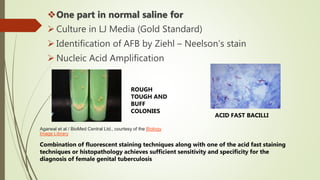
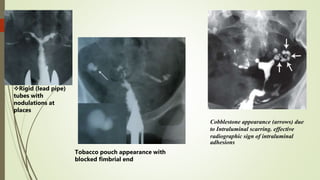
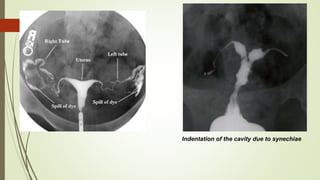
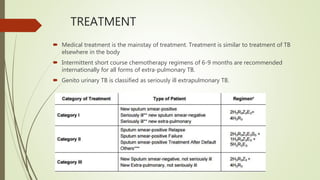
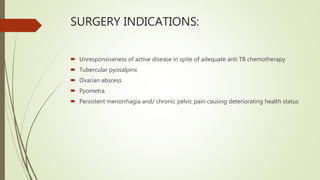
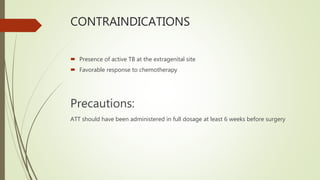
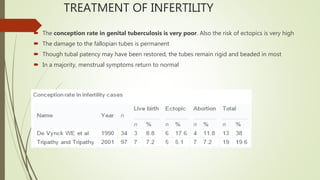
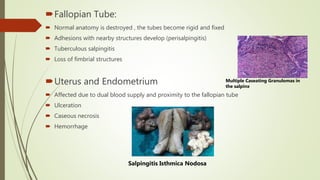
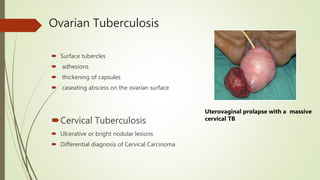
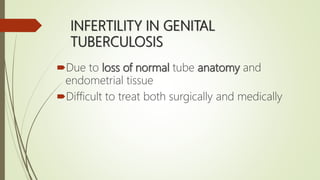
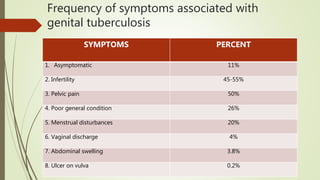
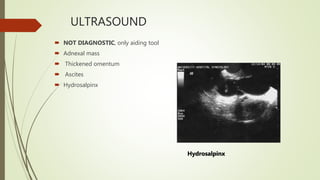
Genital tuberculosis is a significant cause of infertility globally, affecting an estimated 8-10 million women. It commonly involves the fallopian tubes, causing scarring and blockages that impair fertility. Diagnosis is challenging due to the paucibacillary nature of the infection and low sensitivity of diagnostic tests. Investigations include histopathology of endometrial tissue, nucleic acid amplification tests, culture, and imaging. Treatment involves a prolonged course of anti-tuberculosis medications, with surgery reserved for complications. Fertility outcomes are generally poor due to permanent tubal damage, but IVF may offer an option for conceiving.

![Jetley S, Rana S, Jairajpuri ZS. Morphological spectrum of endometrial pathology in middle-aged women with
atypical uterine bleeding: A study of 219 cases. J Mid-life Health [serial online] 2013 [cited 2015 Aug 19];4:216-20.
Available from: http://www.jmidlifehealth.org/text.asp?2013/4/4/216/122242](https://image.slidesharecdn.com/tuberculosisandinfertility-170217084855/85/Tuberculosis-and-infertility-25-320.jpg)