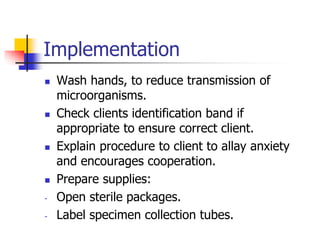
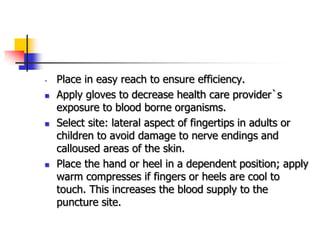
This document provides guidance on collecting various specimen types, including blood, urine, deep specimens, feces, sputum, and genital specimens. It emphasizes the importance of collecting specimens correctly and transporting them to the laboratory promptly to ensure quality results. Key steps include using the proper collection container, obtaining informed consent, maintaining aseptic technique, and documenting and labeling the specimens accurately.