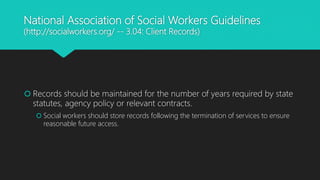
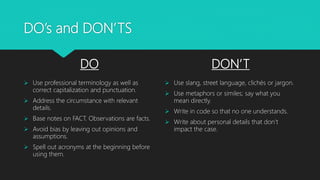
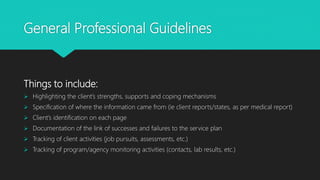
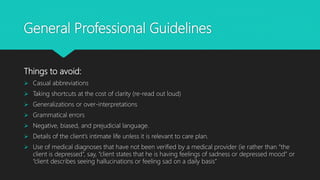
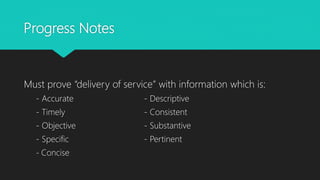
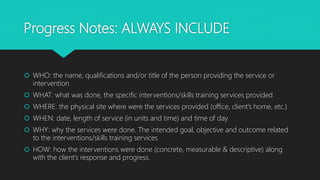
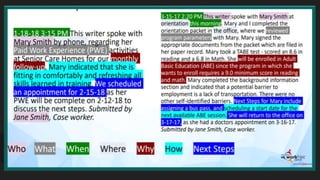
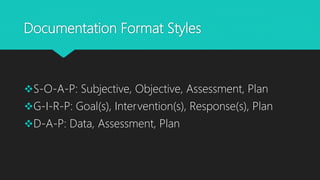
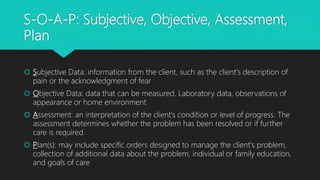
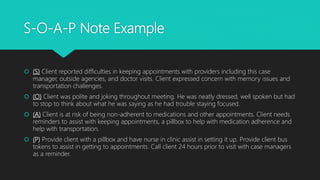
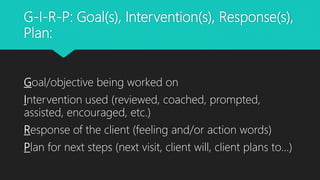
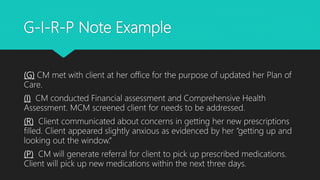
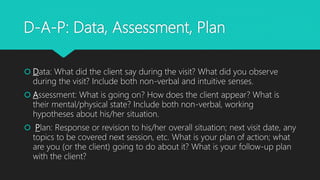
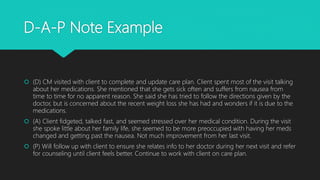
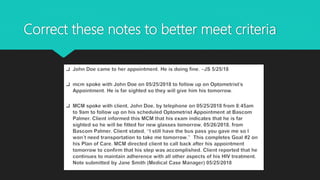
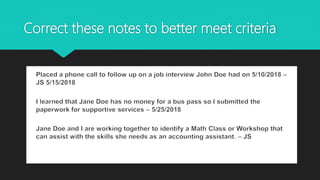
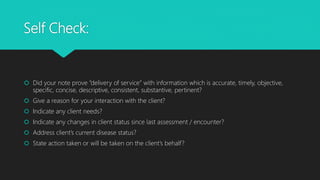
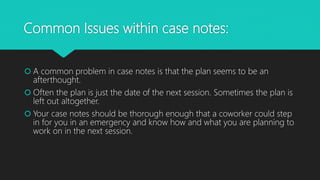
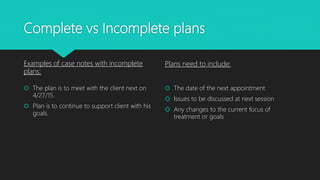
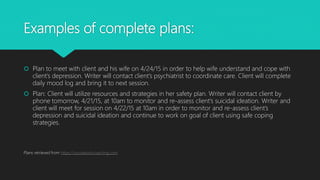
The document provides guidelines for effective social work documentation, emphasizing the importance of accurate records for service planning and evaluation. It outlines best practices for documentation, including maintaining confidentiality, using professional language, and providing specific client information, while also detailing acceptable formats for progress notes. Additionally, it highlights common issues and offers resources for improving case management documentation.