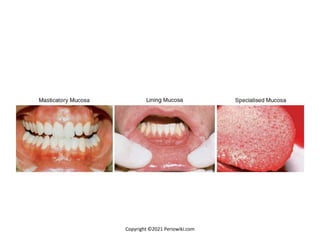
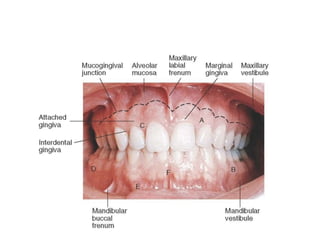
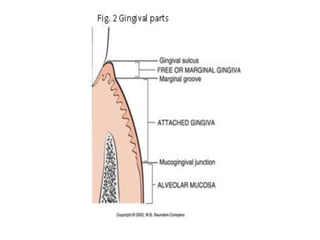
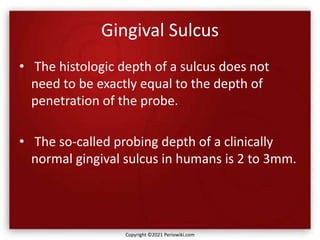
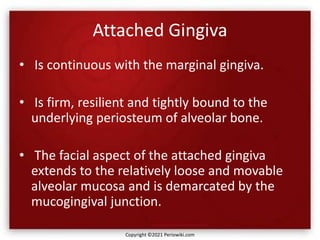
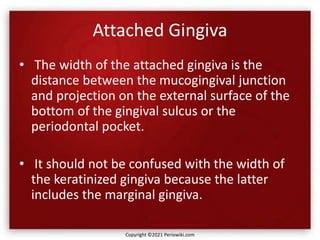
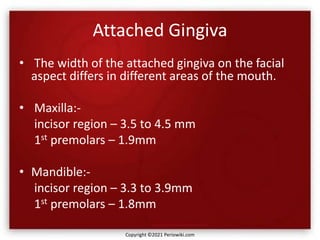
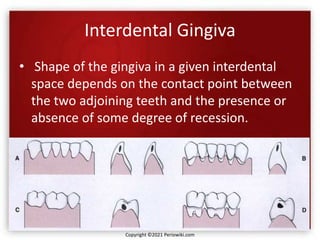
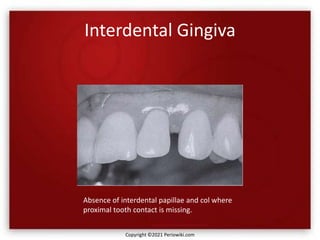
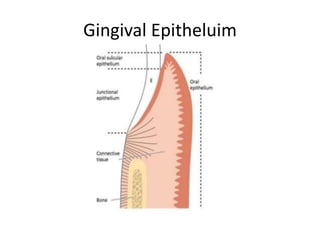
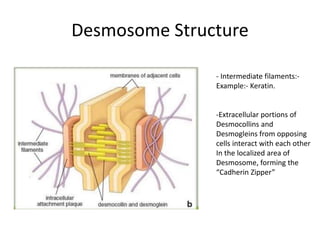
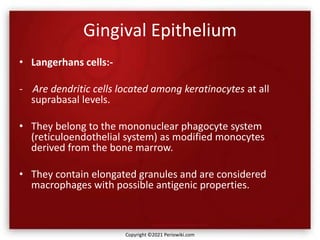
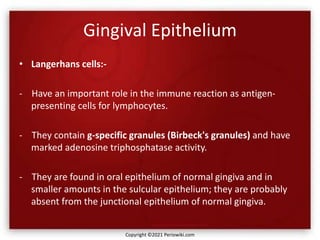
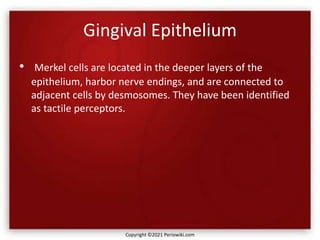
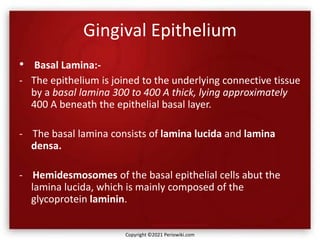
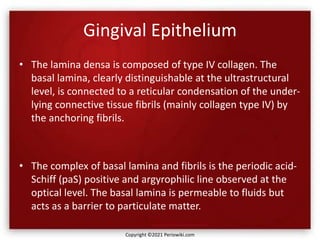
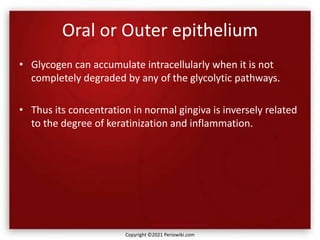
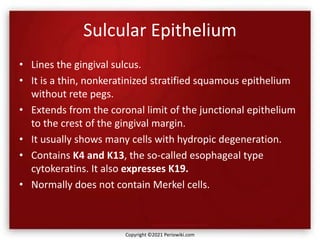
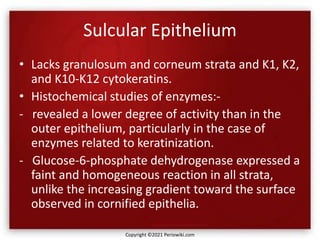
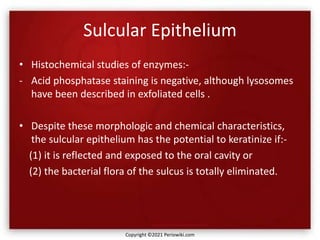
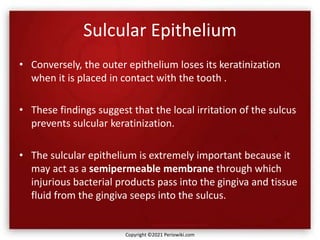
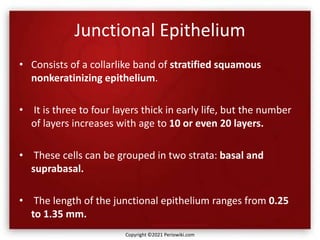
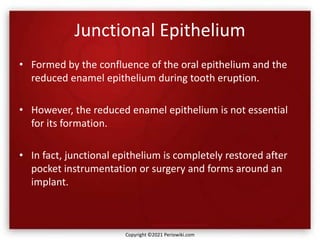
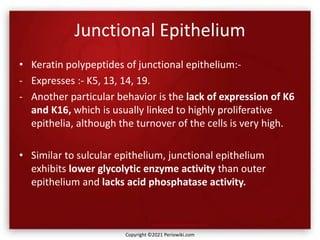
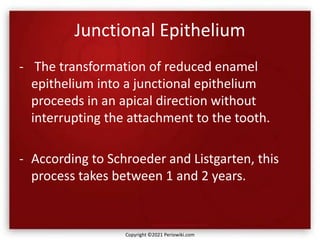
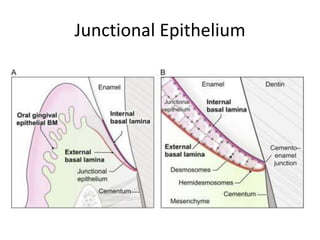
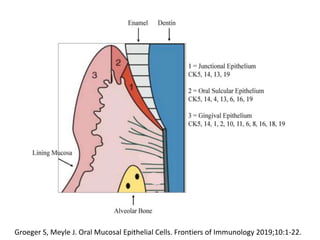
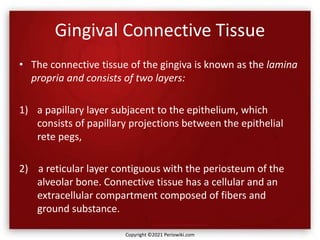
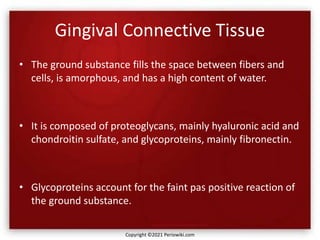
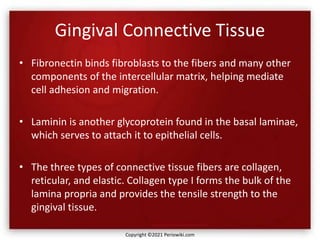
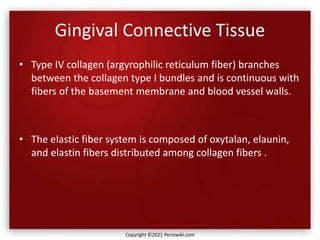
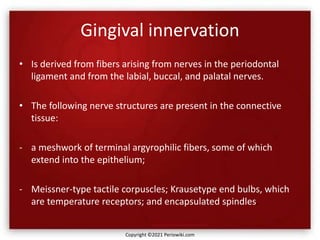
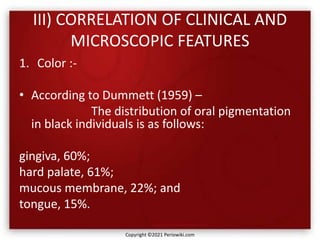
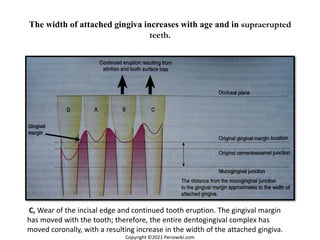
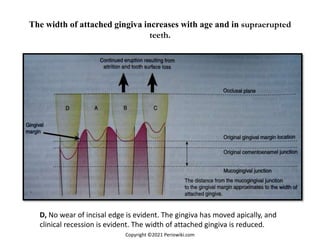
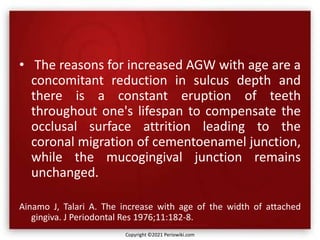
The document discusses the anatomy and histology of the gingiva. It describes the different types of gingiva - marginal, attached, and interdental gingiva - and their clinical and microscopic features. Microscopically, the gingiva consists of stratified squamous epithelium and connective tissue. The gingival epithelium undergoes proliferation and differentiation, including keratinization in some areas. Keratin proteins and other proteins important for epithelial maturation are also discussed.