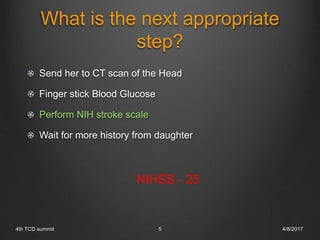
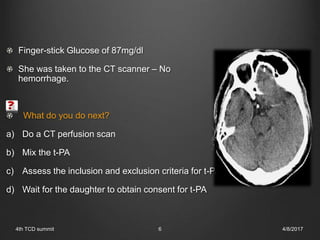
1) A 54-year-old woman presented with sudden onset right-sided weakness and inability to speak, with a history of a prior TIA. Initial assessment found a NIH stroke scale score of 25 and blood glucose of 87 mg/dL.
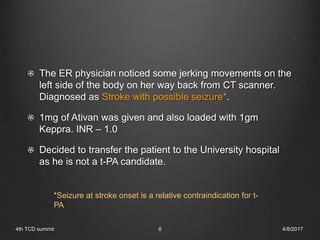
2) CT scan showed no hemorrhage. CT angiogram then revealed an occlusion of the left middle cerebral artery. The patient received tPA and was taken for mechanical thrombectomy.
3) She was admitted to the neurosciences intensive care unit. She improved significantly with treatment and was discharged with a modified Rankin score of 0 at 90 days.