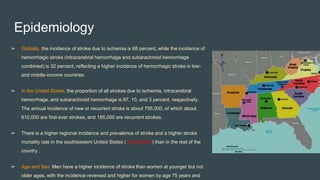
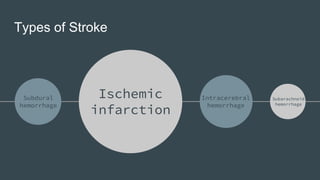
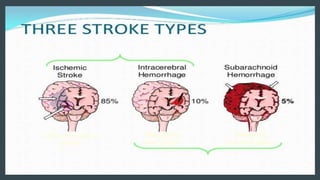
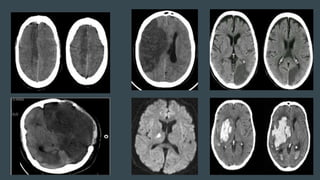
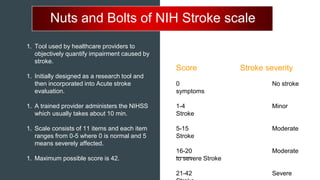
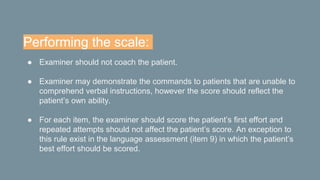
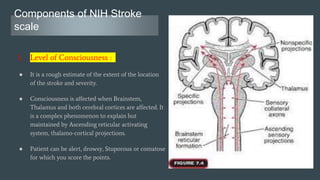
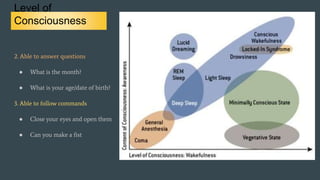
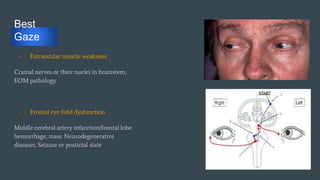
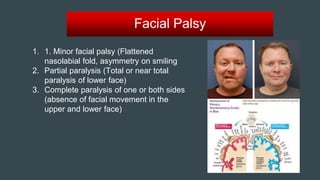
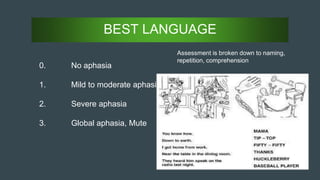
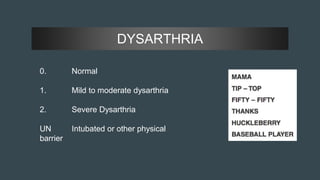
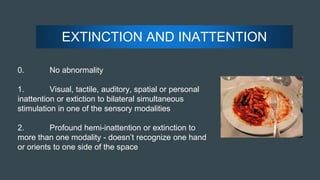
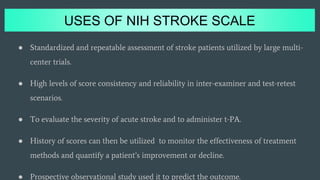
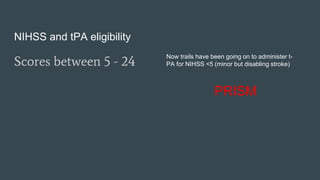
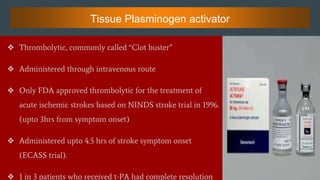
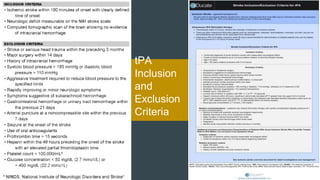
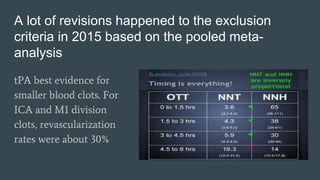
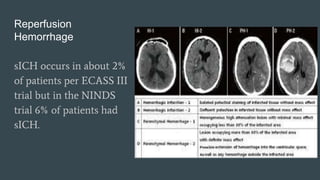
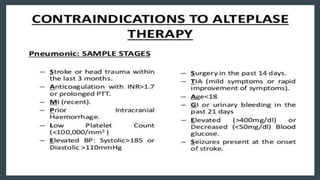
The document discusses stroke classification, with ischemic strokes being more prevalent than hemorrhagic strokes globally. It outlines the NIH Stroke Scale, a tool for assessing stroke severity, and the criteria for administering tissue plasminogen activator (t-pa) in acute ischemic strokes. Lastly, it highlights the epidemiology of strokes, including incidence rates, demographic influences, and management strategies.