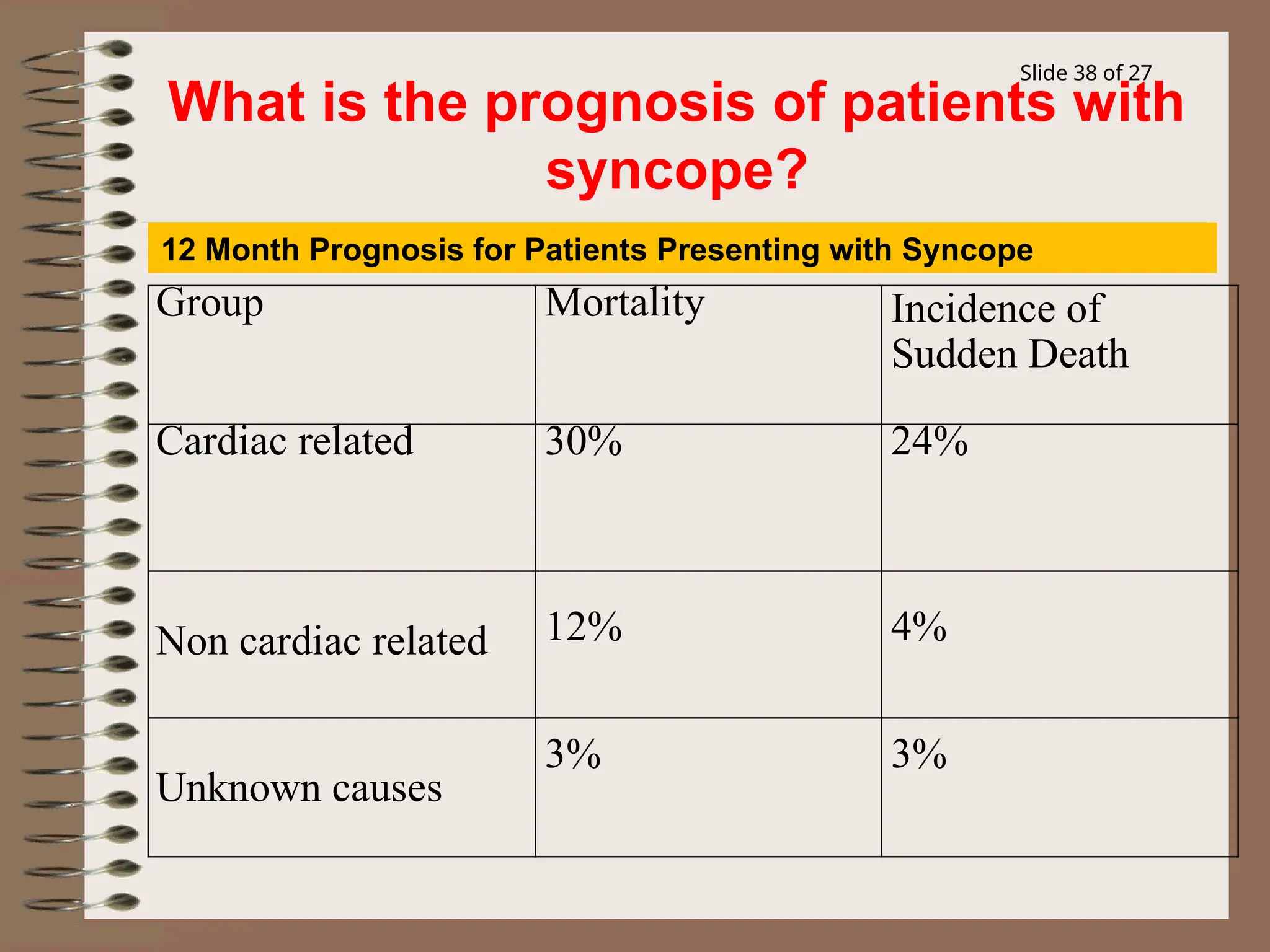
Syncope, or fainting, is a temporary loss of consciousness caused by reduced blood flow to the brain, often resolving spontaneously. It can result from various factors, including vasovagal responses, heart conditions, or neurological issues, with treatment depending on the underlying cause. While it is common, especially in older adults, proper diagnosis and management are essential to prevent more serious health concerns.