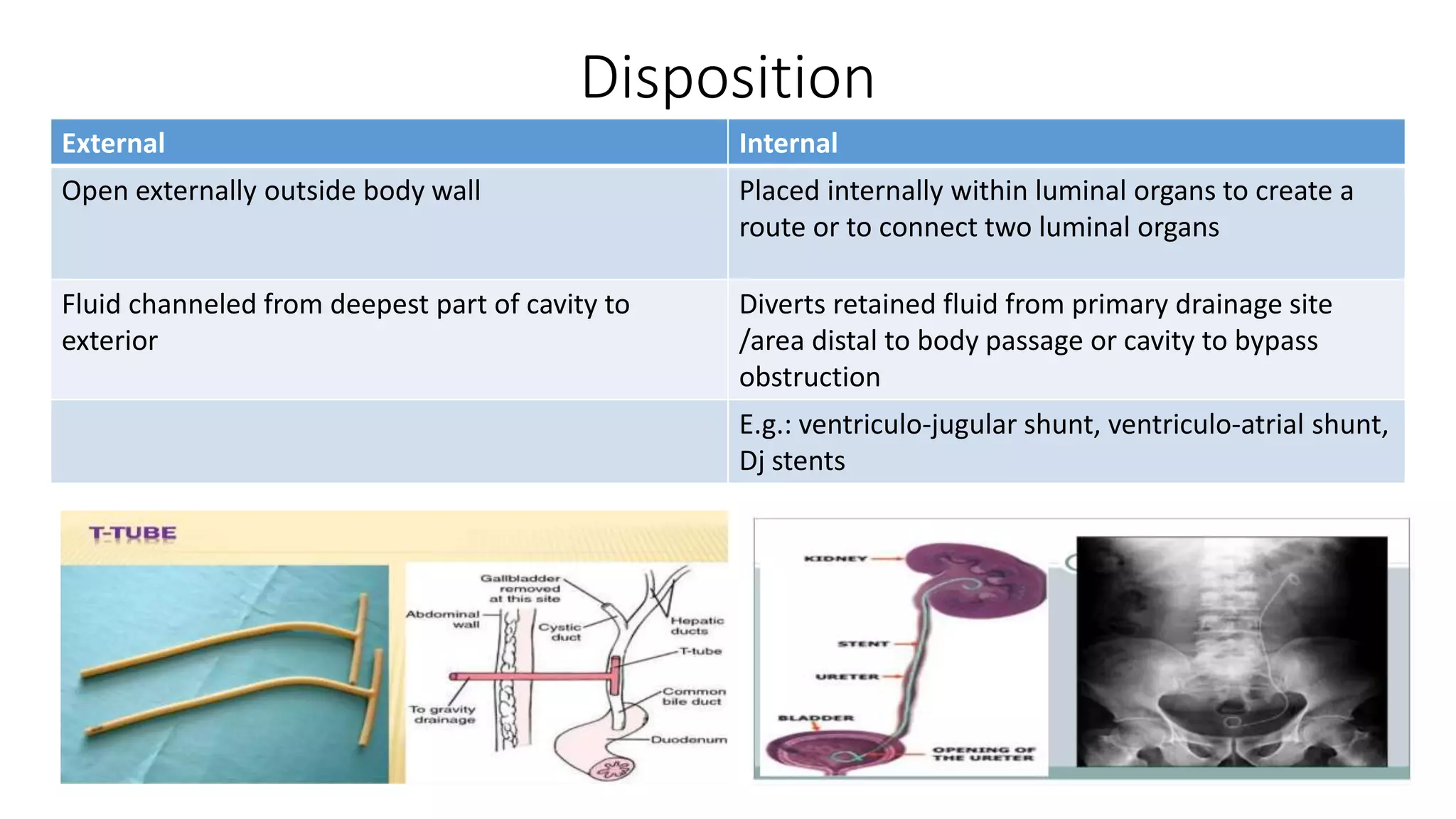
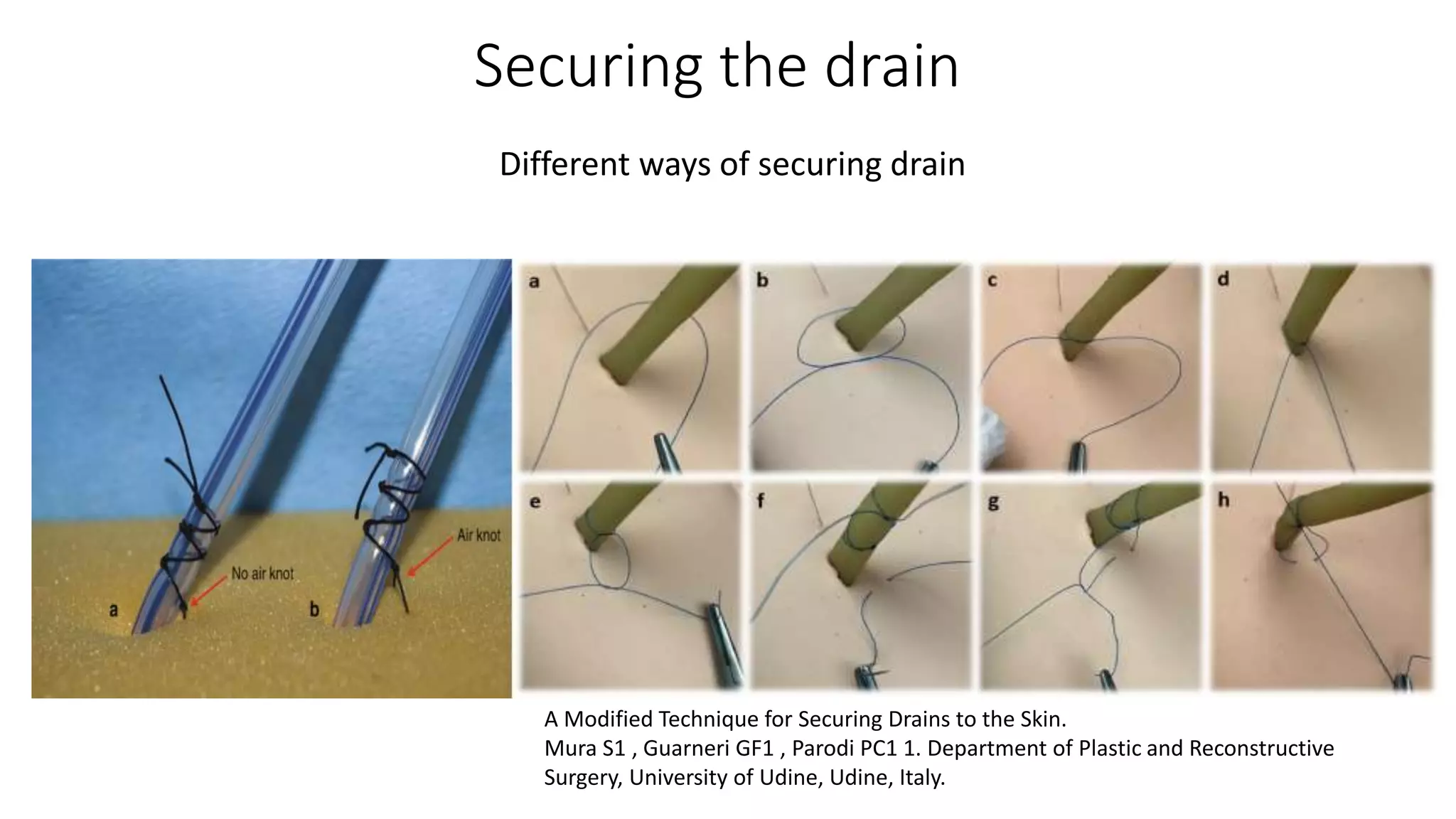
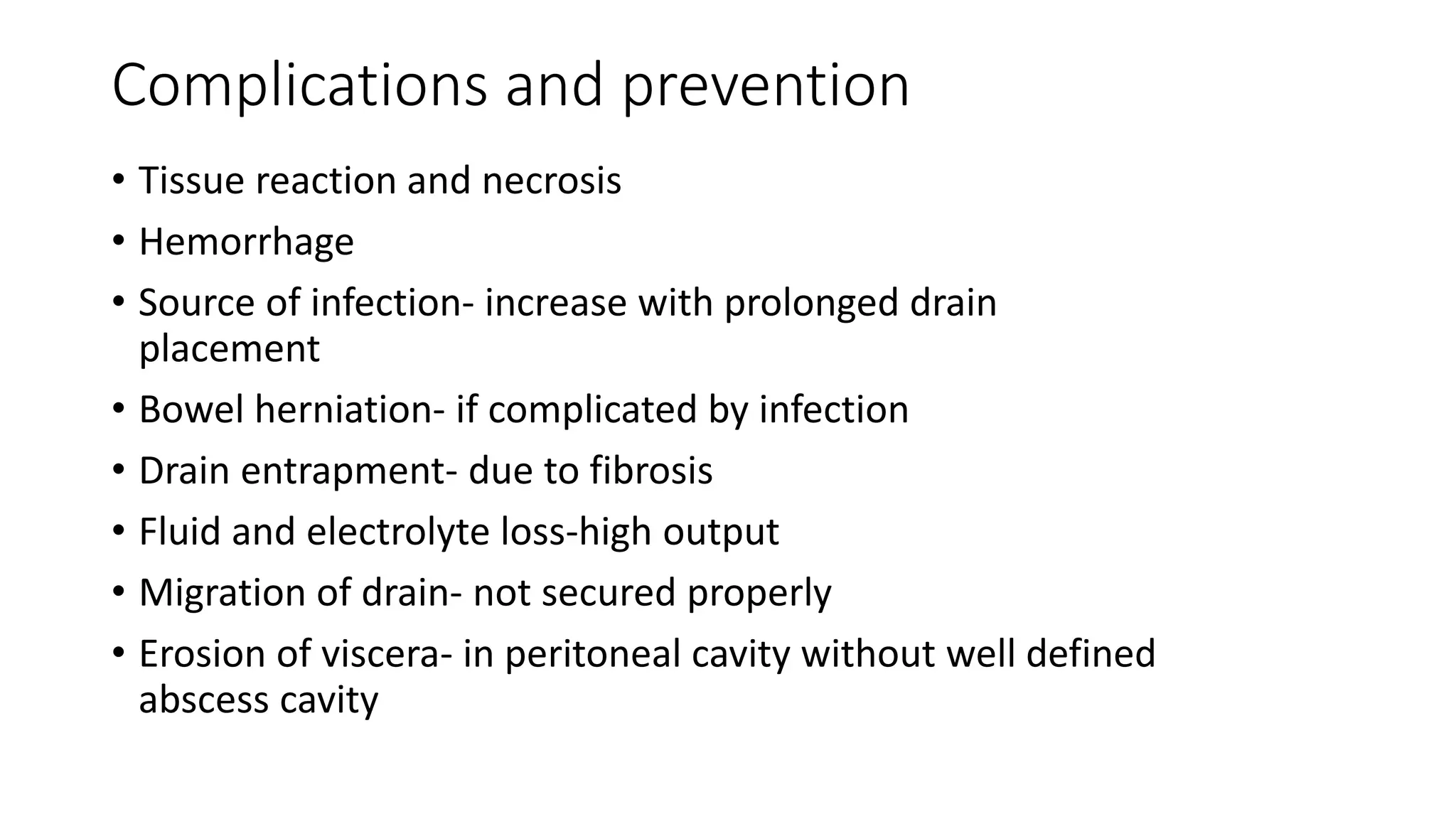
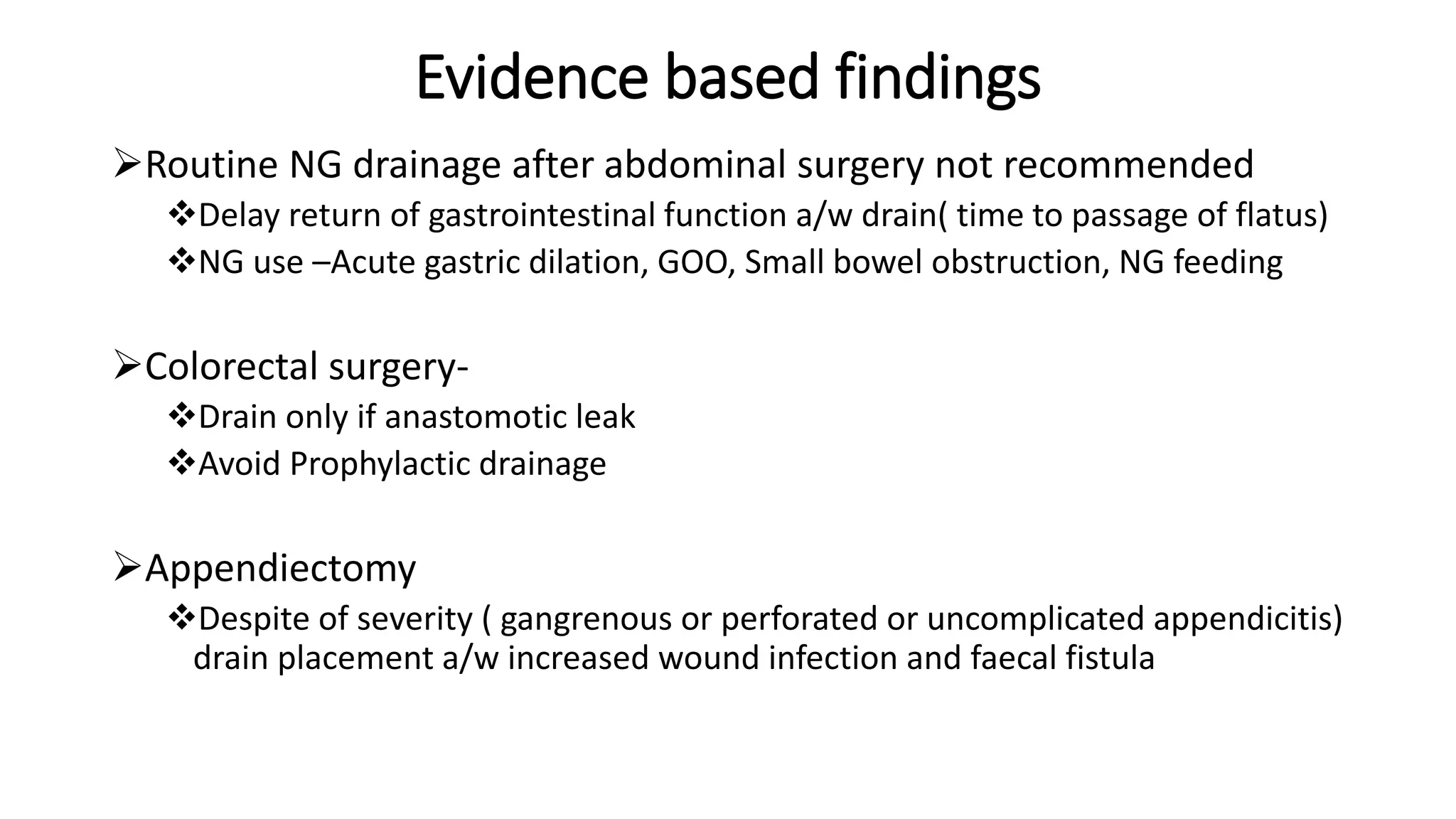
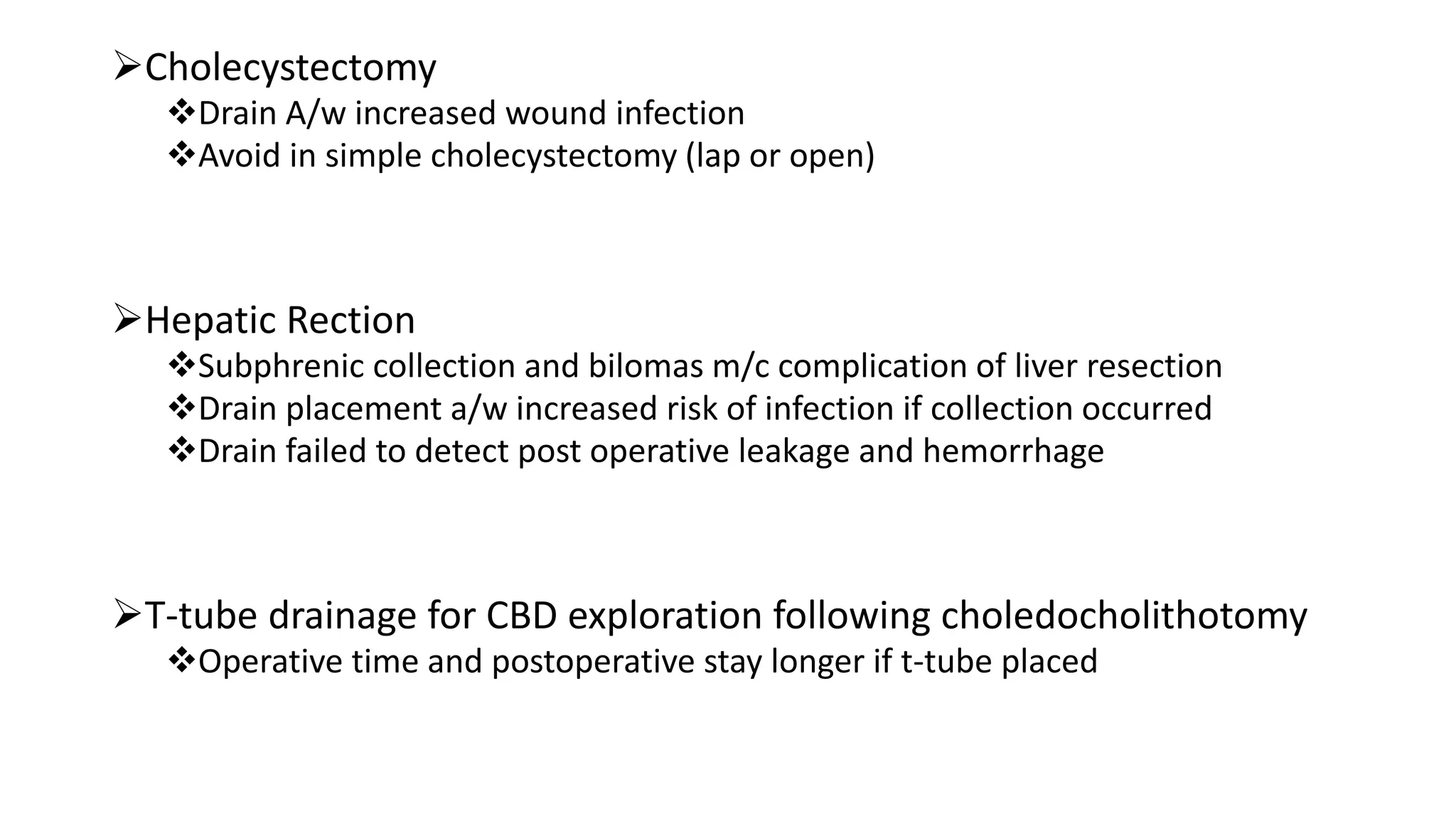
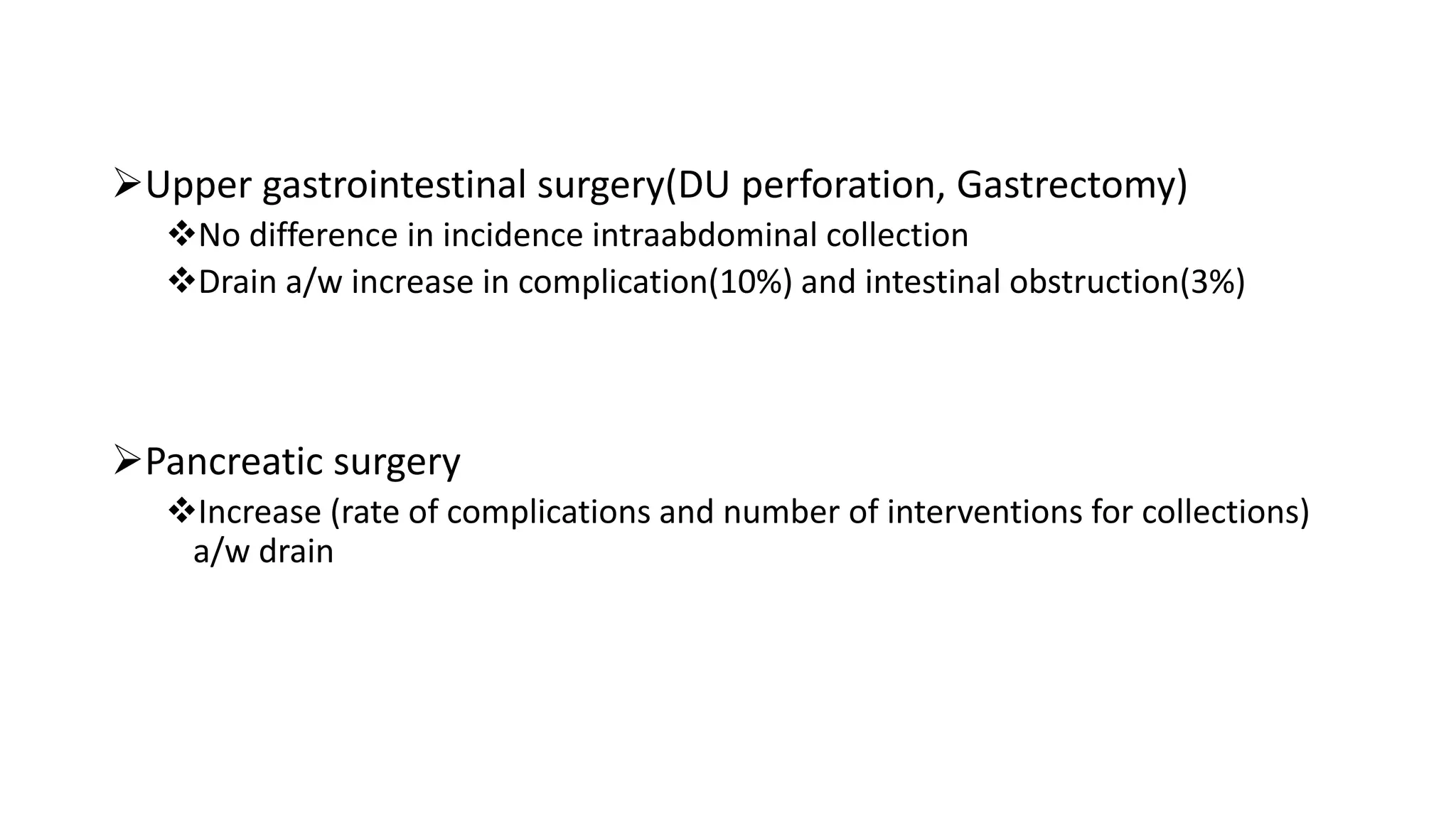
This document discusses tubes and drains used in surgery. It begins by outlining the objectives which are to discuss the principles, types, indications, insertion, care, removal and complications of surgical drains. It then defines drains and describes different types including passive vs. active, open vs. closed, internal vs. external. Placement, care, removal and complications of drains are explained. Evidence-based findings on drain use in different surgeries is presented, noting drains are not always recommended and may increase complications. Therapeutic drainage of symptomatic postoperative collections under imaging guidance is supported. The key messages are to use appropriate drains for the appropriate time based on evidence, and avoid prophylactic drains in many cases