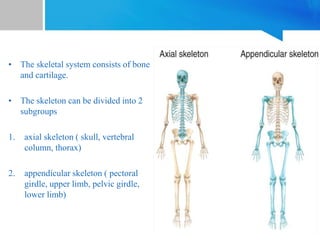
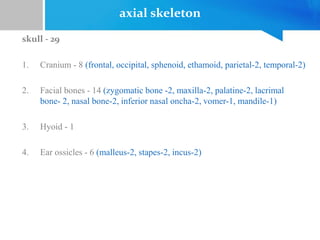
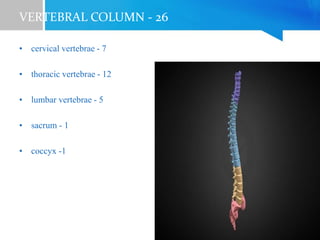
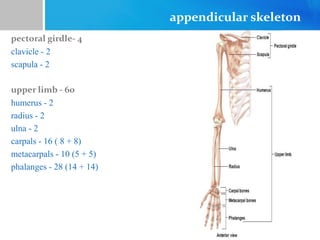
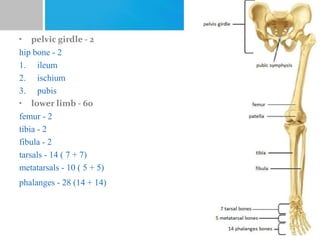
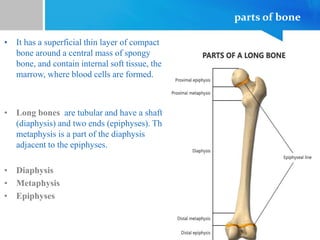
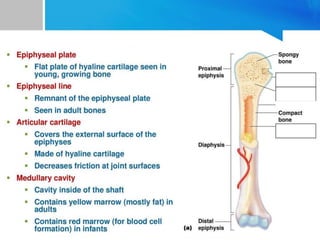
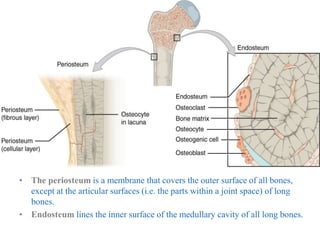
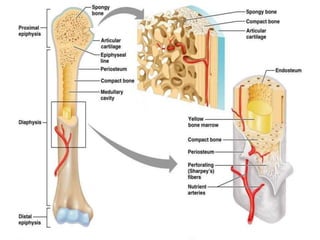
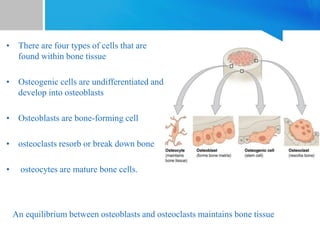
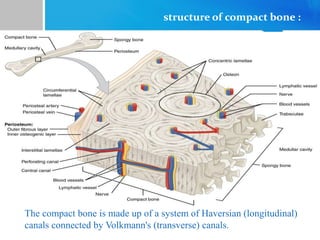
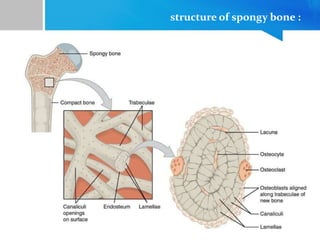
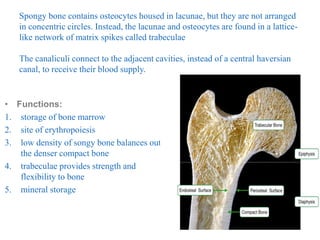
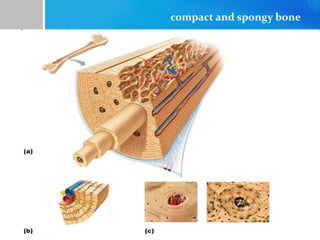
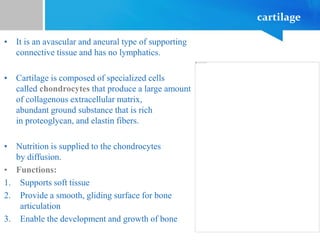
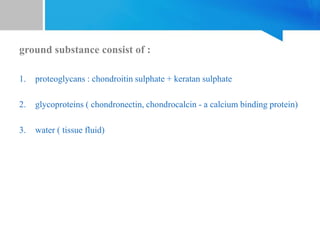
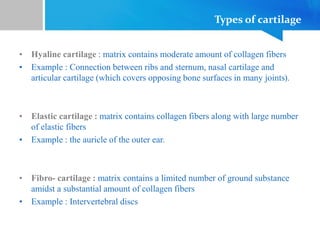
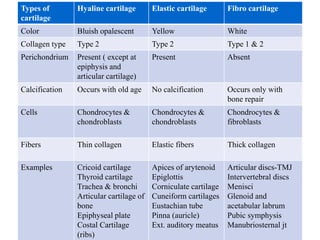
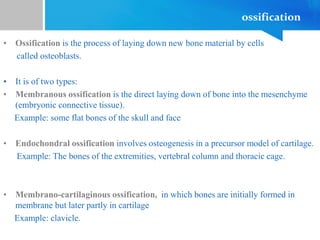
The skeletal system is comprised of bones and cartilage, divided into the axial and appendicular skeleton. Bones function as supportive structures, protect vital organs, and serve as reservoirs for minerals, with various types including compact and spongy bone based on structure. Cartilage supports soft tissue and facilitates bone growth, with types including hyaline, elastic, and fibrocartilage, each serving distinct roles in the body.