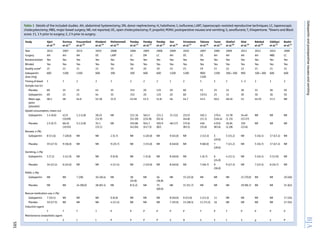
The study analyzes the effectiveness of preoperative gabapentin in preventing postoperative nausea and vomiting (PONV) in abdominal surgeries, finding supportive evidence for its use, with a pooled relative risk reduction for nausea and vomiting. The analysis involved 17 randomized controlled trials, demonstrating a significant decrease in PONV, particularly when propofol was not used in anaesthesia. Future research is suggested to compare gabapentin's efficacy against traditional anti-emetic therapies like 5-HT3 antagonists.



![gabapentinonthefourmainparameters,i.e.nausea,vomiting,
PONVand rescue anti-emetic use, was influenced by individual
studies. The pooled RR for PONV was not significant [0.71 (95%
CI 0.39–1.28)], butwhen thestudybyPandeyand colleagues21
was excluded, the RR was significant [0.59 (95% CI 0.5–0.7)]
and the I2
value for heterogeneity decreased from 94 to
27.2% (Supplementary Table 2). The Galbraith plot showed
no evidence of publication bias (Supplementary Figure 8). The
Egger’s test for asymmetry of the funnel plot was non-
significant (P¼0.27). The trim and fill method estimated the
number of missing studies in the funnel plot as one.
Discussion
The quantitative analysis of the collected data showed
that preoperative administration of gabapentin in patients
undergoing abdominal surgery was associated with a lower in-
cidence of nausea and vomiting. We observed a reduction of
24% for nausea, 38% for vomiting, no significant reduction in
the composite PONV (possibly biased by a single study), and
a 40% reduction in the rescue anti-emetic use in patients
who received preoperative gabapentin. An earlier analysis by
Alayed and colleagues15
also showed that there was a reduc-
tion in the incidence of postoperative nausea and vomiting.
However, the analysis was focussed on only abdominal hyster-
ectomy patients (11 studies). Also, we consider thatcombining
the composite PONV data in the analysis of both nausea
and vomiting outcomes as performed in that analysis could
possibly result in biased estimates. In the present analysis
we included studies on all abdominal surgeries16 – 32
that
evaluated only preoperative gabapentin (even postoperative
gabapentin use was included in the earlier analysis). We
Pooled Relative Risk for Nausea
Favors Gabapentin Favors Placebo
PlaceboGabapentin
Studies Events EventsSample SampleGabapentin Weights RR
(n) (N) Dose (mg) (n) (N) (95% Cl)
Mohamaddi et al
Behdad et al
Ajori et al
Pandey et al*
Ghafari et al
Siddiqui et al
Takmaz et al
Durmus et al
Sen et al
Takmaz et al
Turan et al
RE Model
2
5
8
4
5
17
7
7
9
2
5
0.01
9
5
19
3
7
17
9
9
8
9
0.22 (0.05, 0.96)
0.97 (0.31, 3.01)
0.42 (0.20, 0.90)
1.33 (0.34, 5.21)
0.71 (0.25, 2.02)
1.00 (0.61, 1.63)
0.78 (0.39, 1.54)
0.78 (0.34, 1.76)
1.12 (0.55, 2.32)
0.22 (0.06, 0.86)
7
35
30
69
20
33
36
15
25
20
15
25 0.71 (0.26, 1.95)
3.19%
5.22%
11.28%
3.64%
6.14%
24.61%
13.68%
9.74%
12.24%
3.69%
6.58%
0.76 (0.58, 0.98)100.00%
35
31
69
20
33
36
15
25
20
15
25
300
400
600
600
600
600
900
1200
1200
1200
1200
0.10 0.50 4.00
Relative risk (RR)
Fig 2 Pooled analysis of postoperative nausea.
BJA Achuthan et al.
592](https://image.slidesharecdn.com/bja20151144-150407044806-conversion-gate01/85/Bja-2015-114-4-5-320.jpg)


![moderator analysis. This shows that mechanisms other than the
decreased consumption of opioids are possibly responsible for
gabapentin’s anti-emetic property.
In the sensitivity analysis, the study by Pandey and collea-
gues21
had a significant impact on the results of the PONVend-
point. The pooled RR estimates showed that the effect of
gabapentin on the incidence of PONV was not significant [RR
0.71 (95% CI 20.39–1.28)]. Exclusion of this study resulted in
a statistically significant finding [RR 0.59 (95% CI 20.5–0.7)].
This study by Pandey and colleagues21
showed that preope-
rative gabapentin (300 mg) use caused an increased incidence
of PONV (38/153 compared with 8/153 in the placebo group).
However, in a study by the same authors in 2006,23
it was
shown that the preoperative use of gabapentin (600 mg)
indeed had a beneficial effect on the incidence of PONV (46/
125 compared with 75/125 in the placebo group). Both the
studies were done in laparoscopic cholecystectomy patients.
The reasons for this disparity are unknown; we believe
that this difference could be due to the fact that PONV was
not the primary endpoint in the first study, whereas it was
in the second. This could have led to differences in study
conduct and analysis. Similarly, concerns about the reliability
of the data not formally collected as the primary endpoint
were raised in another recent review.45
In the present analysis the observed reduction in post-
operative nausea and vomiting with preoperative gabapentin
support our recommendation of including gabapentin in
the armamentarium of pharmacotherapies for PONV in pati-
ents undergoing abdominal surgery. The current treatment
guidelines recommend 5-HT3, dopaminergic, and histaminic
antagonists as prophylaxis and treatment for PONV.34
Based
on the additional analgesic properties, safety profile, and
cost, gabapentin might be usefully included in the current list
of PONV prophylactic agents.
Pooled Relative Risk for Rescue Antiemetic Use
Favors Gabapentin Favors Placebo
PlaceboGabapentin
Studies Events EventsSample SampleGabapentin Weights RR
(n) (N) Dose (mg) (n) (N) (95% Cl)
Mohamaddi et al
Ajori et al
Shrivastava et al
Bashir et al
Takmaz et al
Sen et al
Takmaz et al
Turan et al
RE Model
0
7
9
17
12
8
2
11
0.01
4
19
23
27
11
7
11
16
0.11 (0.01, 1.99)
0.37 (0.17, 0.82)
0.39 (0.20, 0.77)
0.63 (0.40, 1.00)
1.09 (0.73, 1.62)
1.14 (0.51, 2.55)
0.18 (0.05, 0.68)
0.69 (0.40, 1.17)
35
69
60
50
15
20
15
25
1.69%
11.97%
13.89%
18.07%
19.40%
11.92%
6.34%
16.72%
0.60 (0.41, 0.89)100.00%
35
69
60
50
15
20
15
25
300
600
600
600
900
1200
1200
1200
0.10 0.50 4.00
Relative risk (RR)
Fig 5 Pooled analysis of postoperative use of rescue medication.
Gabapentin and postoperative nausea and vomiting BJA
595](https://image.slidesharecdn.com/bja20151144-150407044806-conversion-gate01/85/Bja-2015-114-4-8-320.jpg)
![Conclusion
The present analysis overcomes the limitations of earlier ana-
lyses and the additional moderator and sensitivity analyses
conducted provide strong evidence favouring preoperative
gabapentin as a pharmacotherapy for prevention of PONV in
patients undergoing abdominal surgeries. The use of propofol
in the perioperative period could possibly be an important
factor influencing the decision to use gabapentin as a prevent-
iveagent.Nevertheless,theanalgesicpropertiesandapossible
longer duration of action favour preoperative gabapentin
use irrespective of the anaesthetic agent. Future studies com-
paring the efficacy of gabapentin with the more commonly
used 5HT3 antagonists are needed to precisely define the
role of preoperative gabapentin in PONV.
Supplementary material
Supplementary material is available at British Journal of
Anaesthesia online.
Authors’ contributions
S.A., I.S., and S.B. were involved in the data extraction. S.A., I.S.,
A.S., D.H., and A.C. were involved in the data analysis and the
drafting and editing of the manuscript. D.H. and A.C. reviewed
and approved the final manuscript.
Declaration of interest
None declared.
References
1 Wagner DS, Yap JM, Bradley KM, Voepel-Lewis T. Assessing parents
preferences for the avoidance of undesirable anesthesia side
effects in their children undergoing surgical procedures. Paediatr
Anaesth 2007; 17: 1035–42
2 Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia
outcomes are important to avoid? The perspective of patients.
Anesth Analg 1999; 89: 652–8
3 Kerger H, Turan A, Kredel M, et al. Patients’ willingness to pay for
anti-emetic treatment. Acta Anaesthesiol Scand 2007; 51: 38–43
4 Habib AS, Chen YT, Taguchi A, Hu XH, Gan TJ. Postoperative nausea
and vomiting following inpatient surgeries in a teaching hospital: a
retrospective database analysis. Curr Med Res Opin 2006; 22:
1093–9
5 Hill RP, Lubarsky DA, Phillips-Bute B, et al. Cost-effectiveness of
prophylactic antiemetic therapy with ondansetron, droperidol, or
placebo. Anesthesiology 2000; 92: 958–67
6 Carroll NV, Miederhoff PA, Cox FM, Hirsch JD. Costs incurred by out-
patient surgical centers in managing postoperative nausea and
vomiting. J Clin Anesth 1994; 6: 364–9
7 Franck M, Radtke FM, Apfel CC, et al. Documentation of post-
operative nausea and vomiting in routine clinical practice. J Int
Med Res 2010; 38: 1034–41
8 Apfel CC, Laara E, Koivuranta M, Greim CA, Roewer N. A simplified
risk score for predicting postoperative nausea and vomiting: con-
clusions from cross-validations between two centers. Anesthesi-
ology 1999; 91: 693–700
9 Chang CY, Challa CK, Shah J, Eloy JD. Gabapentin in acute post-
operative pain management. Biomed Res Int 2014; 2014: 631756
10 Bockbrader HN, Wesche D, Miller R, Chapel S, Janiczek N, Burger P. A
comparison of the pharmacokinetics and pharmacodynamics of
pregabalin and gabapentin. Clin Pharmacokinet 2010; 49: 661–9
11 VanMeter SA, Kavanagh ST, Warren S, Barrett RW. Dose response of
gabapentinenacarbilversusplaceboinsubjects withmoderate-to-
severe primary restless legs syndrome: an integrated analysis of
three 12-week studies. CNS Drugs 2012; 26: 773–80
12 Guttuso T Jr, Roscoe J, Griggs J. Effect of gabapentin on nausea
induced by chemotherapy in patients with breast cancer. Lancet
2003; 361: 1703–5
13 Downs SH, Black N. The feasibility of creating a checklist for the as-
sessment of the methodological quality both of randomised and
non-randomised studies of health care interventions. J Epidemiol
Community Health 1998; 52: 377–84
14 Wolfgang V. Conducting meta-analyses in R with the metafor
package. J Stat Software 2010; 36: 1–48
15 Alayed N, Alghanaim N, Tan X, Tulandi T. Preemptive use of gaba-
pentin in abdominal hysterectomy: a systematic review and
meta-analysis. Obstet Gynecol 2014; 123: 1221–9
16 Ajori L, Nazari L, Mazloomfard MM, Amiri Z. Effects of gabapentin on
postoperative pain, nausea and vomiting after abdominal hyster-
ectomy: a double blind randomized clinical trial. Arch Gynecol
Obstet 2012; 285: 677–82
17 Durmus M, Kadir But A, Saricicek V, Ilksen Toprak H, Ozcan Ersoy M.
The post-operative analgesic effects of a combination of gabapen-
tin and paracetamol in patients undergoing abdominal hysterec-
tomy: a randomized clinical trial. Acta Anaesthesiol Scand 2007;
51: 299–304
18 Frouzanfard F, Fazel MR, Abolhasani A, Fakharian E, Mousavi G,
Moravveji A. Effects of gabapentin on pain and opioid consumption
after abdominal hysterectomy. Pain Res Manag 2013; 18: 94–6
19 KhademiS,GhaffarpasandF,HeiranHR,AsefiA.Effectsofpreopera-
tive gabapentin on postoperative nausea and vomiting after open
cholecystectomy: a prospective randomized double-blind placebo-
controlled study. Med Princ Pract 2010; 19: 57–60
20 Mohammadi SS, Seyedi M. Effects of gabapentin on early post-
operative pain, nausea and vomiting in laparoscopic surgery for
assistedreproductivetechnologies.PakJBiolSci2008;11:1878–80
21 Pandey CK, Priye S, Singh S, Singh U, Singh RB, Singh PK. Preemptive
use of gabapentin significantly decreases postoperative pain and
rescue analgesic requirements in laparoscopic cholecystectomy.
Can J Anaesth 2004; 51: 358–63
22 Pandey CK, Singhal V, Kumar M, et al. Gabapentin provides effective
postoperative analgesia whether administered pre-emptively or
post-incision. Can J Anaesth 2005; 52: 827–31
23 Pandey CK, Priye S, Ambesh SP, Singh S, Singh U, Singh PK. Prophy-
lactic gabapentin for prevention of postoperative nausea and
vomiting in patients undergoing laparoscopic cholecystectomy: a
randomized, double-blind, placebo-controlled study. J Postgrad
Med 2006; 52: 97–100
24 Sen H, Sizlan A, Yanarates O, et al. A comparison of gabapentin and
ketamine in acute and chronic pain after hysterectomy. Anesth
Analg 2009; 109: 1645–50
25 Srivastava U, Kumar A, Saxena S, Mishra AR, Saraswat N, Mishra S.
Effect of preoperative gabapentin on postoperative pain and tra-
madol consumption after minilap open cholecystectomy: a rando-
mized double-blind, placebo-controlled trial. Eur J Anaesthesiol
2010; 27: 331–5
26 Takmaz SA, Kaymak C, Pehlivan BS, Dikmen B. [Effect of preo-
perative 900 and 1200 mg single oral dose of gabapentin on post-
operative pain relief and tramadol consumption in open
cholecystectomy surgery]. Agri 2007; 19: 32–8
BJA Achuthan et al.
596](https://image.slidesharecdn.com/bja20151144-150407044806-conversion-gate01/85/Bja-2015-114-4-9-320.jpg)
![27 Turan A, Karamanlioglu B, Memis D, Usar P, Pamukcu Z, Ture M. The
analgesic effects of gabapentin after total abdominal hysterec-
tomy. Anesth Analg 2004; 98: 1370–3
28 GhafariMH,AkramiM,NouralishahiB,SadeghA.Preoperativegaba-
pentin or clonidine decreases postoperative pain and morphine
consumption after abdominal hysterectomy. Res J Biol Sci 2009;
4: 458–63
29 Ghai A, Gupta M, Hooda S, Singla D, Wadhera R. A randomized con-
trolledtrialtocomparepregabalinwithgabapentinforpostoperative
pain in abdominal hysterectomy. Saudi J Anaesth 2011; 5: 252–7
30 Behdad S, Ayatollahi V, Bafghi AT, Tezerjani MD, Abrishamkar M.
Effect of gabapentin on postoperative pain and operation compli-
cations: a randomized placebo controlled trial. West Indian Med J
2012; 61: 128–33
31 Siddiqui NT, Fischer H, Guerina L, Friedman Z. Effect of a pre-
operative gabapentin on postoperative analgesia in patients with
inflammatory bowel disease following major bowel surgery: a
randomized, placebo-controlled trial. Pain Pract 2014; 14: 132–9
32 Bashir F, Mohd K, Qazi S, Hashia AM. A randomized, double blind,
placebo controlled study evaluating preventive role of gabapentin
for PONV in patients undergoing laparoscopic cholecystectomy.
JK Sci J Med Educ Res 2009; 11: 190–3
33 Apfel CC, HeidrichFM, Jukar-Rao S, et al. Evidence-based analysis of
risk factors for postoperative nausea and vomiting. Br J Anaesth
2012; 109: 742–53
34 Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the
management of postoperative nausea and vomiting. Anesth
Analg 2014; 118: 85–113
35 Tramer M, Moore A, McQuay H. Propofol anaesthesia and post-
operative nausea and vomiting: quantitative systematic review of
randomized controlled studies. Br J Anaesth 1997; 78: 247–55
36 Sen H, Sizlan A, Yanarates O, et al. The effects of gabapentin on
acute and chronic pain after inguinal herniorrhaphy. Eur J Anaes-
thesiol 2009; 26: 772–6
37 Guttuso T Jr, Kurlan R, McDermott MP, Kieburtz K. Gabapentin’s
effects on hot flashes in postmenopausal women: a randomized
controlled trial. Obstet Gynecol 2003; 101: 337–45
38 Maneuf YP, Hughes J, McKnight AT. Gabapentin inhibits the sub-
stance P-facilitated K+
-evoked release of [3
H]glutamate from rat
caudial trigeminal nucleus slices. Pain 2001; 93: 191–6
39 Fehrenbacher JC, Taylor CP, Vasko MR. Pregabalin and gabapentin
reduce release of substance P and CGRP from rat spinal tissues
only after inflammation or activation of protein kinase C. Pain
2003; 105: 133–41
40 Felix R, Gurnett CA, De Waard M, Campbell KP. Dissection of func-
tional domains of the voltage-dependent Ca2+
channel a2d
subunit. J Neurosci 1997; 17: 6884–91
41 Stahl SM. Mechanism of action of alpha2delta ligands: voltage sen-
sitive calcium channel (VSCC) modulators. J Clin Psychiatry 2004;
65: 1033–4
42 Dias JM, de Brito TV, de Aguiar Magalhaes D, et al. Gabapentin, a
synthetic analogue of gamma aminobutyric acid, reverses system-
ic acute inflammation and oxidative stress in mice. Inflammation
2014; 37: 1826–36
43 Rychter J, Clave P. Intestinal inflammation in postoperative ileus:
pathogenesis and therapeutic targets. Gut 2013; 62: 1534–5
44 Clarke H, KirkhamKR, OrserBA, et al. Gabapentin reduces preopera-
tive anxiety and pain catastrophizing in highly anxious patients
prior to major surgery: a blinded randomized placebo-controlled
trial. Can J Anaesth 2013; 60: 432–43
45 Guttuso T Jr. Gabapentin’s anti-nausea and anti-emetic effects: a
review. Exp Brain Res 2014; 232: 2535–9
Handling editor: J. G. Hardman
Gabapentin and postoperative nausea and vomiting BJA
597](https://image.slidesharecdn.com/bja20151144-150407044806-conversion-gate01/85/Bja-2015-114-4-10-320.jpg)
