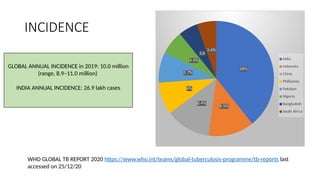
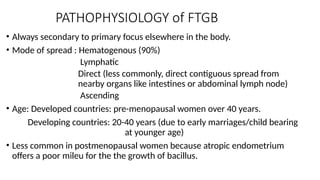
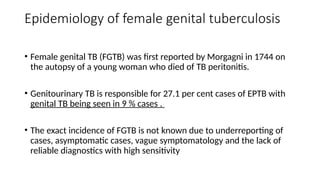
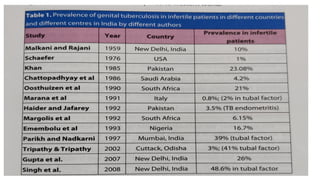
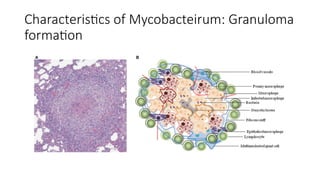
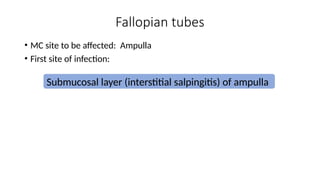
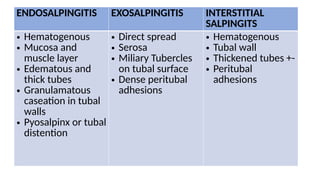
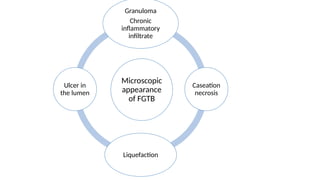
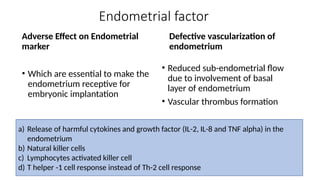
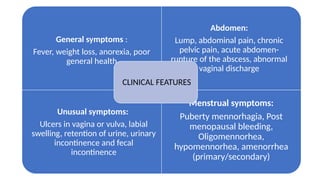
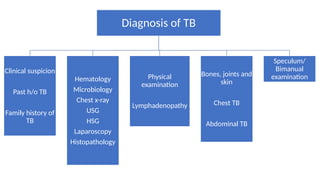
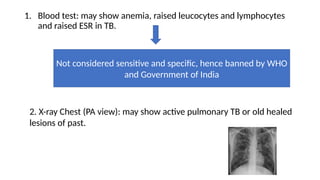
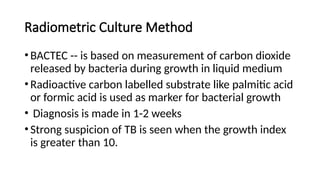
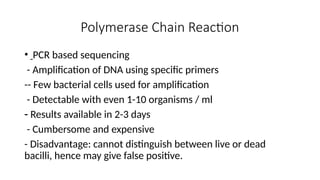
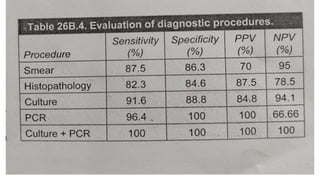
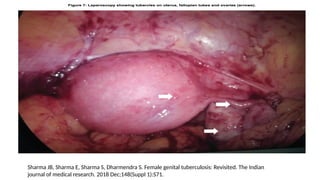
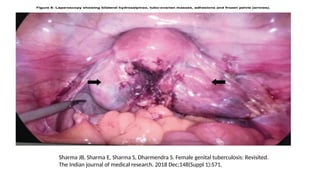
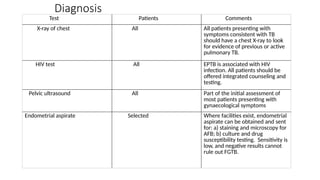
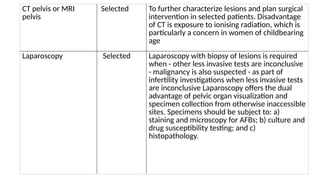
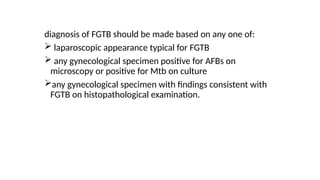
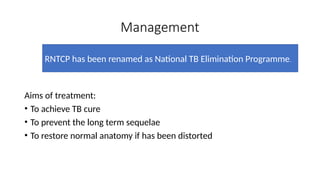
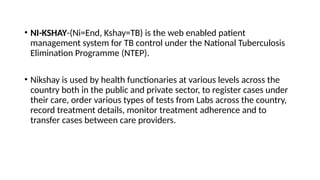
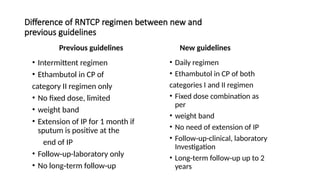
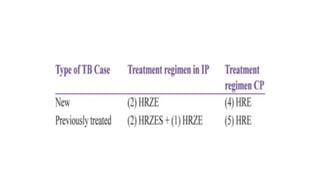
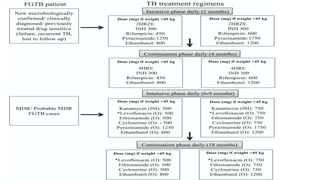
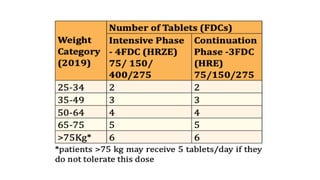
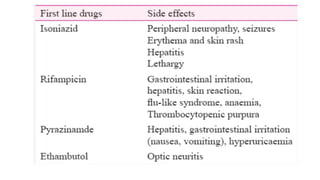
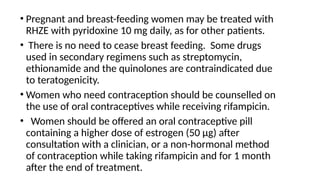
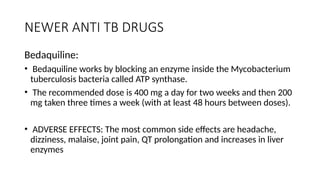
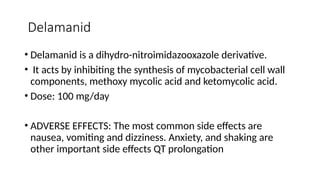
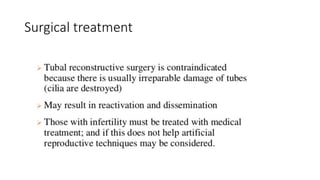
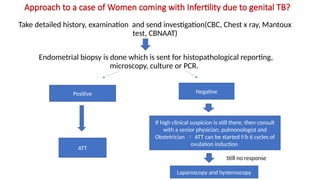
The document addresses genital tuberculosis (GTB), detailing its global incidence, pathophysiology, clinical symptoms, diagnosis, and management. It emphasizes the burden of disease, particularly in developing countries like India, and outlines the diagnostic challenges due to underreporting and nonspecific symptoms. The treatment protocols have been updated under India's National TB Elimination Programme, highlighting the need for comprehensive patient management systems.