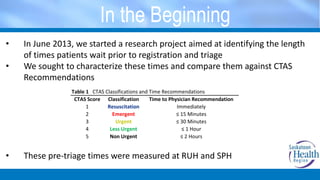
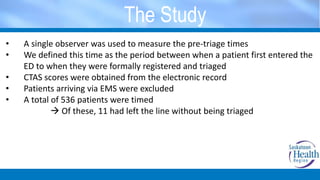
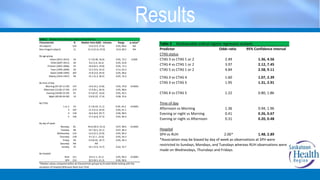
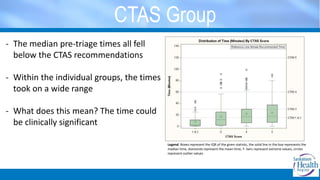
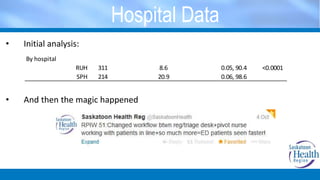
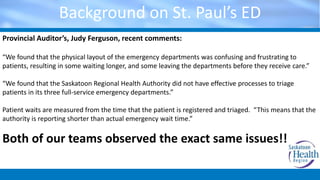
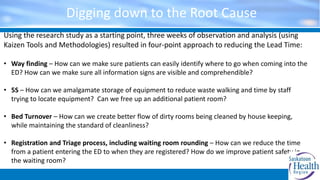
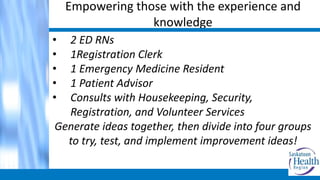
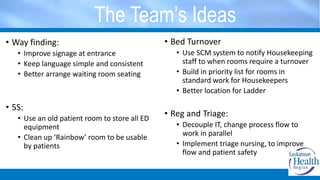
This document outlines a quality improvement project aimed at reducing emergency department wait times by translating academic research into practical solutions. Key findings showed significant issues with patient triage delays and through a rapid process improvement workshop, strategies were developed to enhance patient flow and safety. The project successfully reduced wait times and improved patient experience based on collaborative efforts involving medical staff and patient feedback.