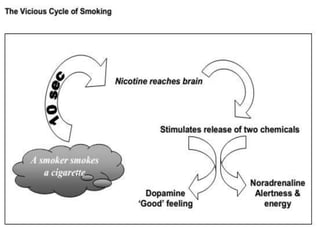
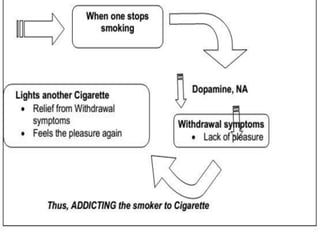
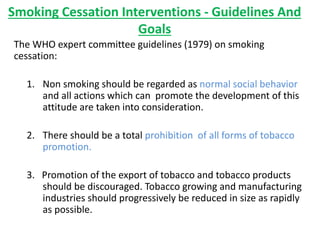
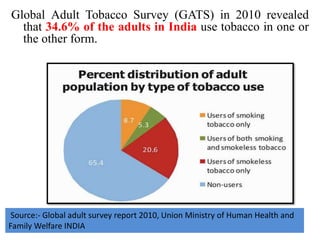
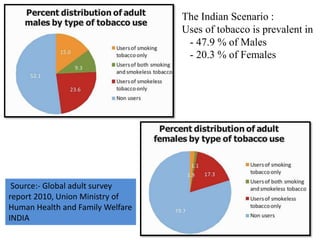
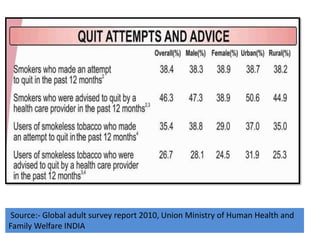
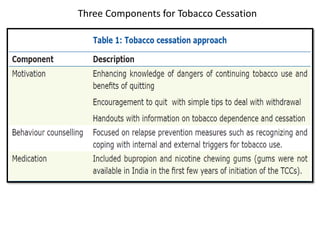
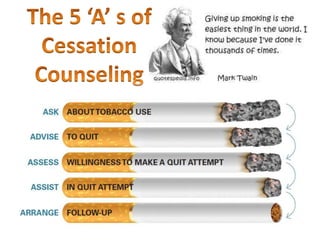
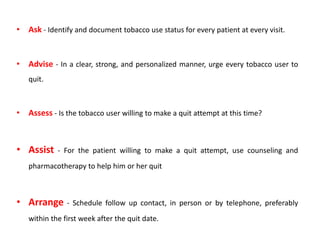
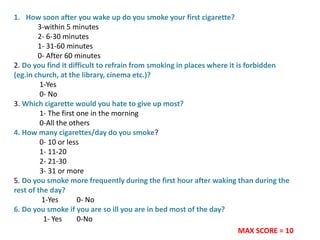
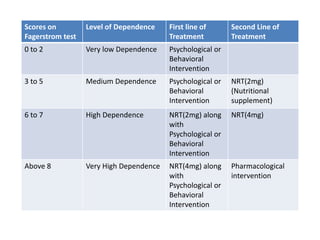
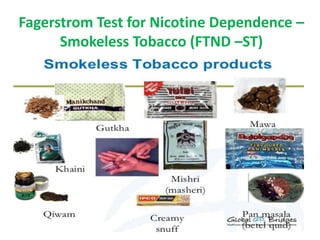
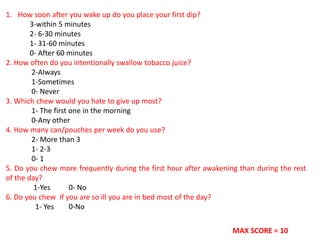
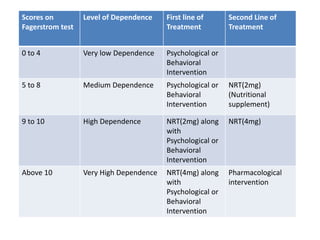
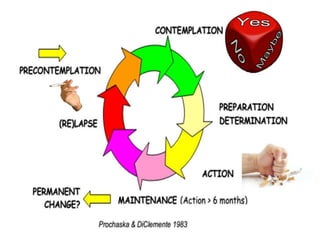
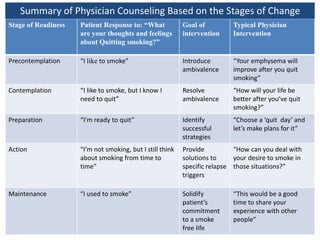
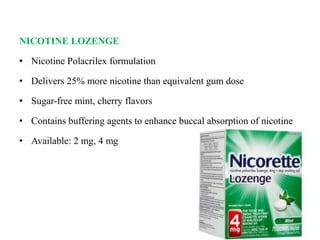
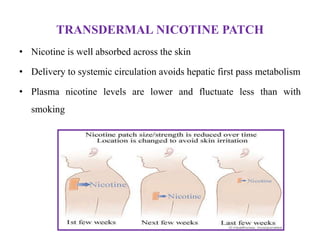
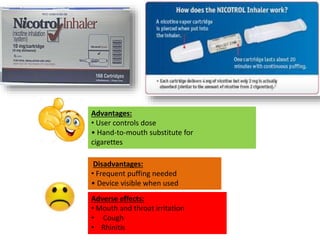
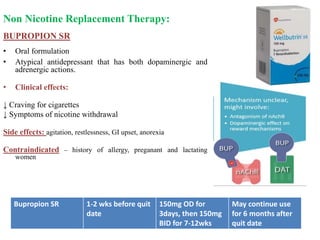
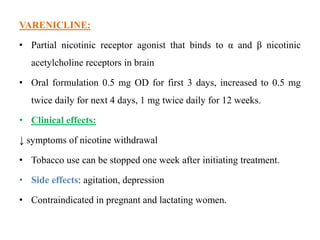
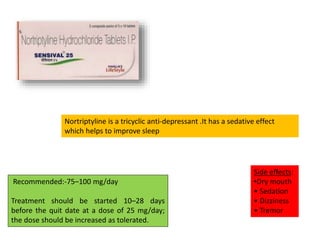
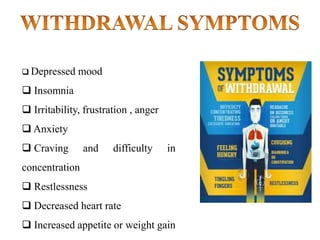
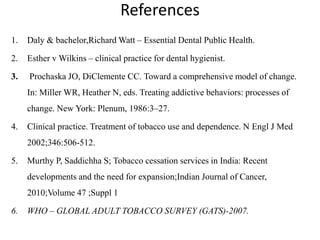
This document discusses guidelines for smoking cessation interventions and treatment. It outlines recommendations from the WHO and US Public Health Service on promoting non-smoking as the norm, prohibiting tobacco promotion, and reducing tobacco industries. The goals of smoking cessation treatment are achieving long-term abstinence, offering treatment to all tobacco users, and consistently identifying and treating tobacco use. Dental professionals can play a key role in educating patients and the community about the harms of tobacco and helping to enroll them in cessation programs. Assessment tools like the Fagerstrom Test and stages of change model are also discussed to guide treatment and counseling approaches. A variety of nicotine replacement therapies and non-nicotine medications are described for treating nic