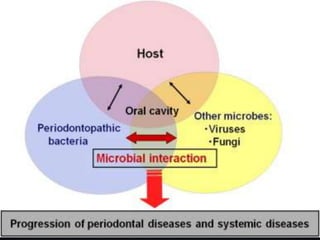
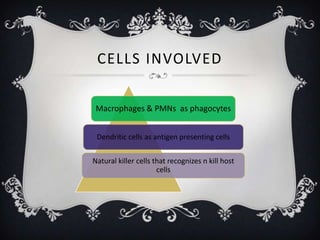
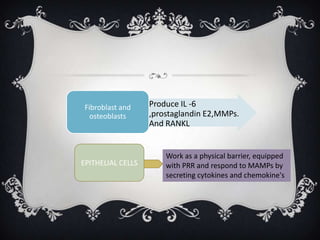
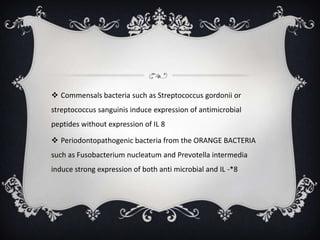
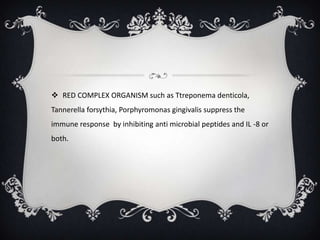
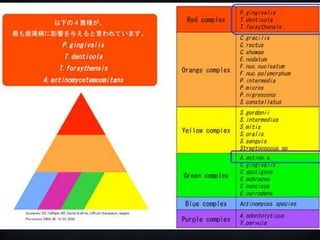
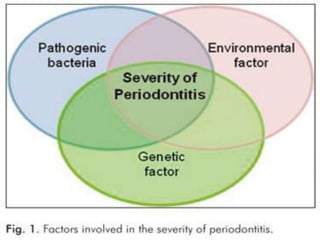
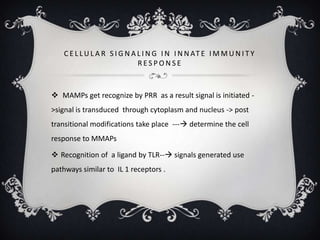
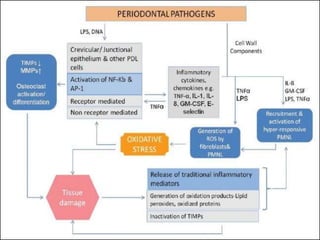
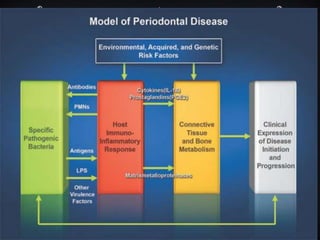
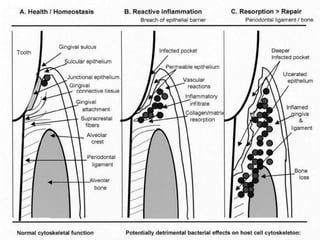
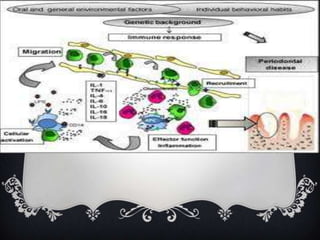
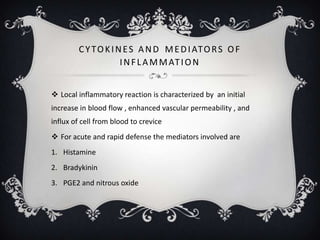
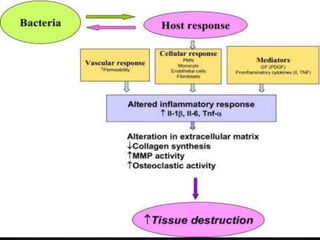
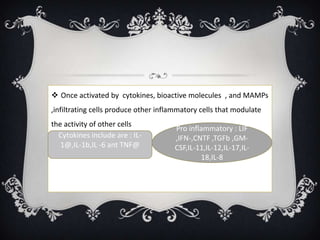
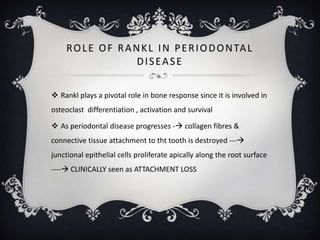
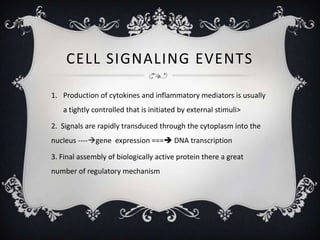
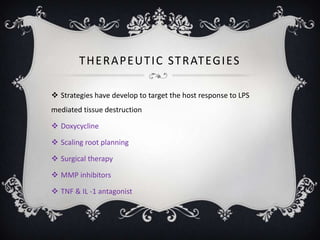
This document provides an overview of the molecular biology of the host-microbe interaction in periodontal disease. It discusses how the innate immune system recognizes microbes via pattern recognition receptors like TLRs. It also describes how innate immunity initiates and modulates the adaptive immune response. Key aspects of the pathogenesis of periodontal disease are explained, including the roles of pro-inflammatory cytokines, RANKL signaling, and MMPs in degrading periodontal tissues. Host genetic variations and intracellular signaling pathways are also discussed in modulating susceptibility to periodontal disease.