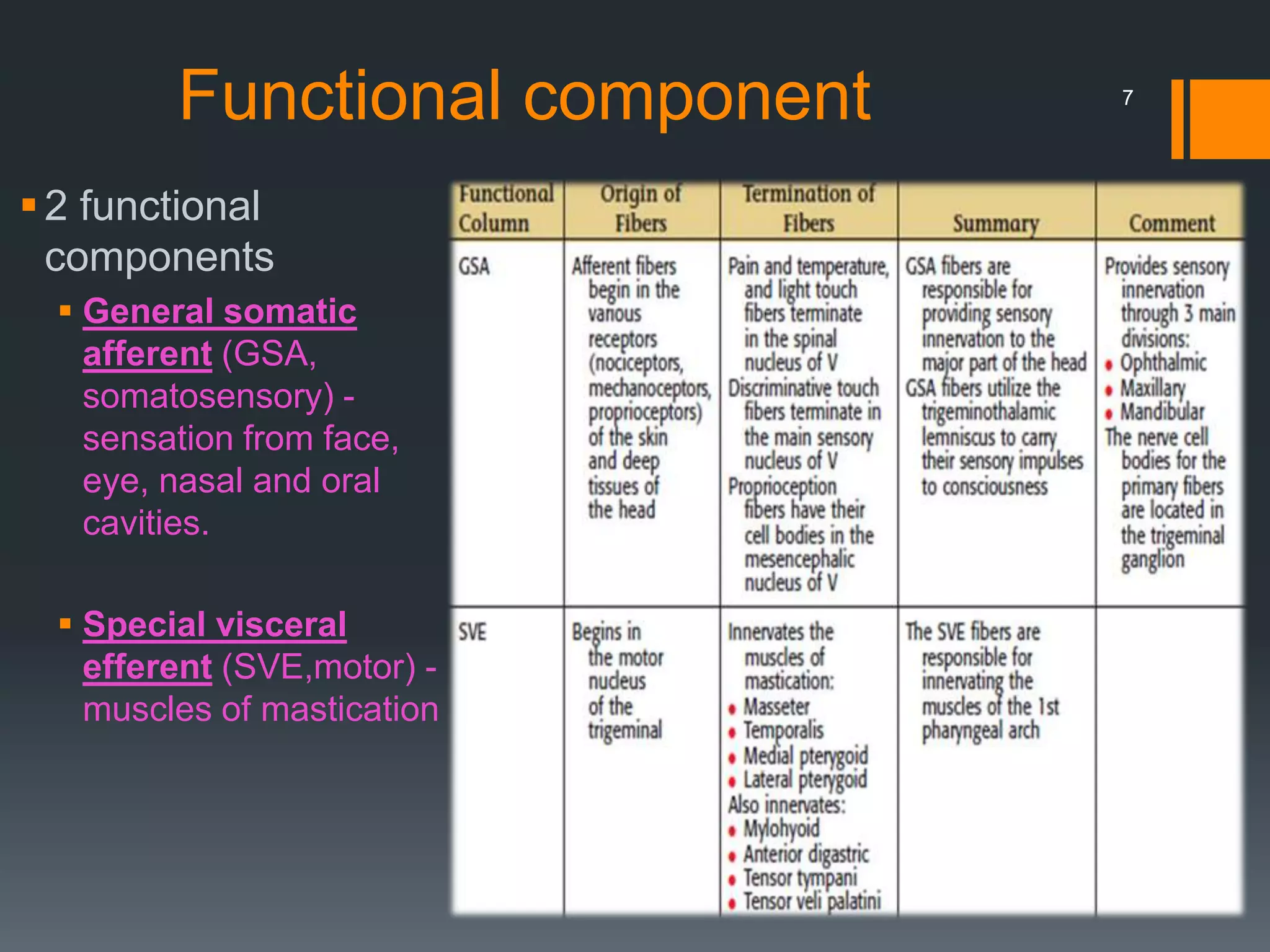
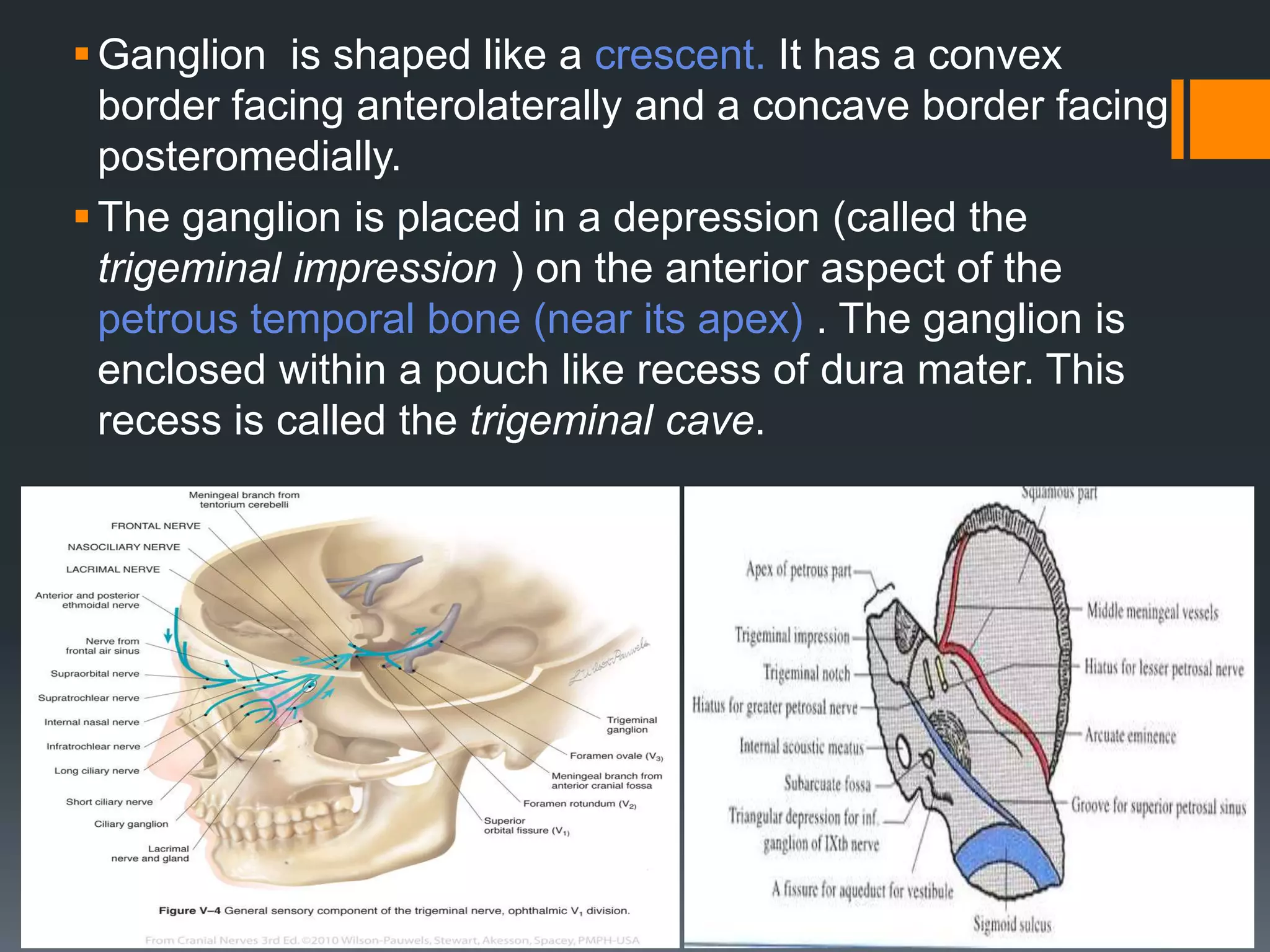
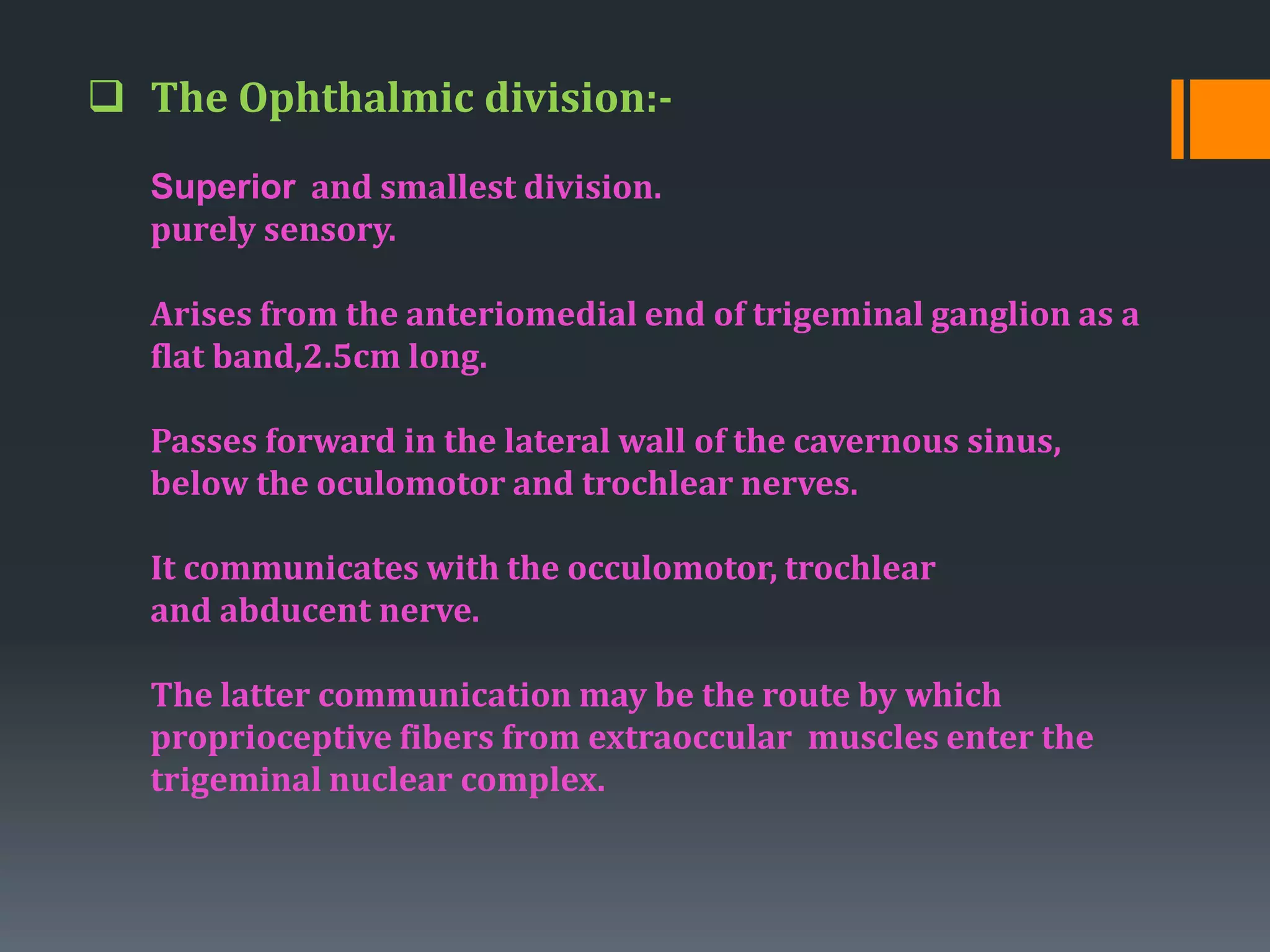
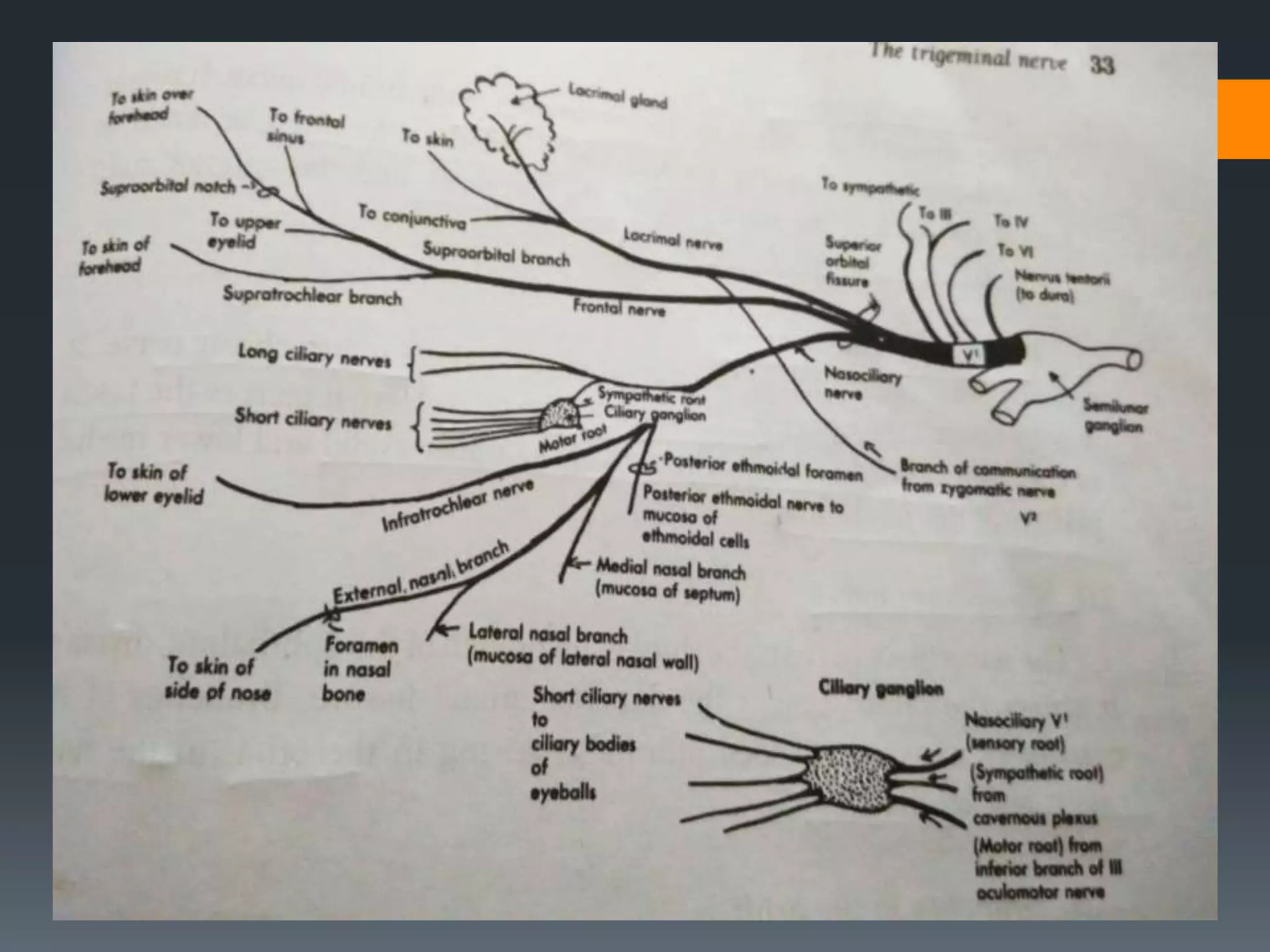
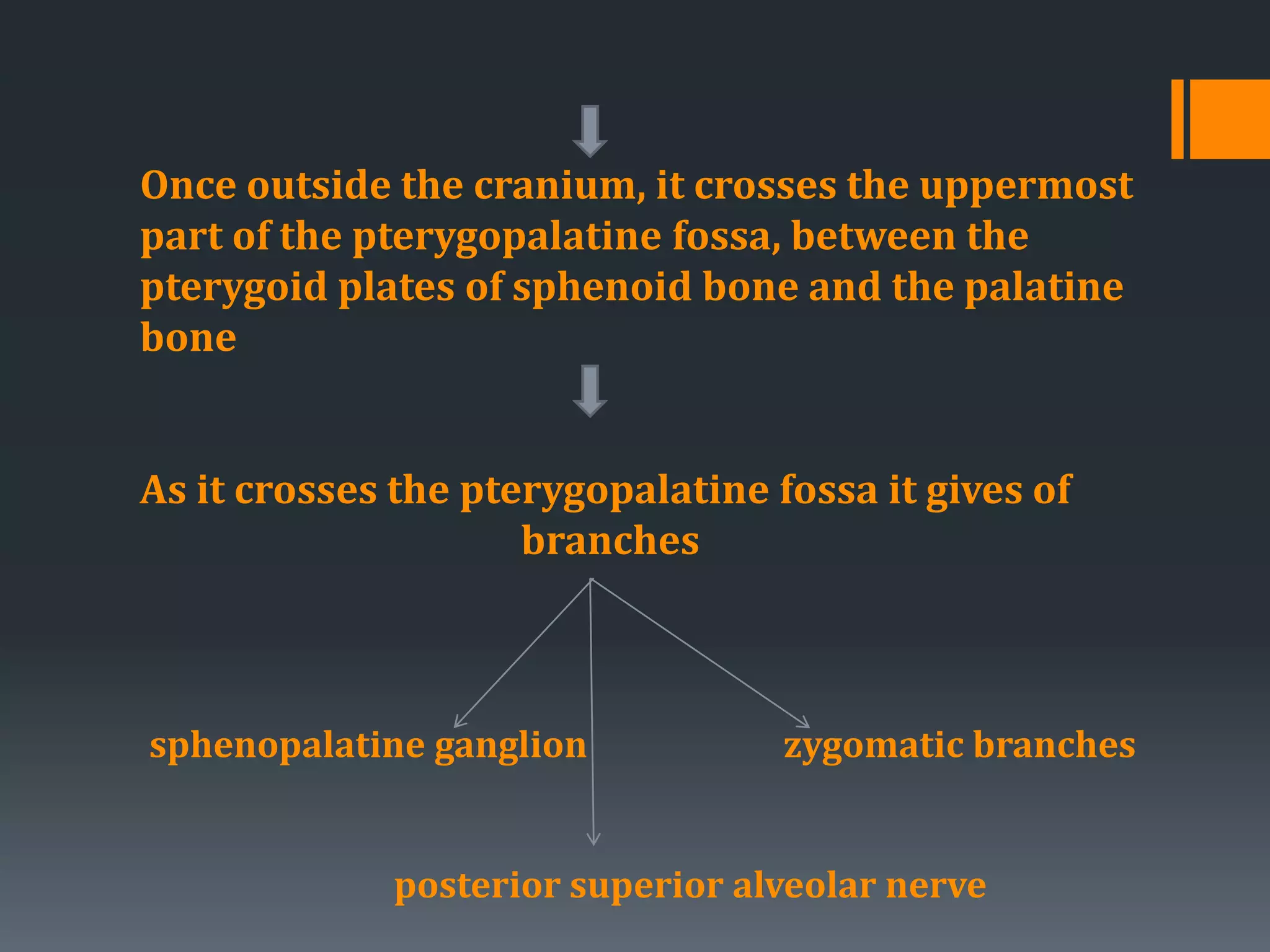
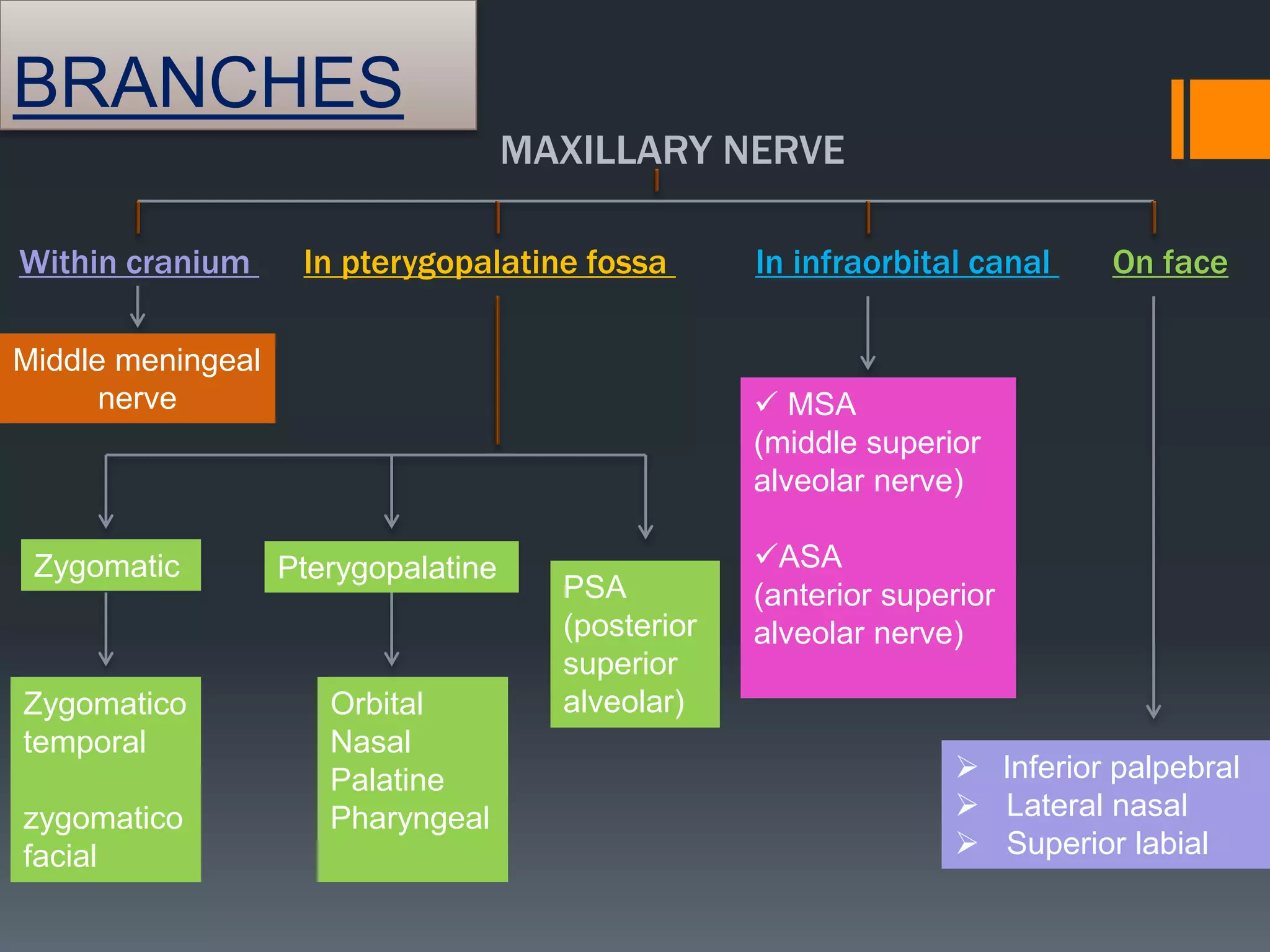
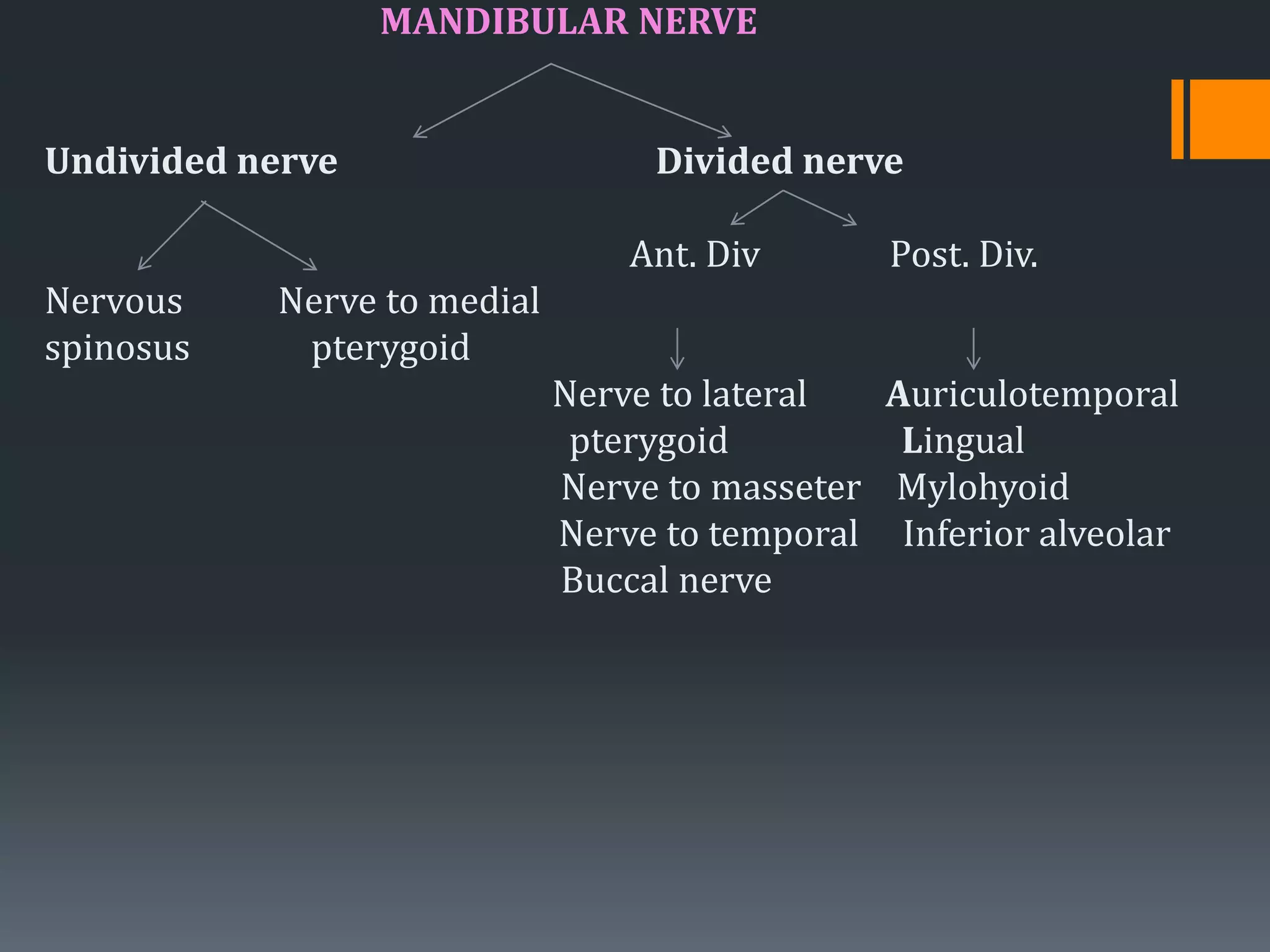
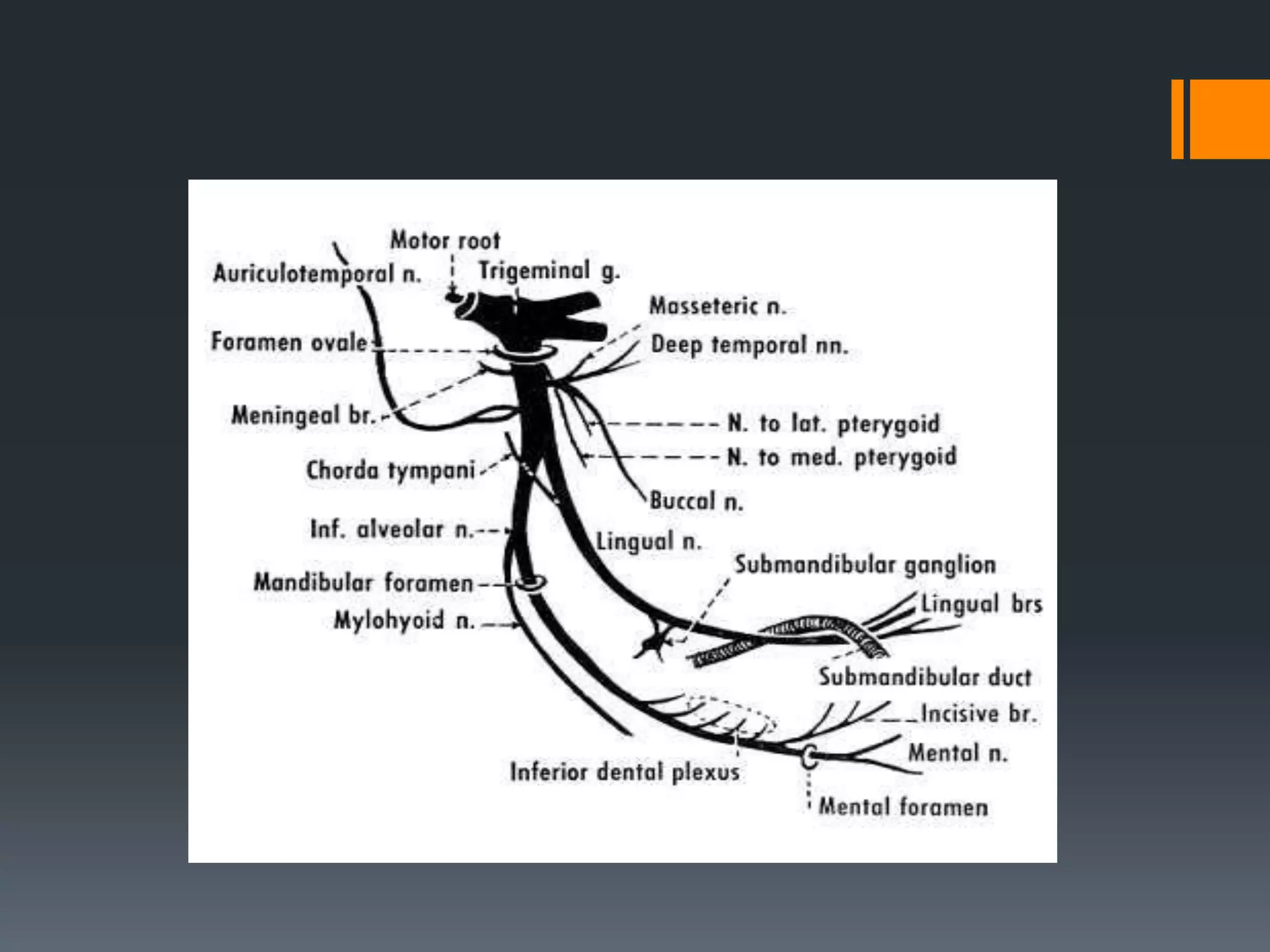
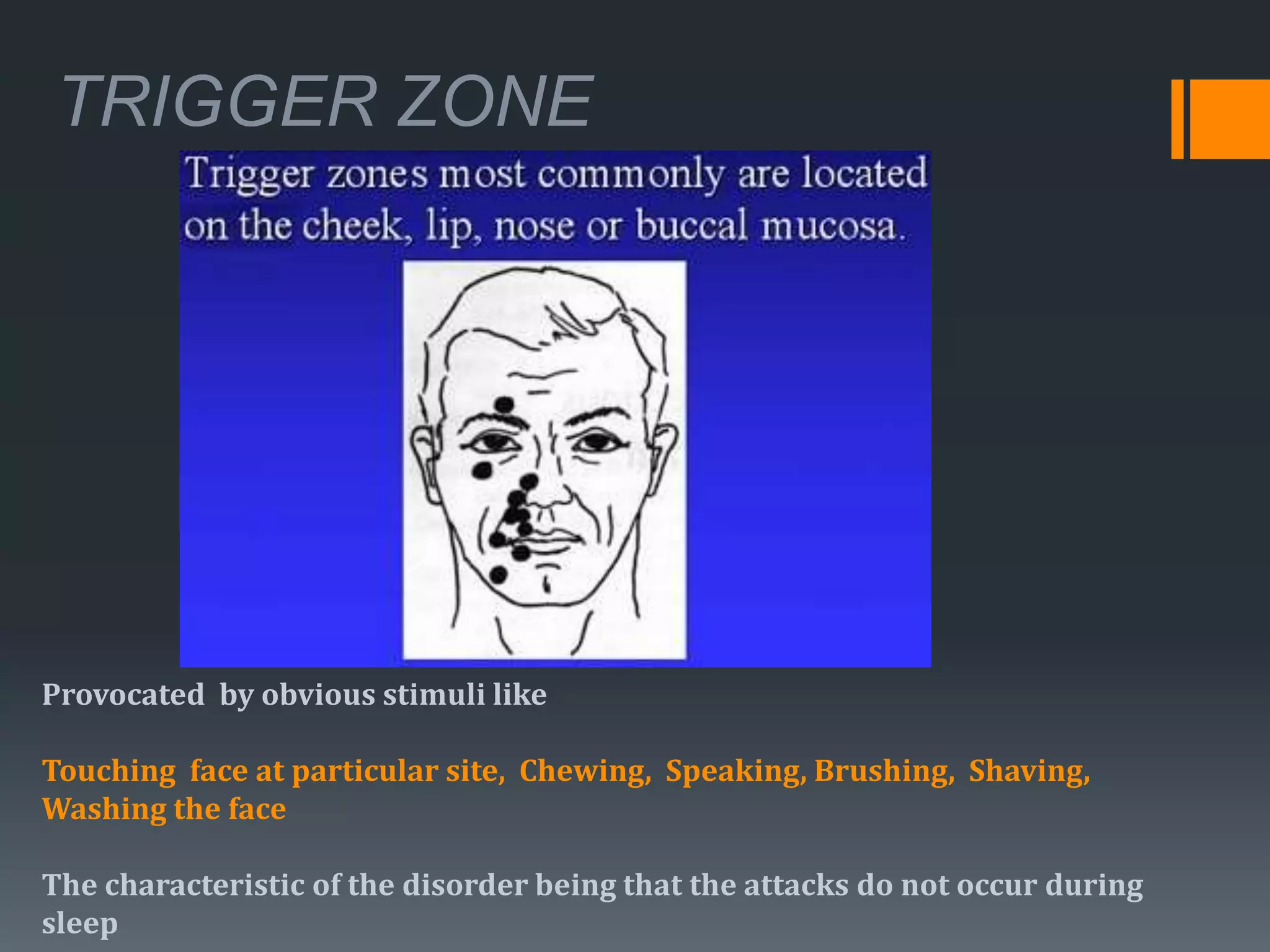
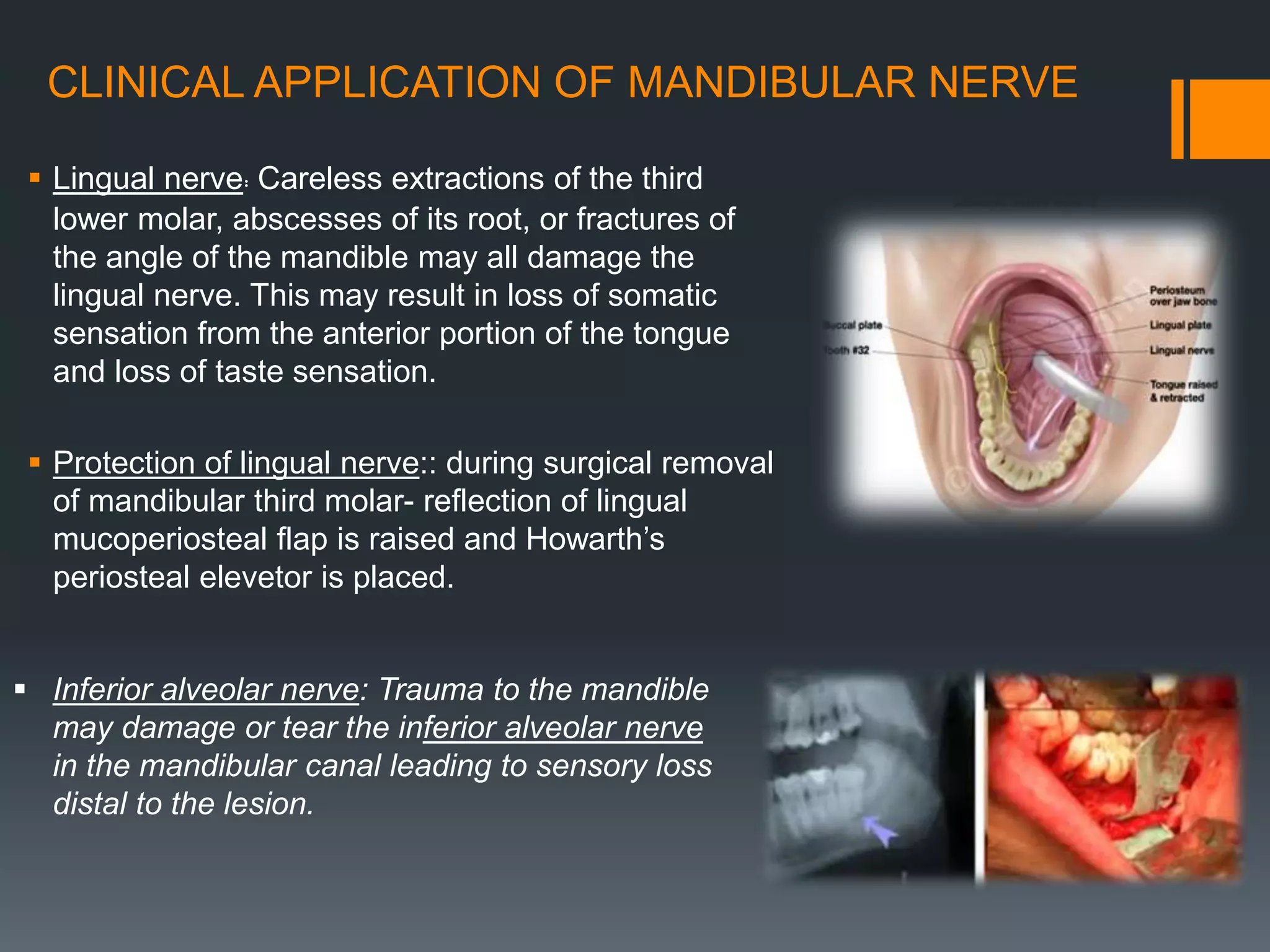
The trigeminal nerve is the fifth cranial nerve. It is a mixed nerve that carries motor and sensory fibers. It has three main divisions - the ophthalmic, maxillary, and mandibular nerves. The ophthalmic nerve innervates the upper face, the maxillary nerve innervates the mid face, and the mandibular nerve innervates the lower face and has both sensory and motor components. The trigeminal nerve is important for facial sensation and functions like chewing. It is also associated with conditions like trigeminal neuralgia.