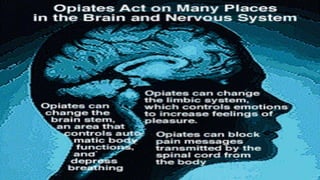
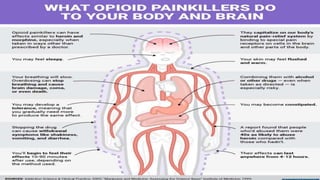
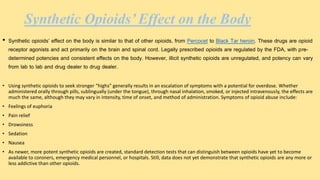
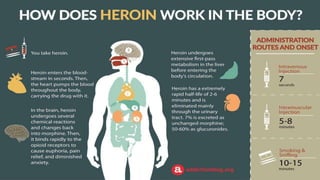
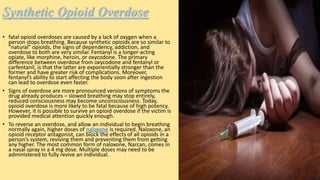
1) Synthetic opioids like fentanyl are much more potent than natural opioids like morphine and heroin. They work by binding to opioid receptors in the brain and spinal cord, triggering feelings of euphoria but also slowing respiration.
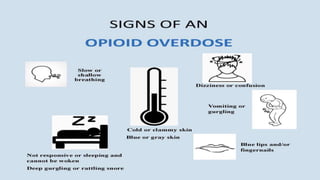
2) Synthetic opioids carry a high risk of overdose due to their potency and unpredictability. Overdose occurs when respiration slows to the point of stopping, depriving the brain of oxygen.
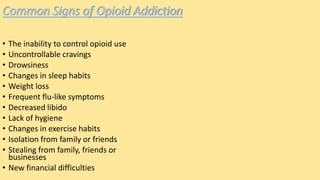
3) Signs of opioid addiction include an inability to control use, cravings, and changes in sleep, appetite, hygiene and social activities. Addiction results from the drugs' effects on the brain's reward pathways.






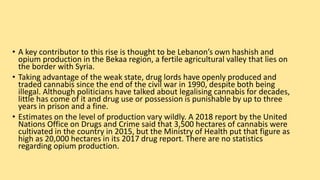
![• The health ministry also claims that hashish is sold for a little over $1 a gram, explaining in part why it is the
most popular recreational drug. The most common drugs seized by the authorities are cannabis, and the non-
locally-produced cocaine, Captagon and ecstasy. The latter are smuggled through the airport or the porous
Syrian border.
• Captagon, sometimes referred to as “chemical courage”, made headlines when it became popular among
fighters in the Syrian civil war – it is considered to improve alertness and combat effectiveness
• Despite drug usage being common, it remains stigmatised by Lebanese society and the media. This week,
Lebanese daily Al Akhbar reported that a 70-year old pharmacist in Beirut was attacked by a drug addict wanting
tramadol, an opioid-based painkiller. A former heroin user told us that when heroin is unavailable users turn to
tramadol, which is known as farawla, or strawberry, in Lebanese Arabic because of the pill’s red colour.
• Heroin is cheap, however, costing between $10 and $30 a gram, making it popular among the working class, but
its usage is more heavily stigmatised than cocaine.
• “Some people start with coke and run out of money and turn to heroin. I don’t like it [heroin] – it is dirty”, said
Fadi – who did not want to give his full name – 34, a regular cocaine user from Beirut’s southern suburb of
Dahieh.
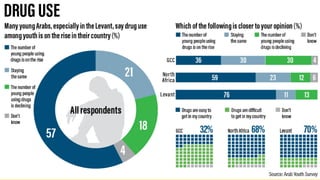
• The Arab Youth Survey found that in most cases, drug consumption begins with encouragement from friends,
and a number of recreational drug users who spoke to The National agreed.
• Fadi said that he started taking cocaine to stay awake while consuming large quantities of alcohol. “Now every
time I go to a club, I can’t enjoy it without coke,” he said.](https://image.slidesharecdn.com/syntheticopioidsinarab2-200509182849/85/Synthetic-opioids-in-arab-2-42-320.jpg)

![UAE's new online prescription platform to tackle drug abuse
• A new online platform for drug prescriptions is set to be rolled out across the UAE as part of efforts to
clamp down on substance abuse.
• From Monday, any patient requiring controlled opioids such as morphine will have their full details logged
on a single database accessible by medics across the country.
• The move aims to prevent individuals from obtaining multiple doses of highly addictive drugs by seeking
the same prescription from both government and private hospitals in the UAE.
• Experts hope the change will prevent drug abuse - for example - from patients who could approach more
than one doctor to obtain potentially dangerous repeat prescriptions.
• “The main objective is to ensure greater control over the prescription and dispersal of narcotic drugs and
controlled medicines,” said Dr Khaled Al Jaberi, of the Department of Health.
• “[This is] with a view to reducing the illegal use of controlled medicines among the community and to
promote the safety of their use to their intended beneficiaries only.
• “The new platform will also reduce inefficiencies caused by the loss of paper prescriptions in addition to
ensuring accurate tracking of prescriptions and dispersal of drugs and controlled medicines at state level.”](https://image.slidesharecdn.com/syntheticopioidsinarab2-200509182849/85/Synthetic-opioids-in-arab-2-47-320.jpg)
![• The new system - called the Unified Electronic Platform - was led by the Ministry of Interior in co-
operation with the Ministry of Health and Abu Dhabi Department of Health.
• It aims to combine all of the country’s private and government sector outpatient healthcare facilities
into a single database.
• Patients will no longer be able to have repeat doses prescribed to them from multiple doctors across
multiple hospitals or emirates.
• Instead, information on their medication needs will be available to all healthcare facilities, allowing
doctors to prevent unwarranted prescriptions.
• The change of policy will also see an end to paper prescriptions for controlled substances which can be
lost or even stolen, sometimes resulting in drugs falling into the wrong hands.
• “If the patient goes to any other clinic or physician for the same medication, the system will clearly
show that he or she has an active prescription and has just received his medication,” said Dr Al Jaberi.
• “So there will not be an oversupply of medications. We are sure it will result in a lower number of
prescriptions.
• “We can also now monitor numbers of prescriptions, doctors who have prescribed them, where they
[patients] are getting their prescriptions from, type of medications and so on.
• “We can access all the information and prevent any abuse. This is one of the biggest and most
important initiatives to control [drug abuse].](https://image.slidesharecdn.com/syntheticopioidsinarab2-200509182849/85/Synthetic-opioids-in-arab-2-48-320.jpg)