This document provides an overview of sexually transmitted diseases (STDs), including their causes, symptoms, screening, diagnosis, treatment, and prevention. Some key points:
- STDs are passed through sexual contact or other bodily fluids and sometimes from mother to child. Many show no symptoms but can cause complications if left untreated.
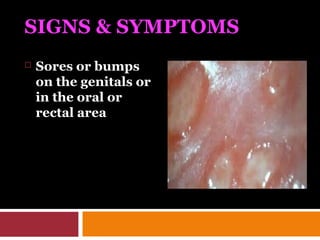
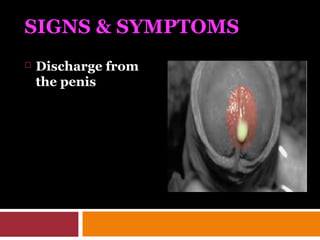
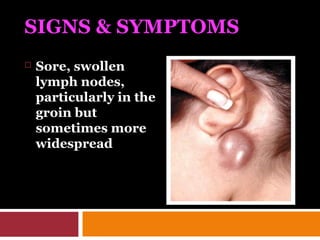
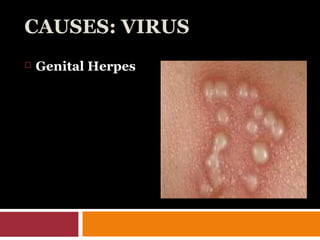
- Symptoms vary by infection but may include sores, discharge, pain, rashes, or bleeding. Regular screening is recommended for those with multiple partners or in high risk groups.
- Common bacterial and viral STDs include chlamydia, gonorrhea, herpes, HIV, and HPV. Screening includes blood/urine tests and fluid samples.
-