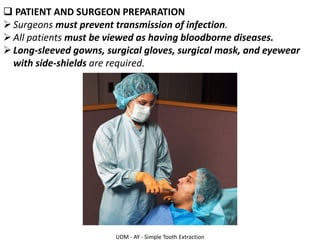
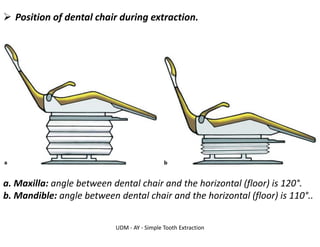
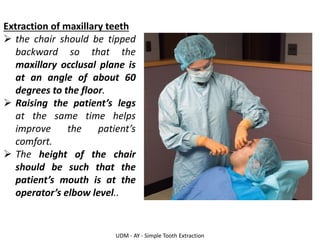
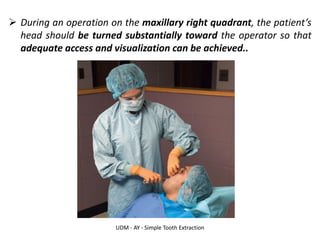
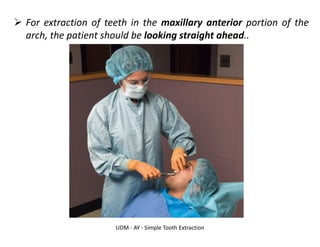
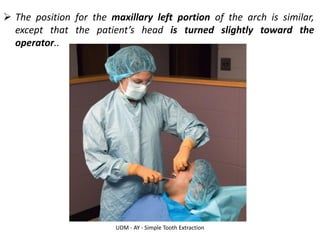
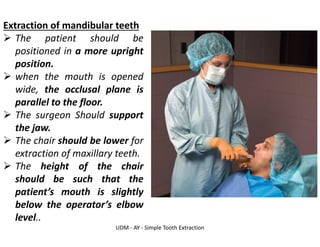
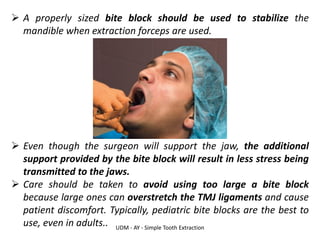
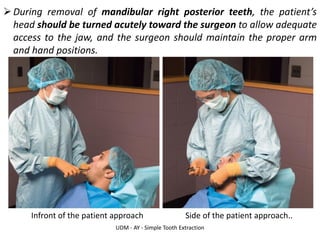
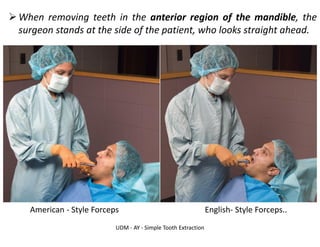
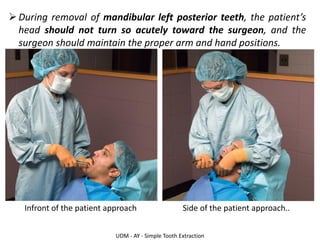
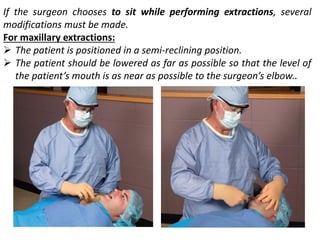
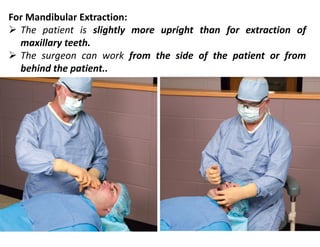
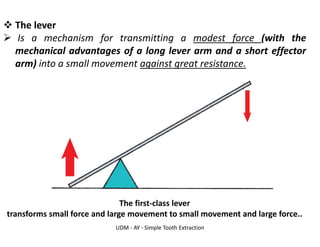
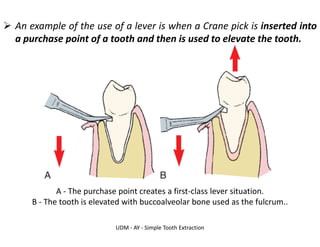
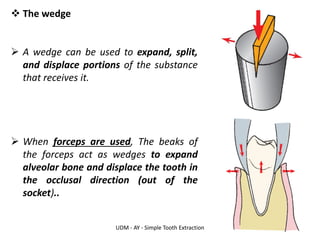
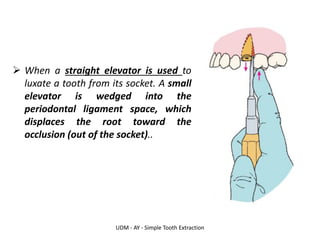
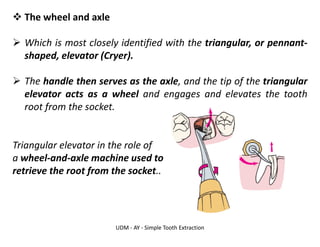
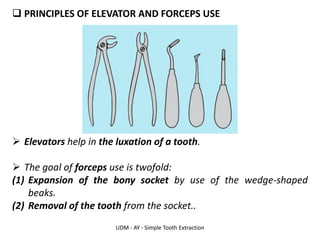
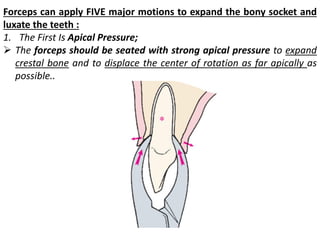
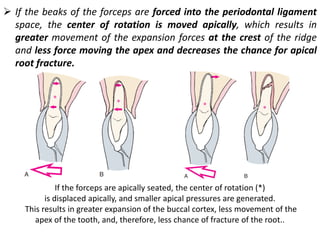
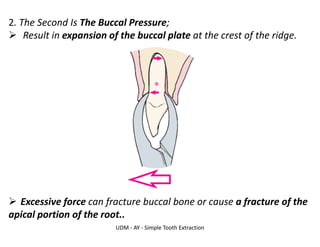
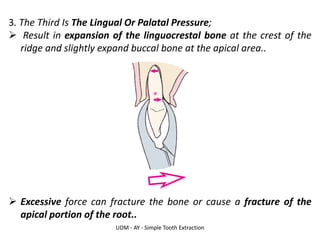
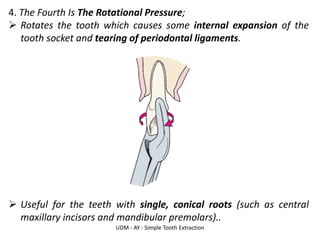
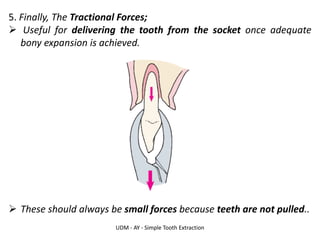
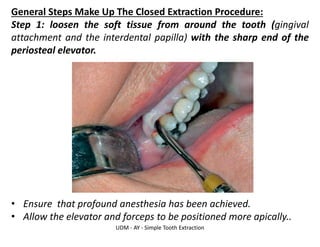
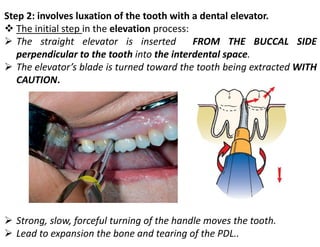
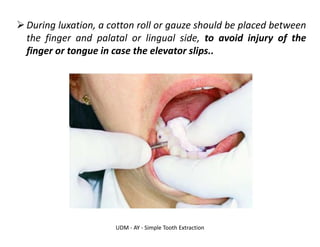
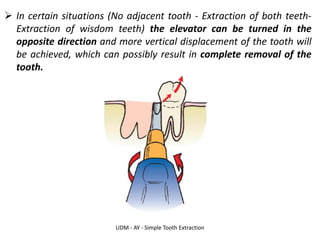
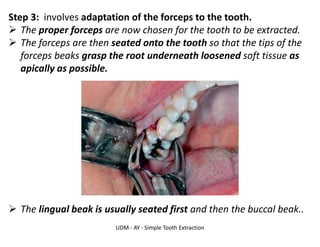
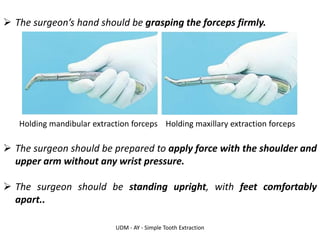
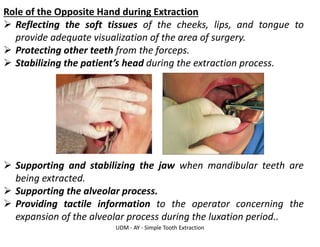
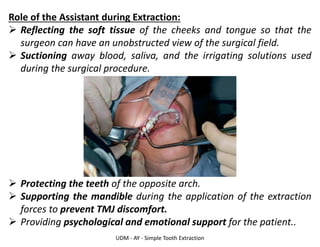
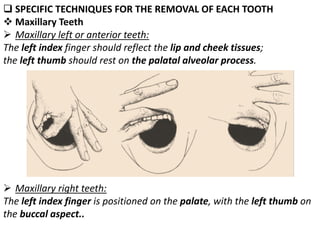
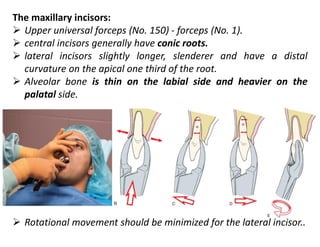
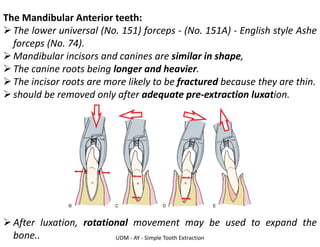
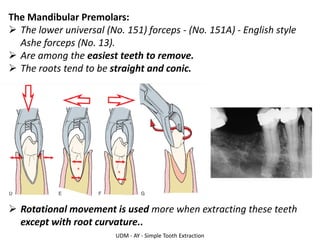
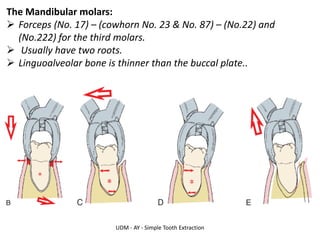
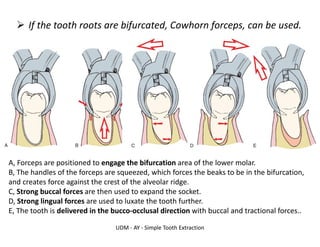
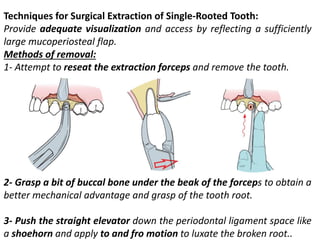
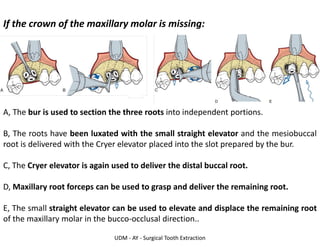
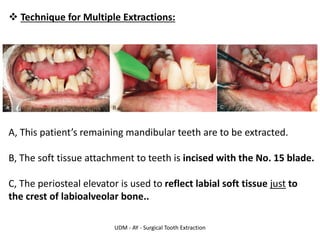
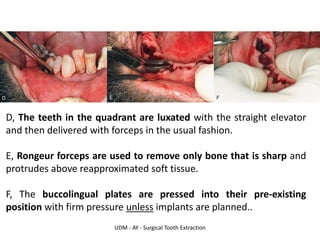
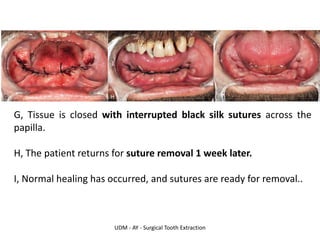
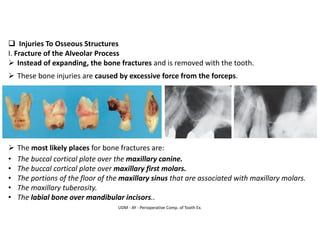
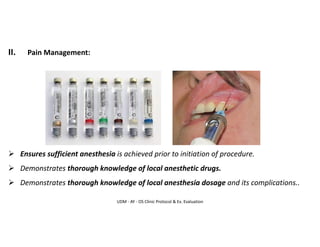
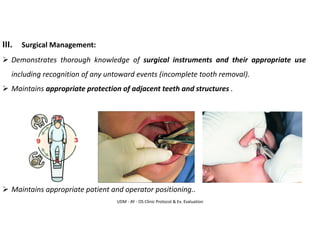
The document outlines the procedure and principles of simple tooth extraction, including patient and surgeon preparation, positioning during the procedure, and the mechanical principles involved. It emphasizes the importance of correct chair positioning for both maxillary and mandibular extractions, the proper use of elevators and forceps, and detailed steps for performing an atraumatic extraction. Specific techniques for removing various types of teeth are also discussed, highlighting the role of the assistant and the importance of minimizing trauma during the extraction process.