This document provides information on a presentation about tobacco. Some key points:
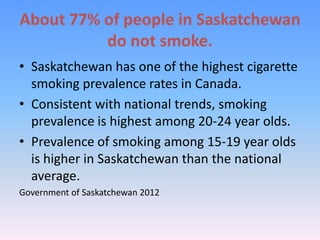
- Smoking remains a leading cause of preventable illness and death in Canada. Saskatchewan has high smoking rates, especially among youth.
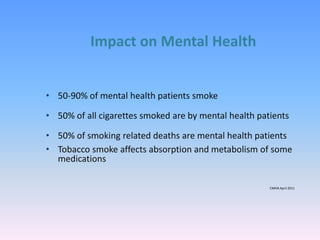
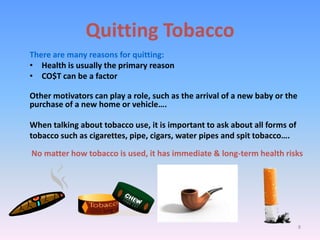
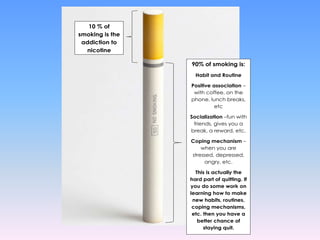
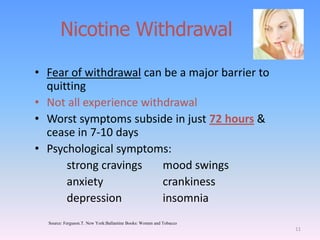
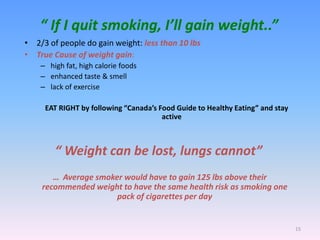
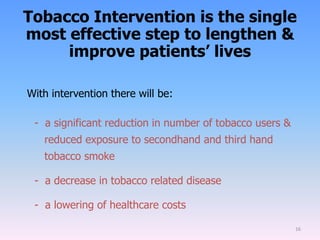
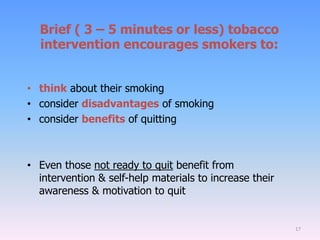
- Secondhand and thirdhand smoke harm others exposed to tobacco smoke. Quitting tobacco can be challenging due to nicotine addiction and behavioral factors.
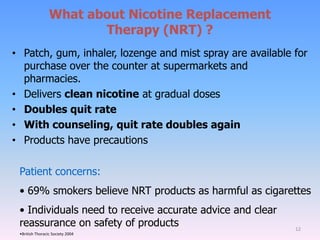
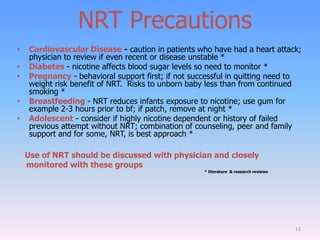
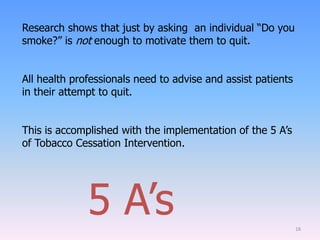
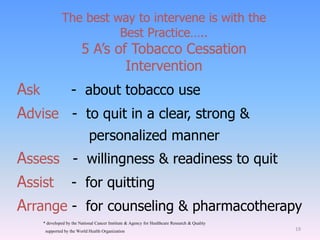
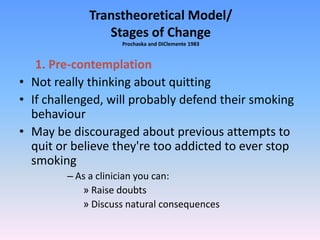
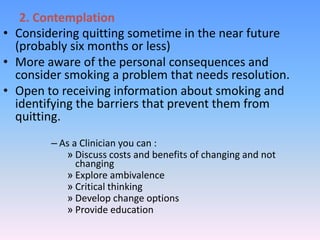
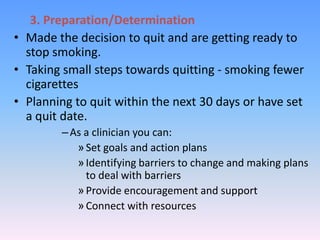
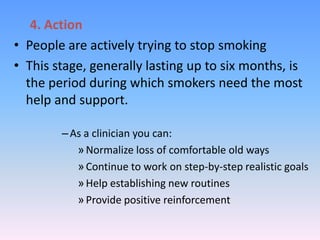
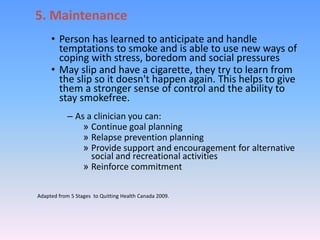
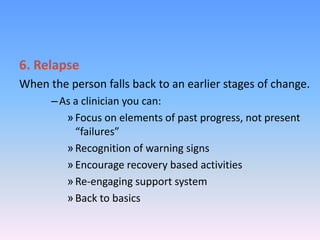
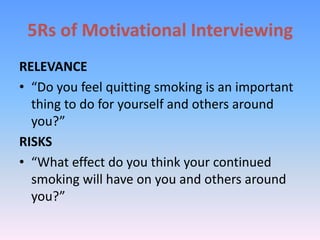
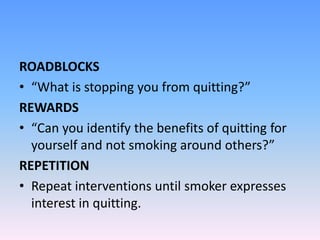
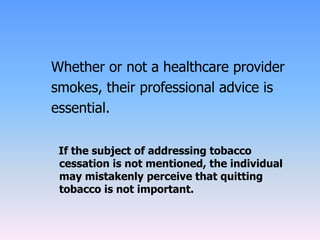
- Healthcare providers should use the 5 A's approach (Ask, Advise, Assess, Assist, Arrange) to counsel patients on quitting smoking. This involves discussing reasons to quit, barriers to quitting, and treatment options like nicotine replacement therapy.
- While some providers may hesitate to counsel patients due to their own smoking status,