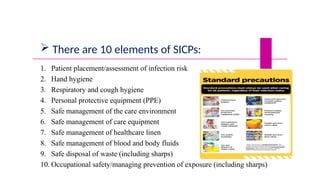
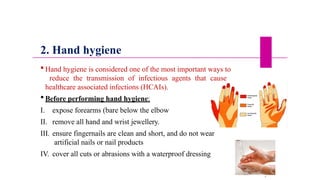
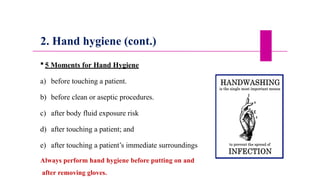
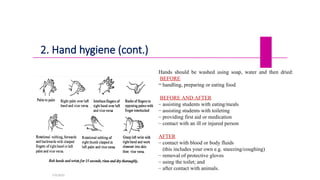
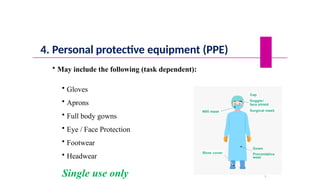
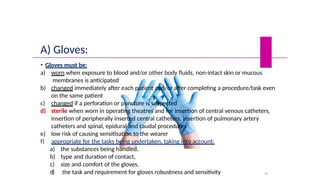
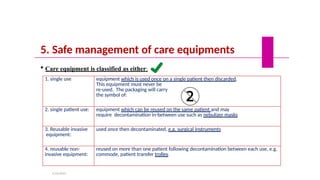
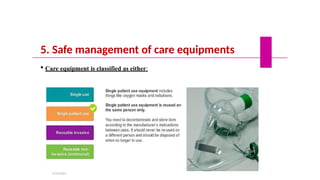
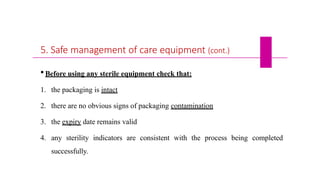
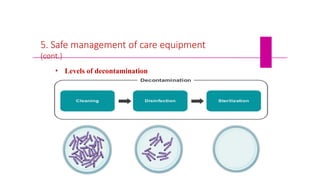
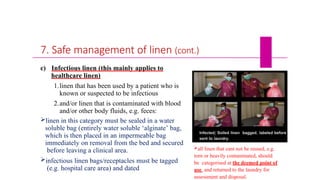
The document outlines Standard Infection Control Precautions (SICPs) essential for preventing the transmission of infectious agents in healthcare settings. It details ten key elements of SICPs, including proper hand hygiene, the use of personal protective equipment (PPE), and effective management of care equipment and environments. The document emphasizes adherence to these precautions by all healthcare staff at all times to ensure safety for patients, staff, and visitors.