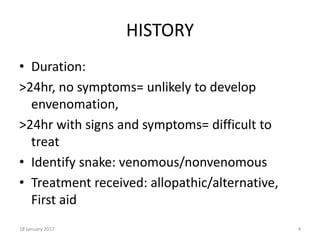
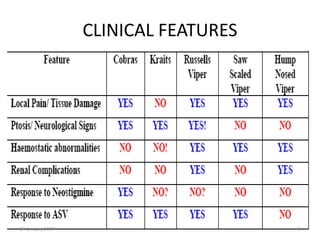
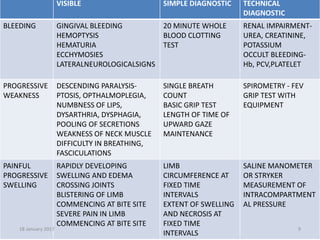
The document provides an overview of snake bite protocols. It discusses the diagnosis and treatment of snake bites, including administering antivenom and neostigmine for neurotoxic symptoms. Diagnosis involves identifying symptoms characteristic of different snake species based on visible signs, simple tests, or more advanced diagnostic techniques. Treatment depends on the severity and symptoms presented, with life-threatening cases involving antivenom administration and supportive care like dialysis or ventilation.