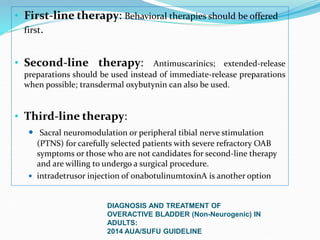
Pelvic floor muscle training (PFMT) and behavioral therapies are recommended as first-line treatments for overactive bladder (OAB) according to international guidelines. PFMT involves exercises to strengthen pelvic floor muscles and can be used alone or combined with other treatments like bladder training. Studies show PFMT reduces incontinence episodes and improves quality of life and irritative symptoms. It is considered as effective as medications with fewer side effects. Biofeedback and electrical stimulation may help when patients cannot contract muscles properly. Guidelines indicate behavioral therapies should be tried for 3 months before other options due to their effectiveness and lack of side effects.






















![Systemic Review on the role Behavorial Therapy for OABSystemic Review concluded
Decreas in number of incontinence episodes (decreased from 64% to
86% after treatment versus before treatment)
Improvement in quality of life (P≤0.001)
Decrease in irritative symptoms (P=0.035 to P<0.001)
Nocturia
Activities and participation, maximum flow rate, mean
voided volume and daytime frequency were not
significantly improved in all trials..
[Pelvic floor muscles training, electrical stimulation,
bladder training and lifestyle interventions to manage lower
urinary tract dysfunction in multiple sclerosis: a systematic
2013 Dec 11 review].](https://image.slidesharecdn.com/roleofpmftinoab-200221101555/85/Role-of-pmft-in-oab-24-320.jpg)




![A retrospective comparison of
ring pessary and
multicomponent behavioral
therapy in managing overactive
bladder
Int urogynecol 2014 may
Ring pessary and multicomponent
behavioral therapy had similar cure
rates [19 %] vs [20 %] respectively.](https://image.slidesharecdn.com/roleofpmftinoab-200221101555/85/Role-of-pmft-in-oab-29-320.jpg)














