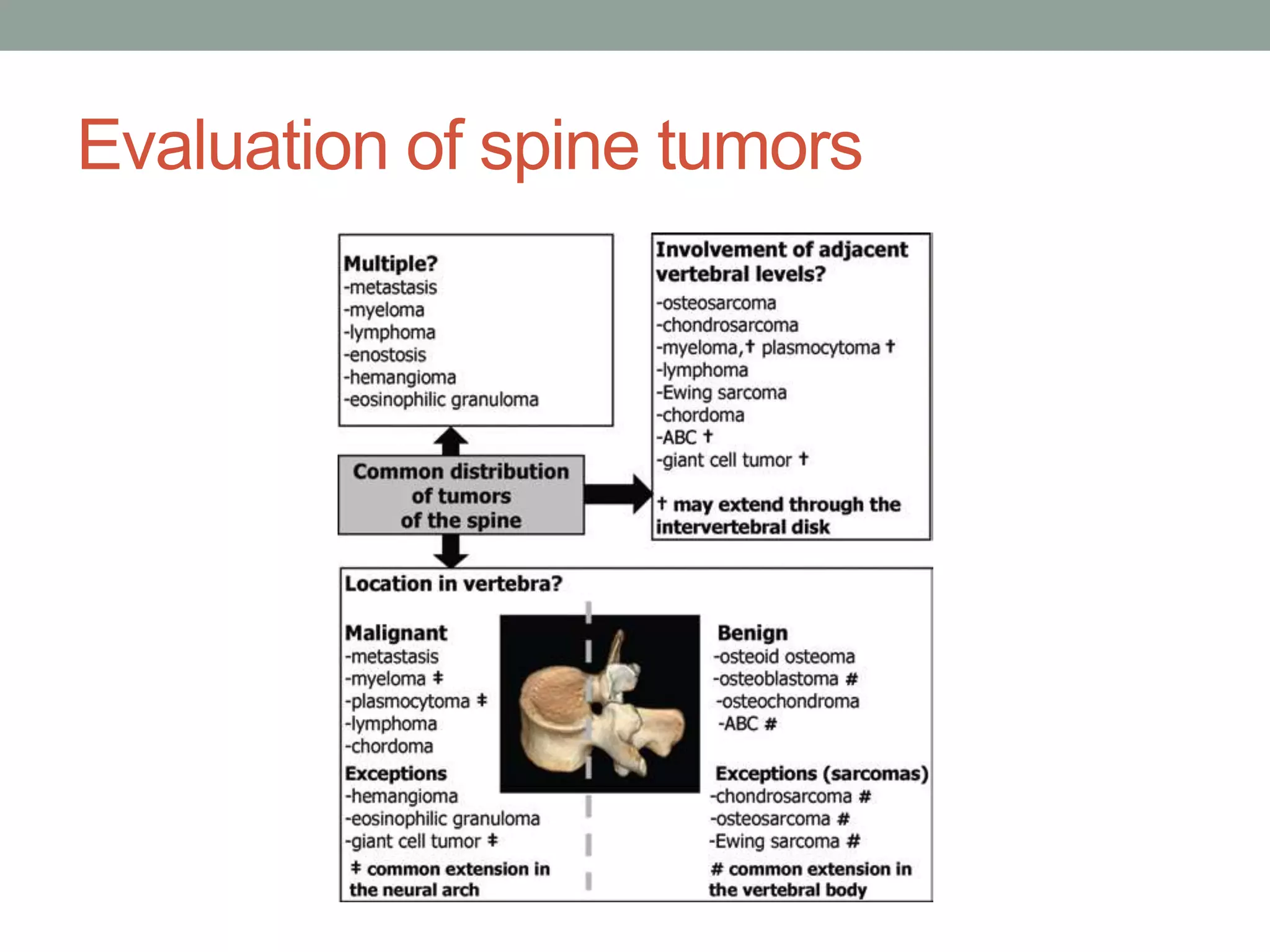
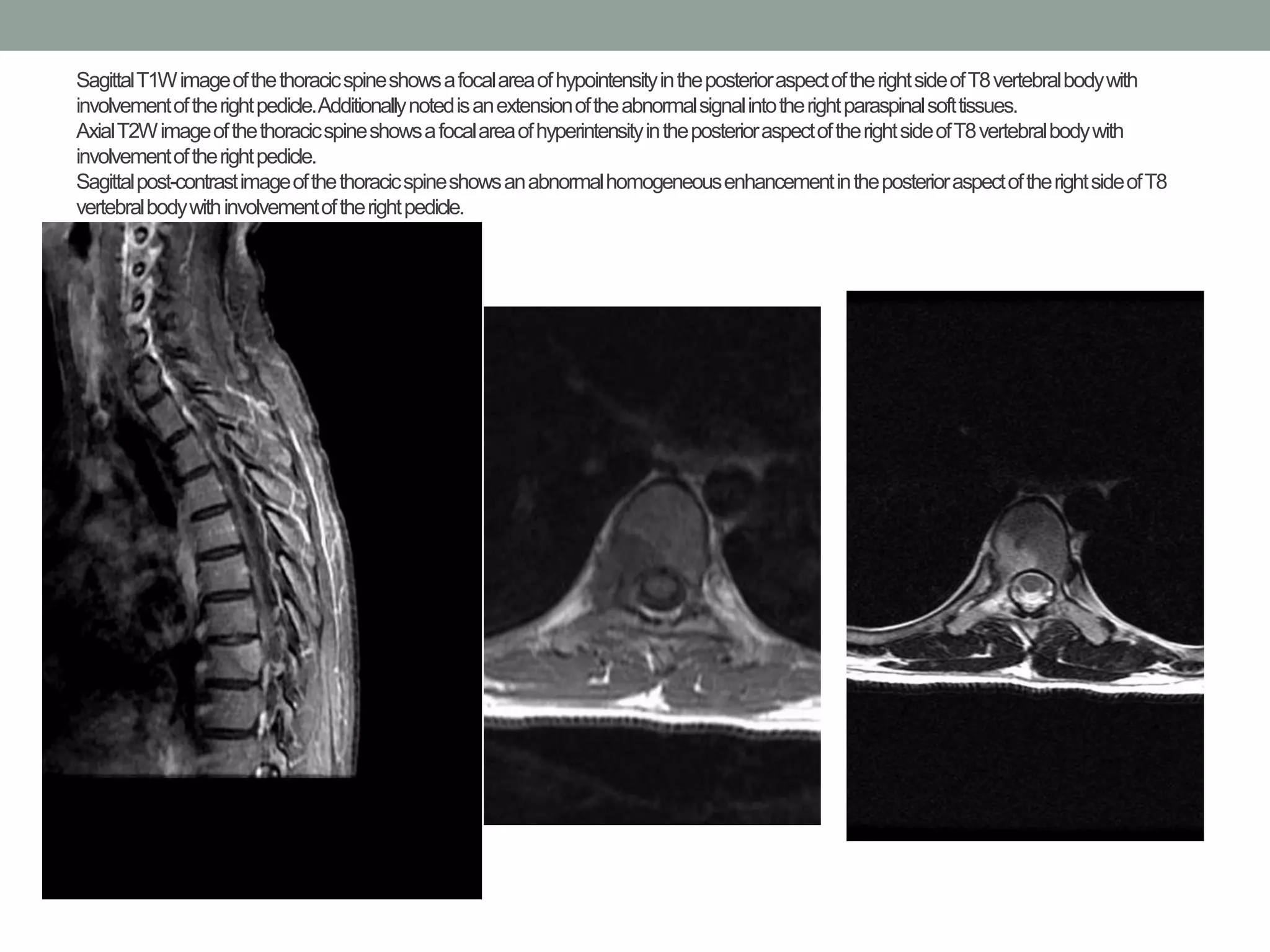
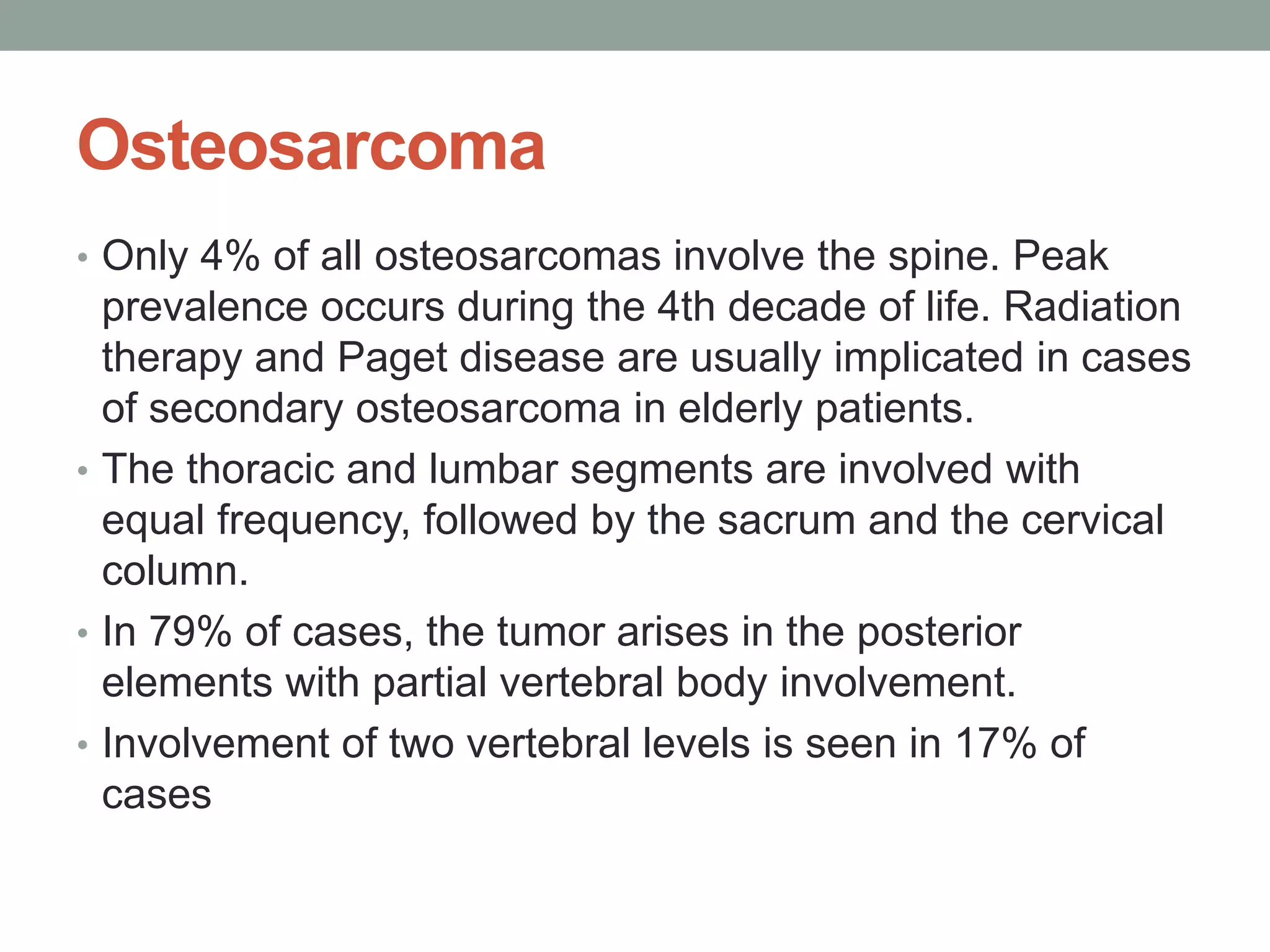
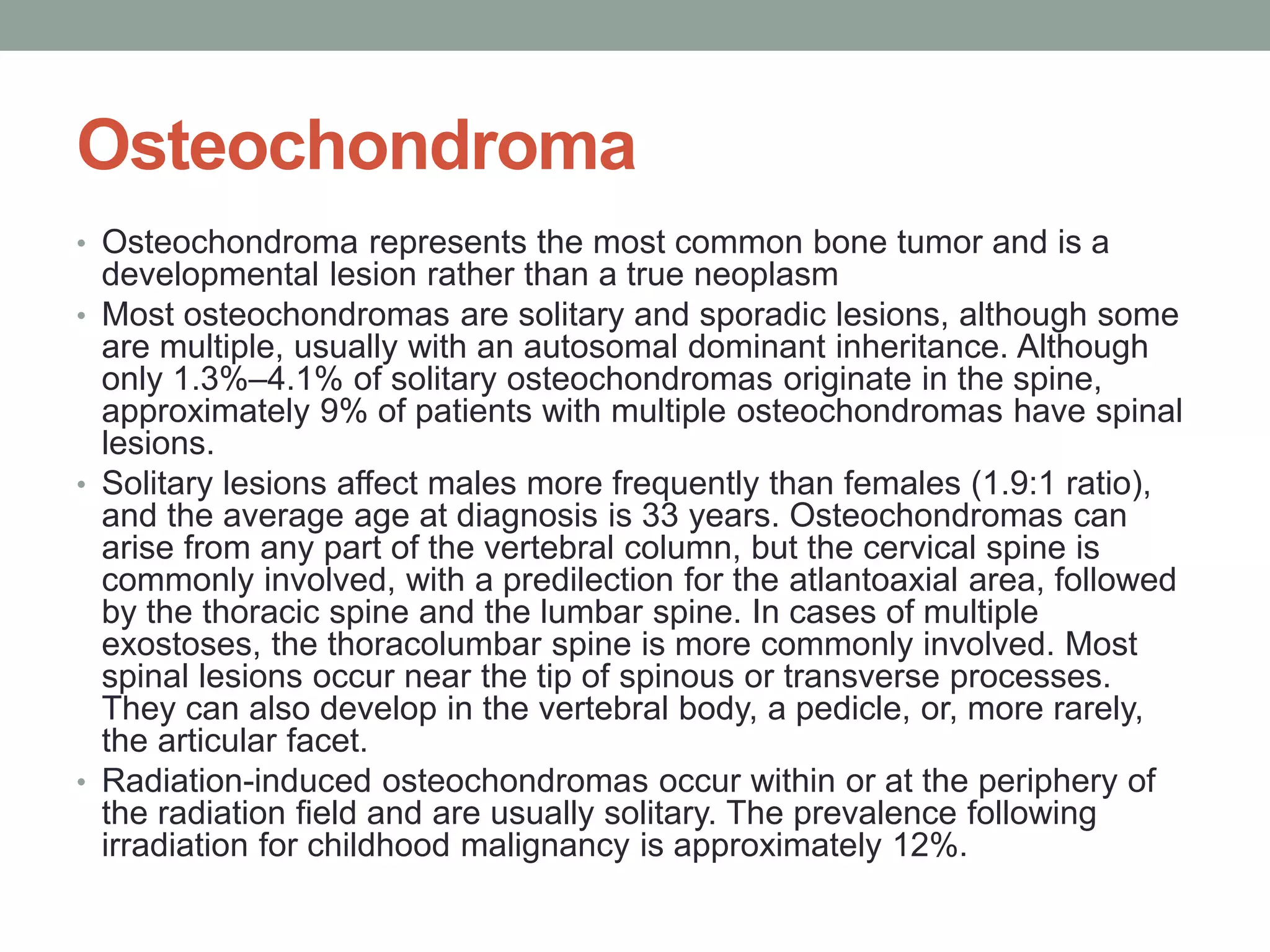
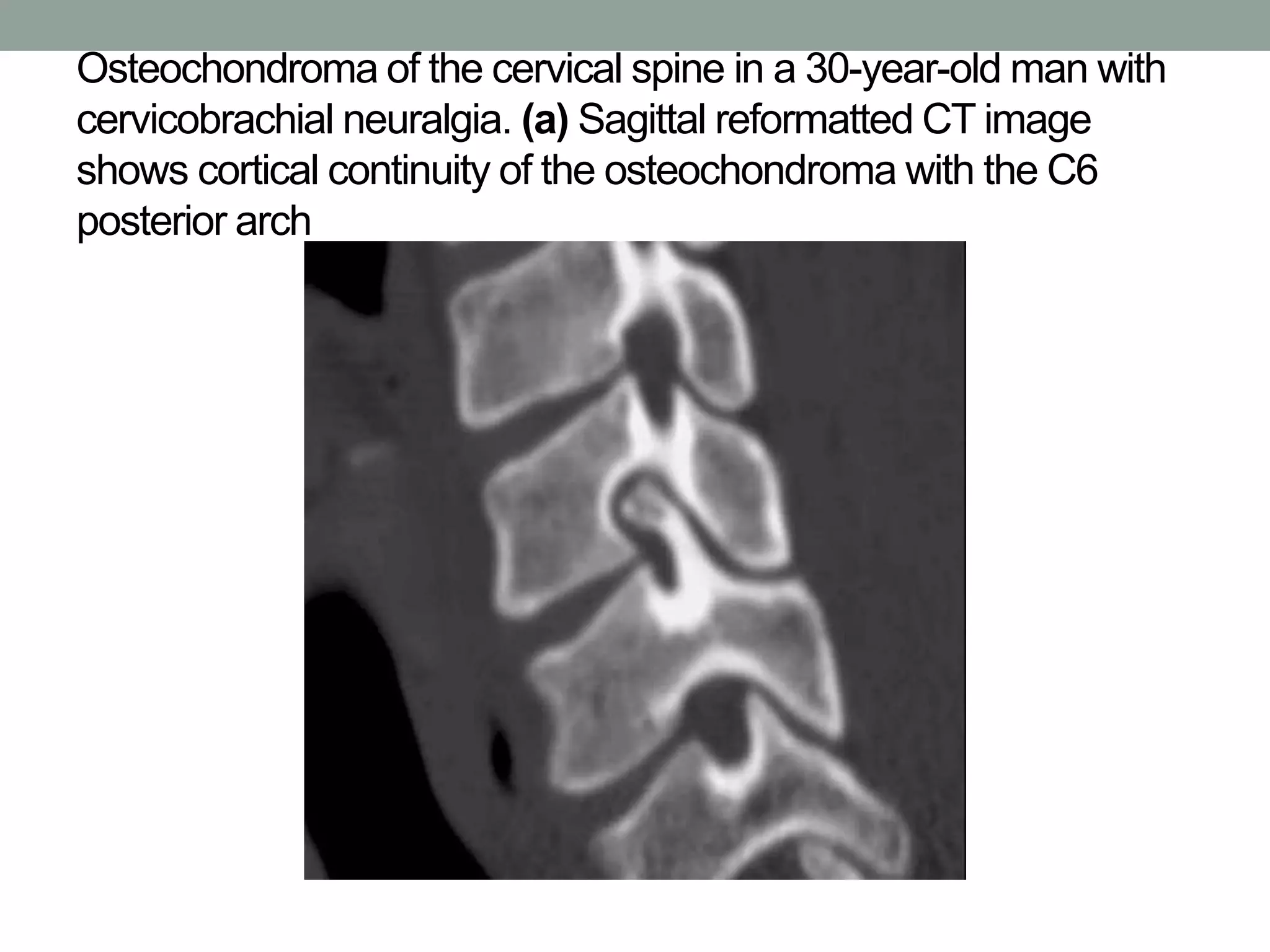
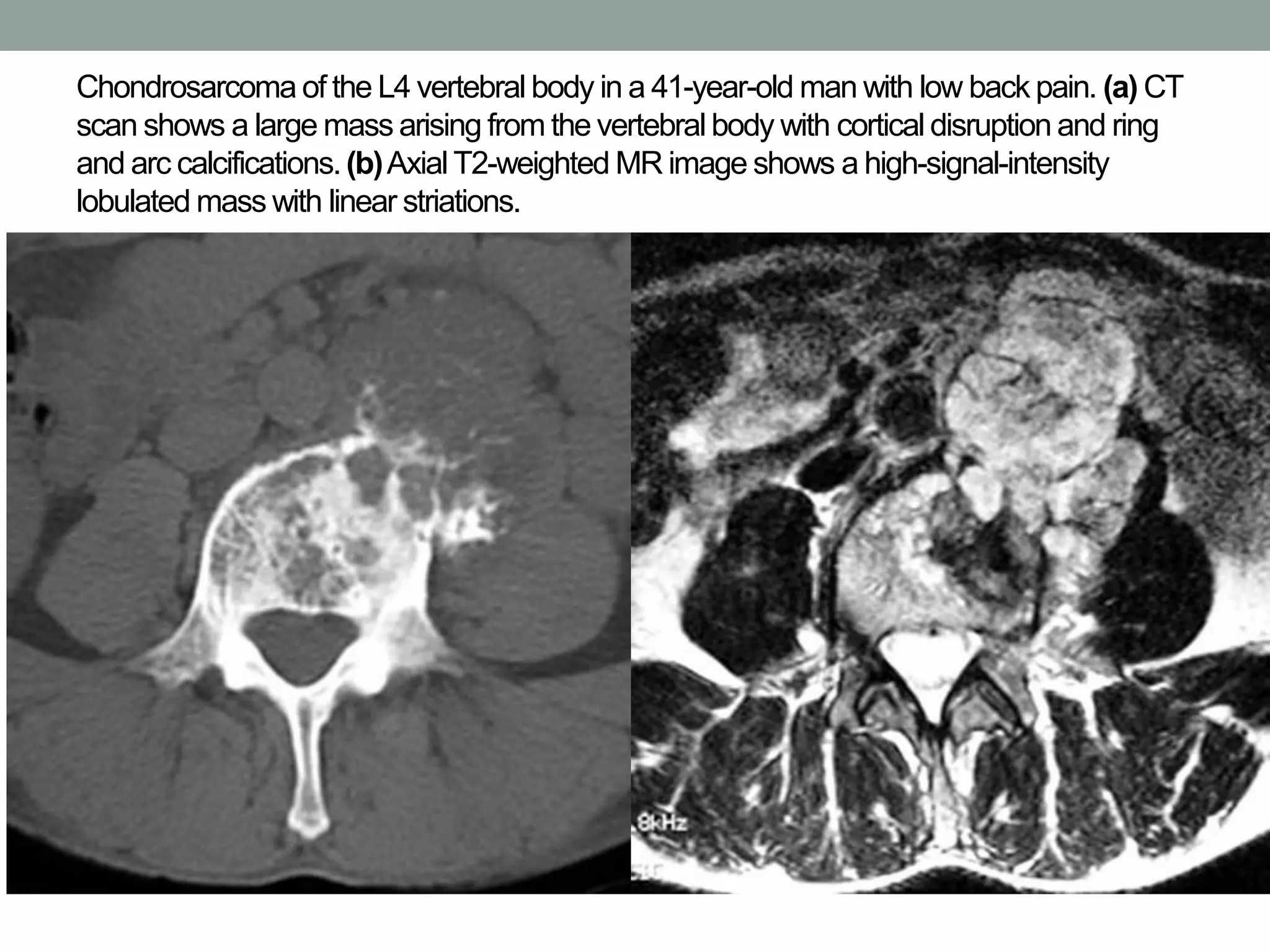
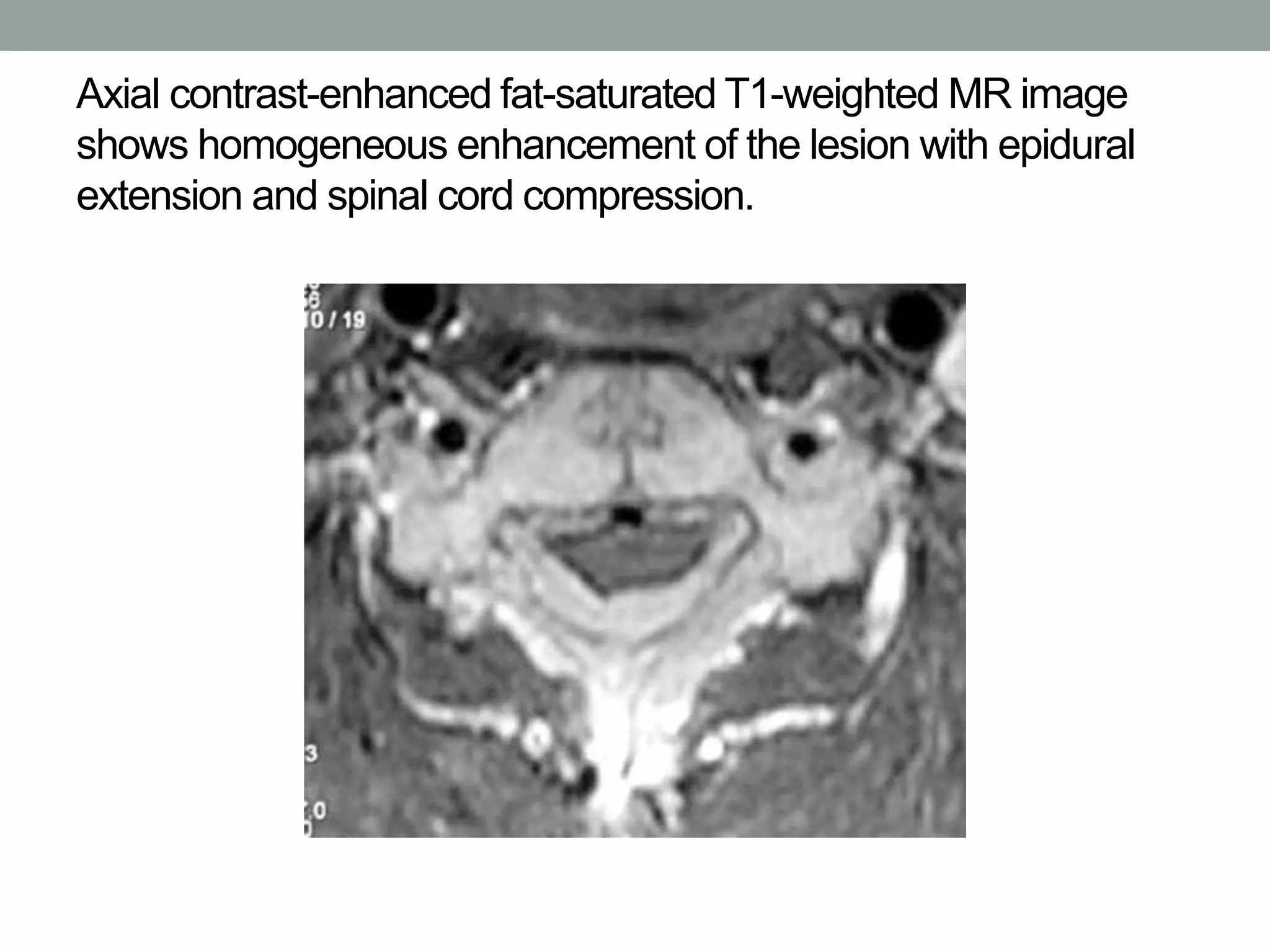
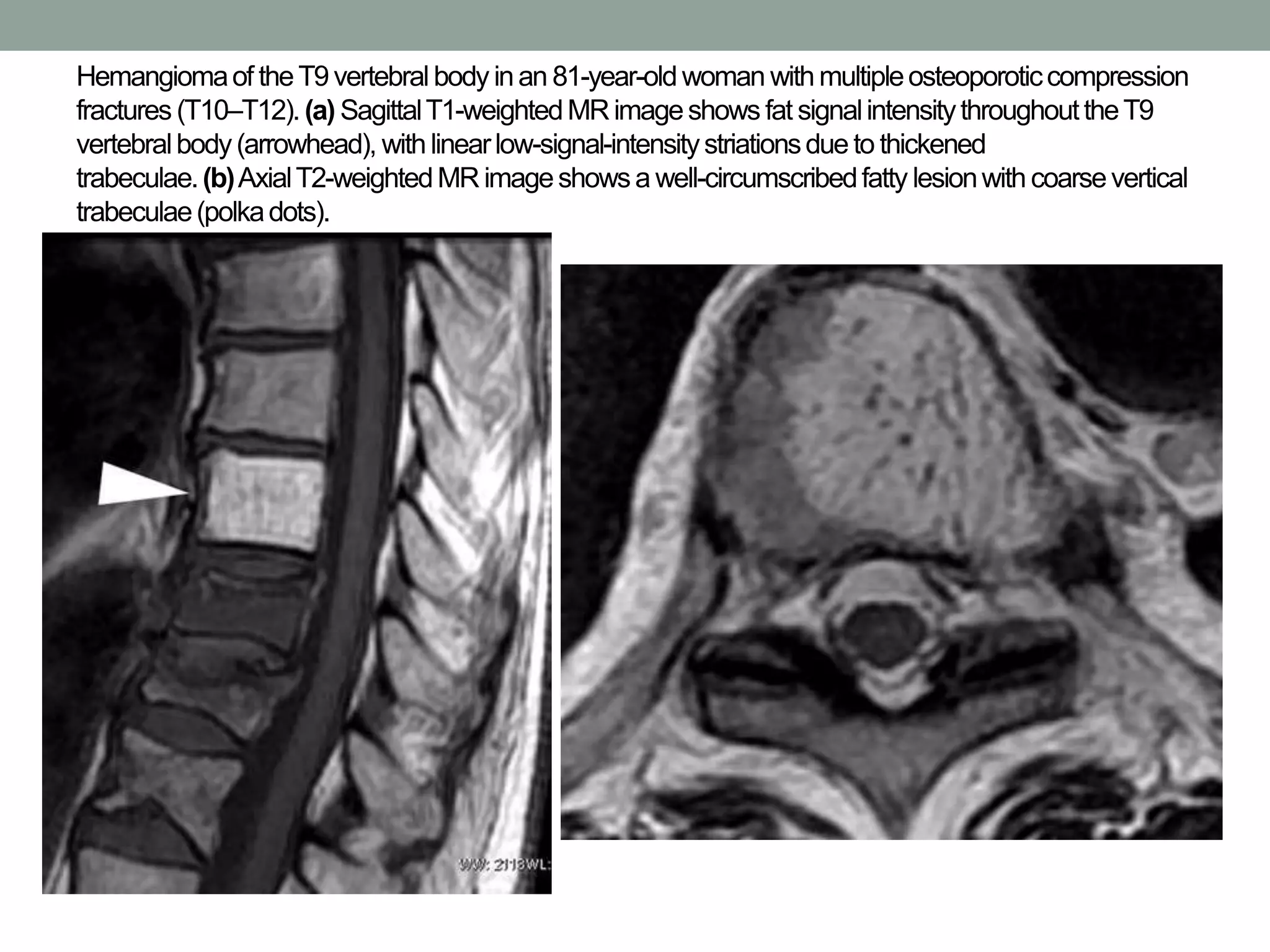
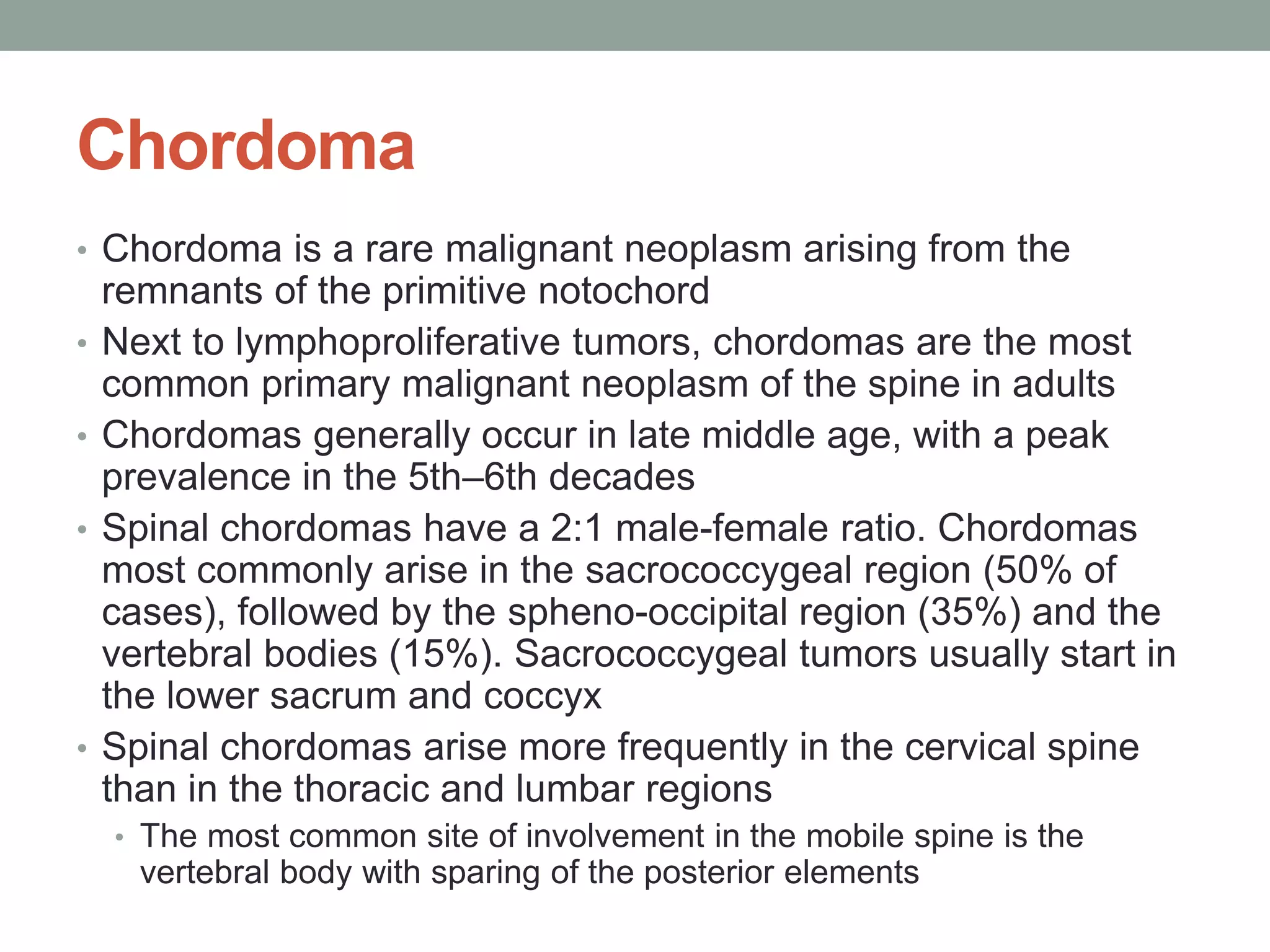
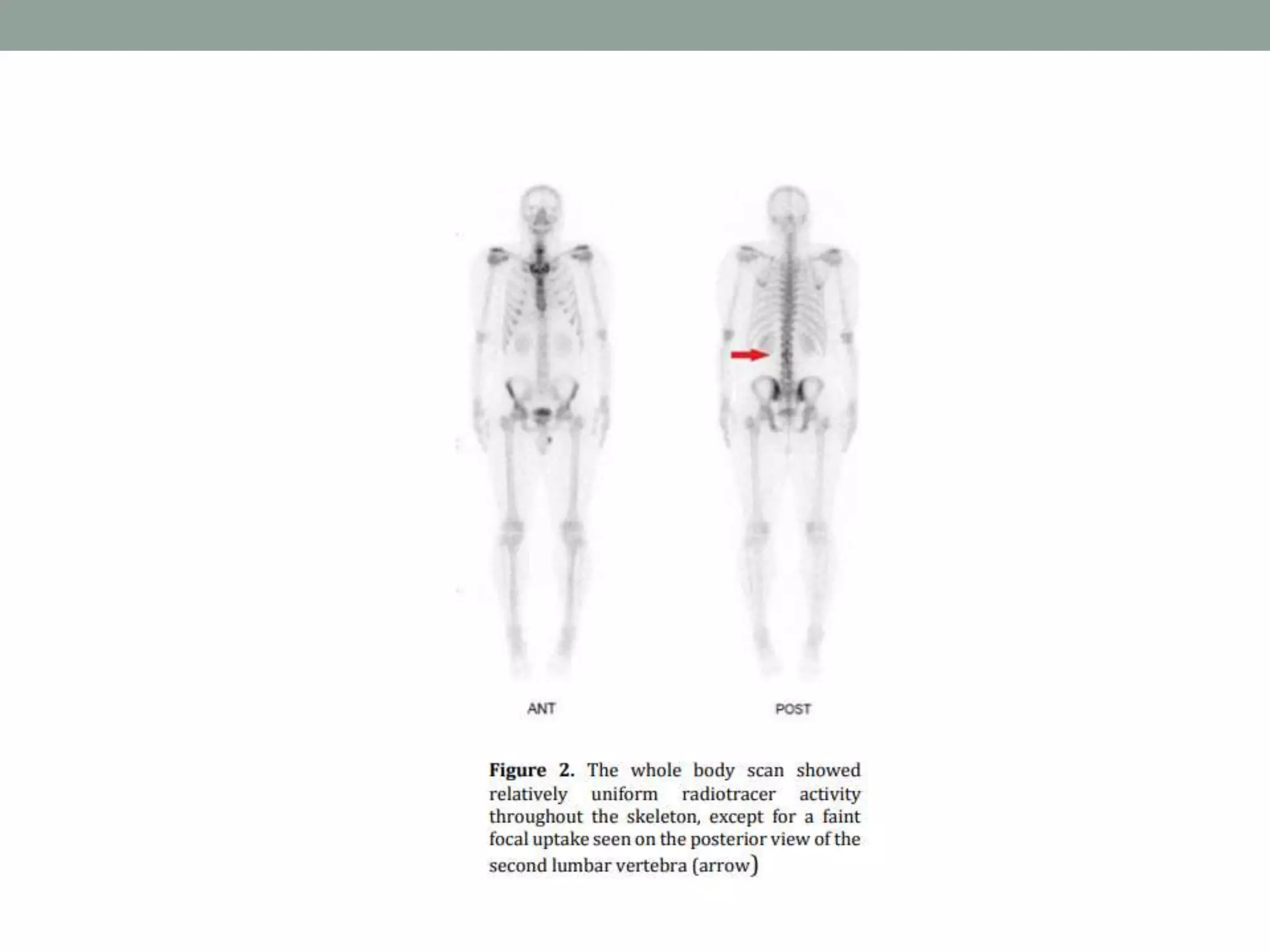
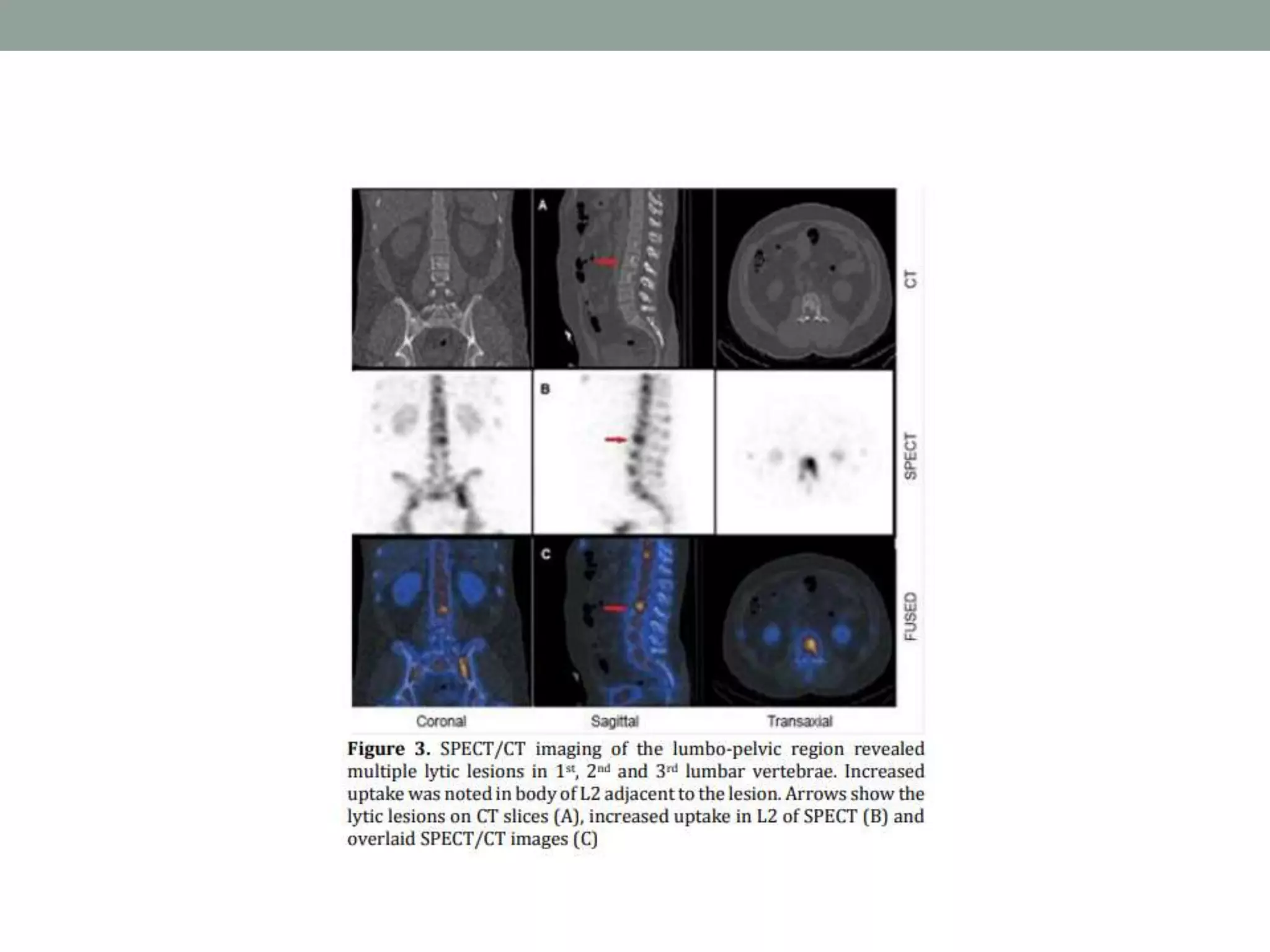
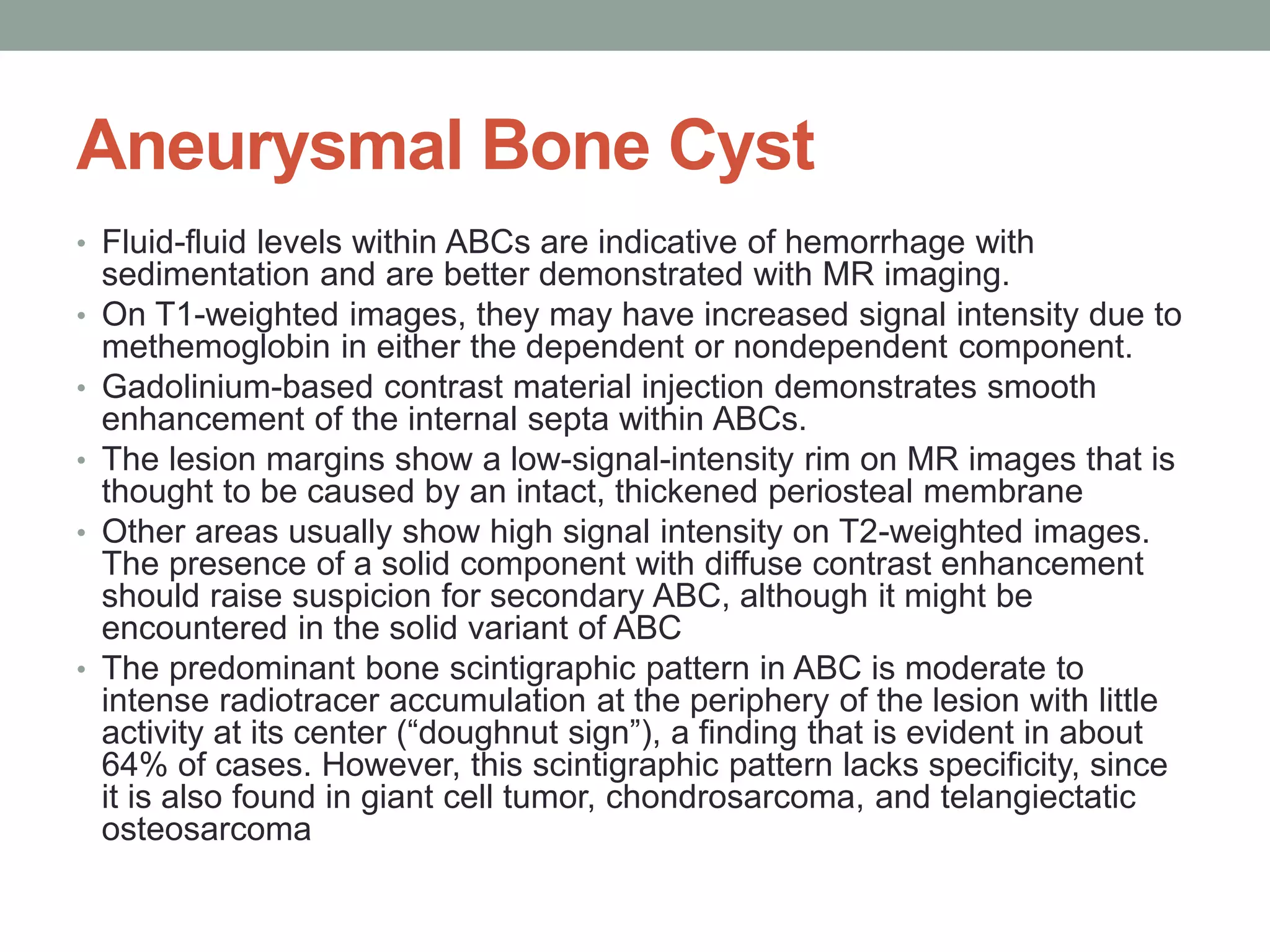
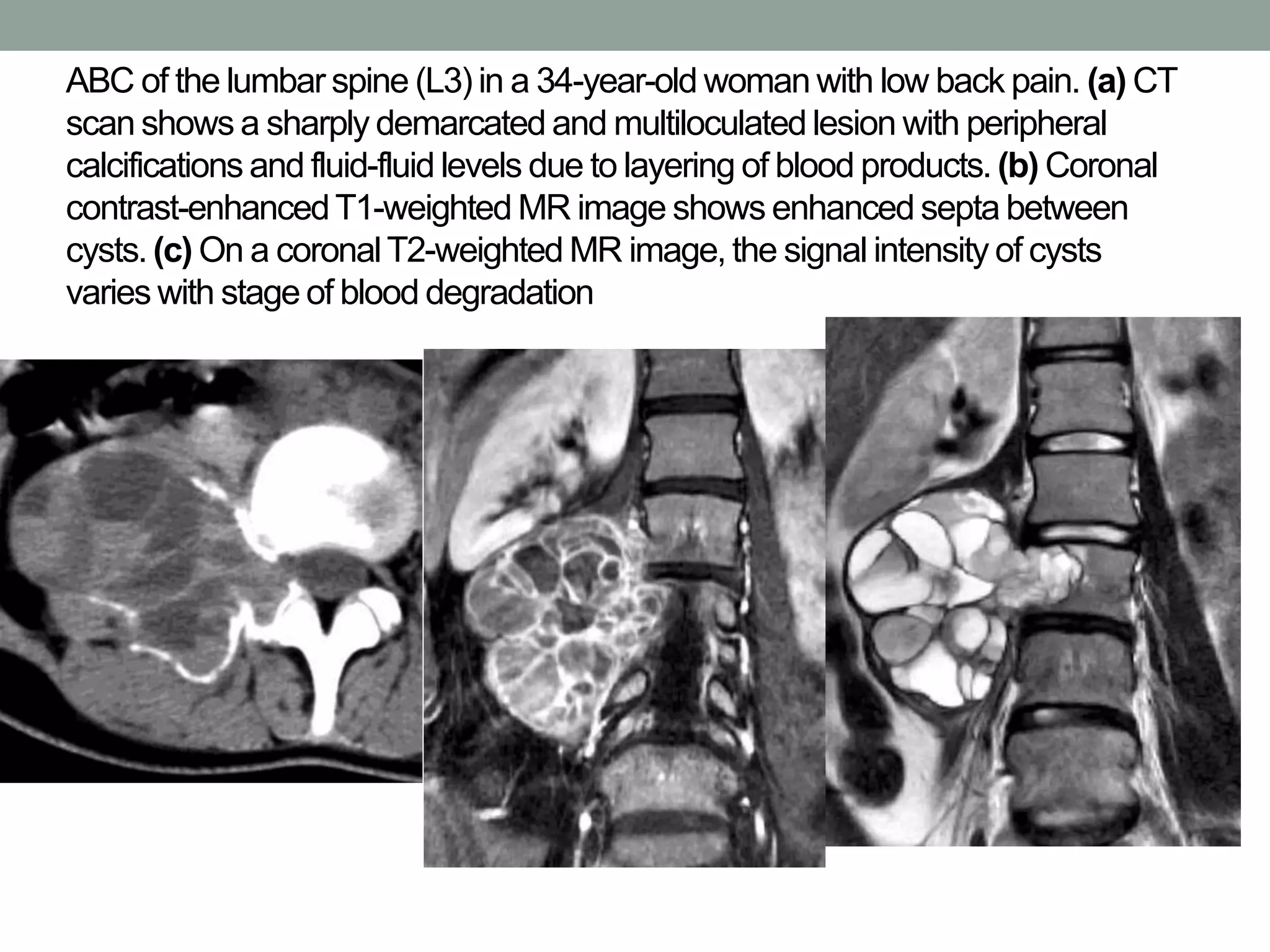
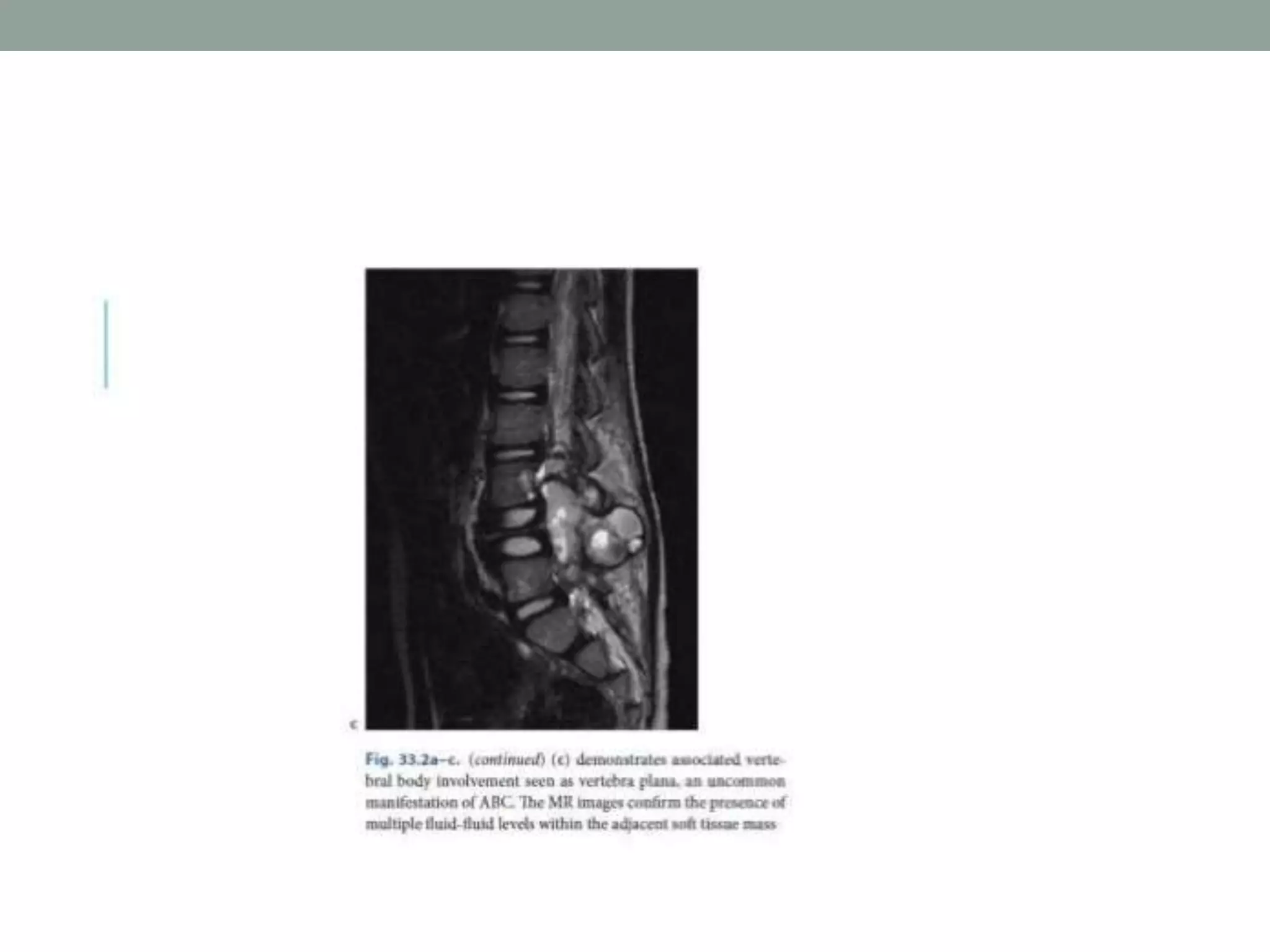
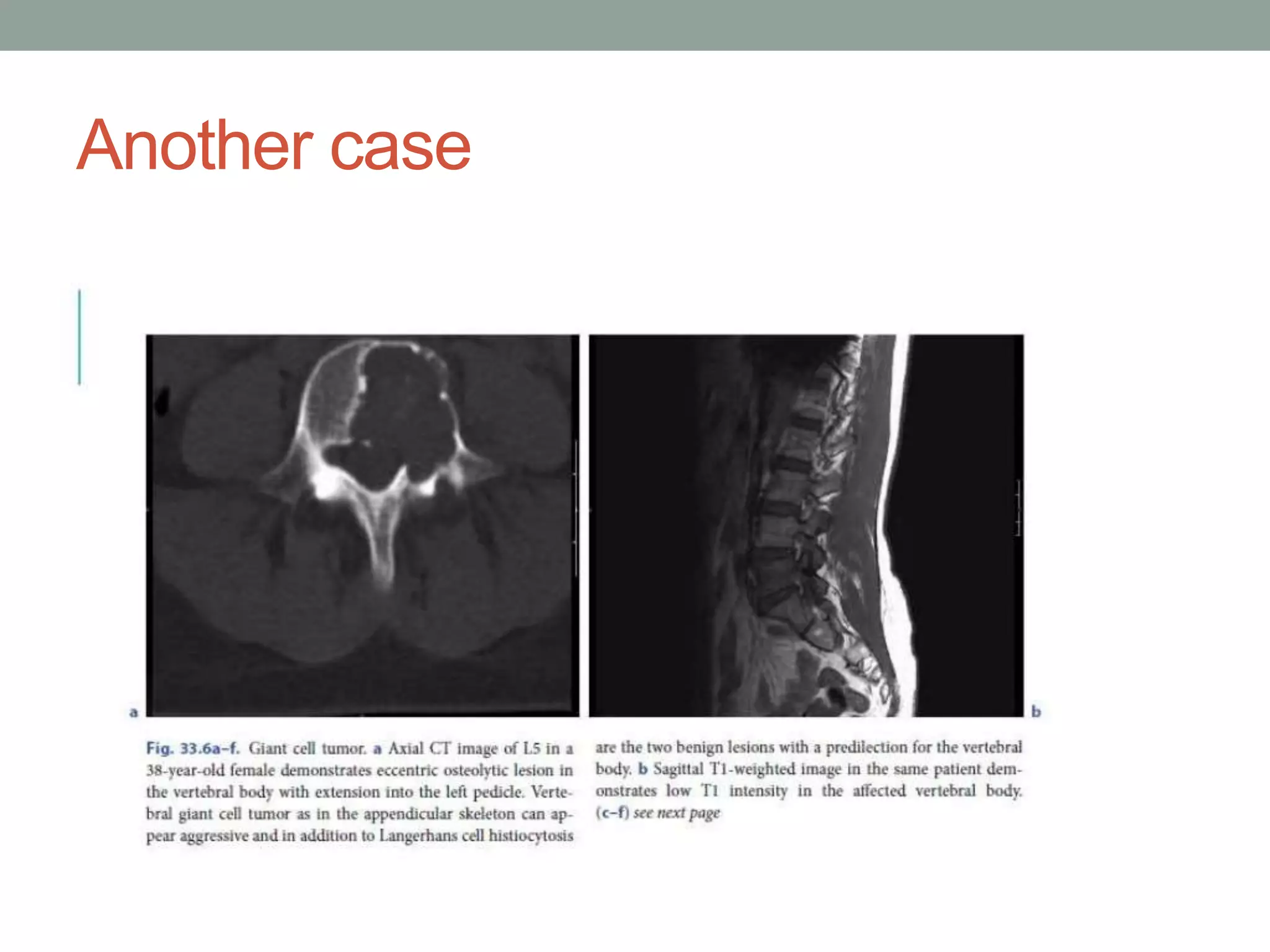
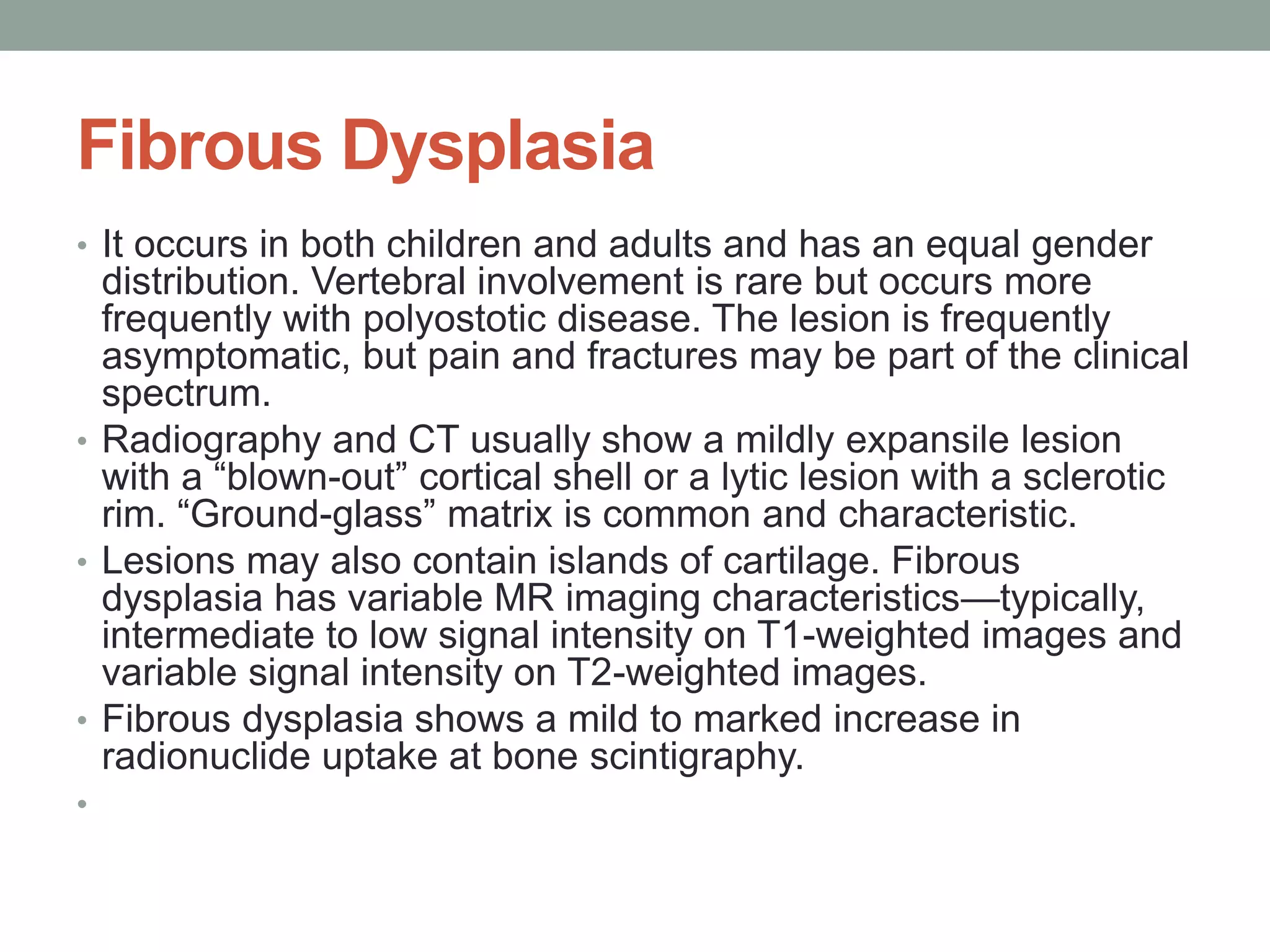
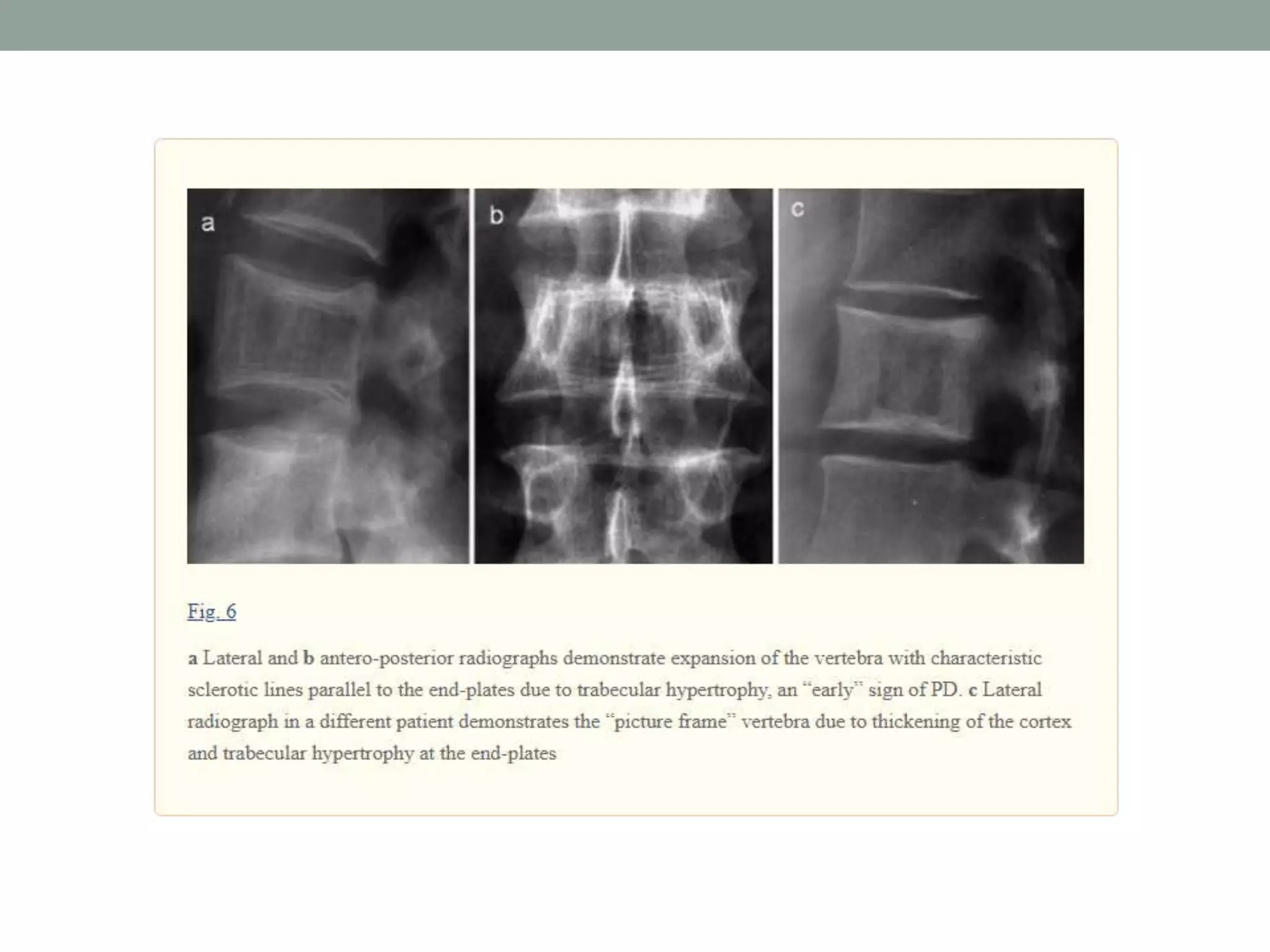
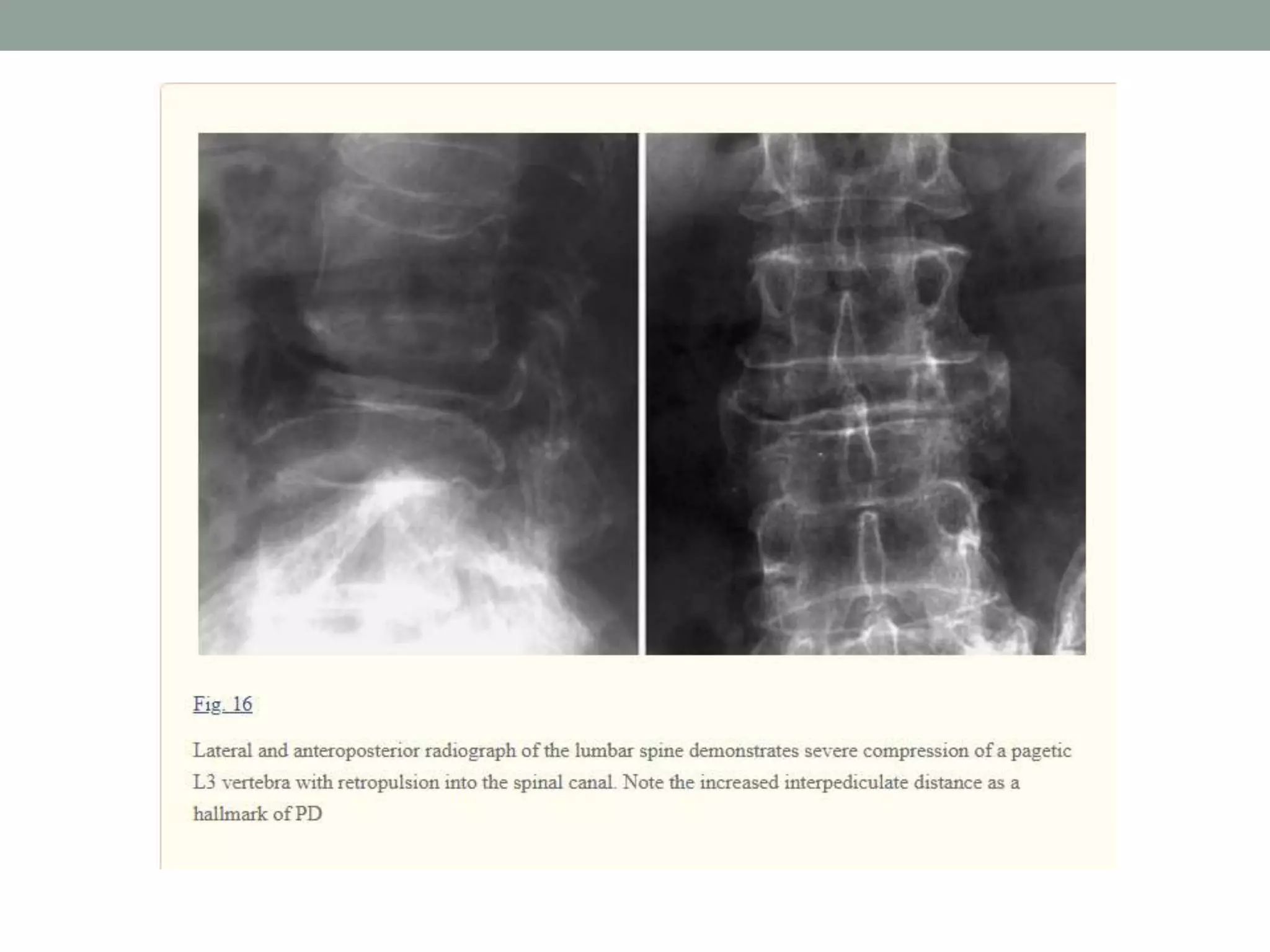
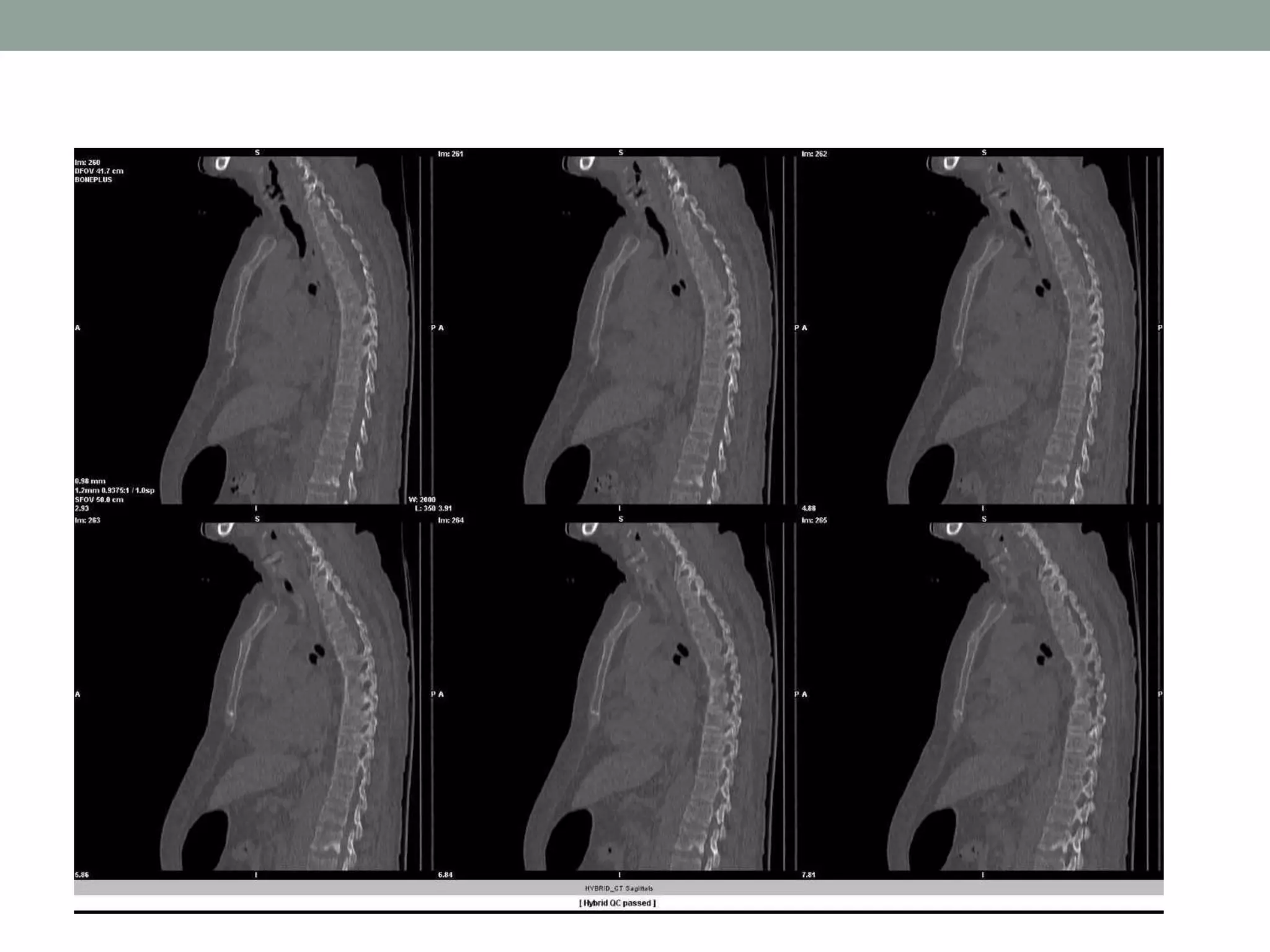
This document discusses primary bone tumors of the spine, detailing their characteristics based on patient age, tumor type, and imaging findings. It highlights benign tumors prevalent in younger patients while malignant tumors predominate in older individuals, with specific tumors like osteosarcoma and chondrosarcoma being noted for their imaging presentations. The document also emphasizes the importance of imaging techniques, such as CT and MRI, in diagnosing and differentiating these tumors.