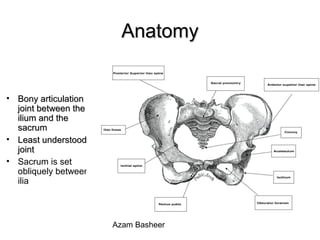
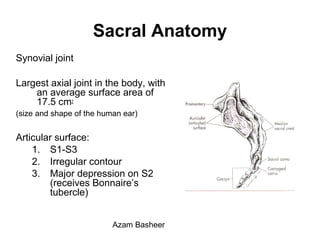
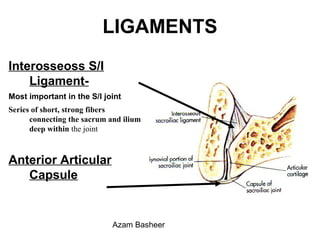
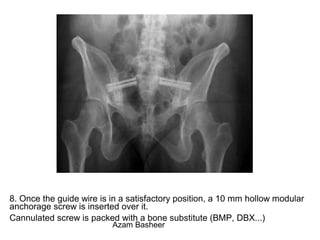
The document discusses the sacroiliac joint (SIJ), including its anatomy, biomechanics, evaluation, and treatment options for SIJ pain. Key points include:
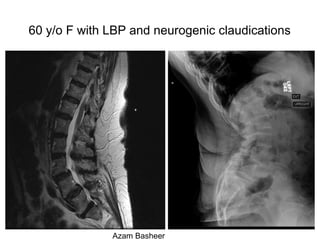
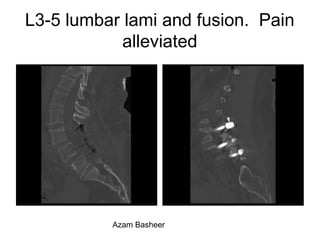
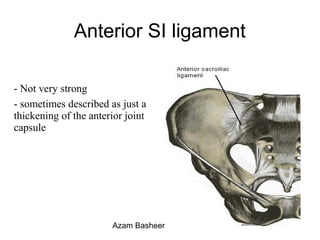
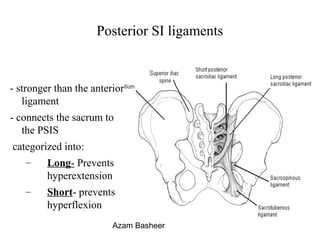
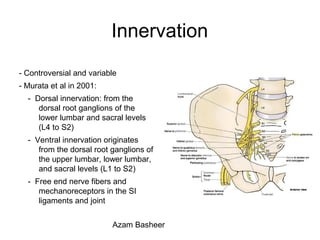
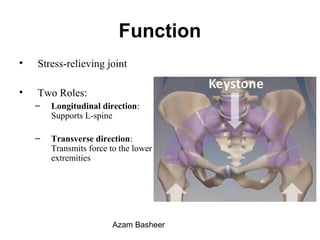
- The SIJ is a synovial joint between the sacrum and ilium bones that allows limited motion. It is innervated by lumbar and sacral nerve roots and plays a role in stress relief and force transmission.
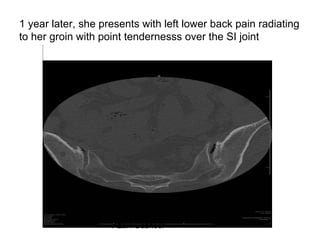
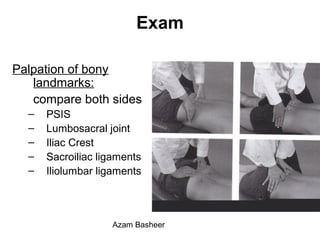
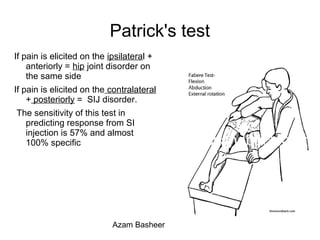
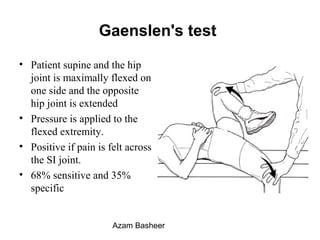
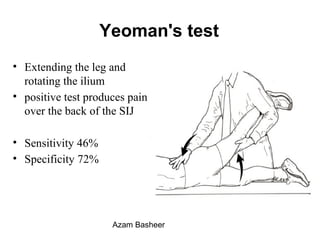
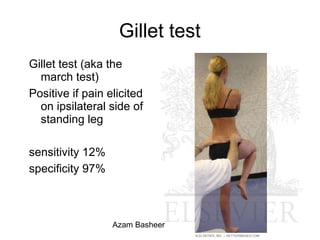
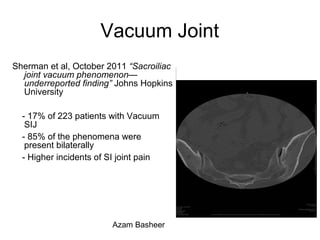
- Evaluation of SIJ pain is challenging due to its anatomy. History, physical exam maneuvers like Patrick's test, and image-guided injections are used to diagnose SIJ pain.
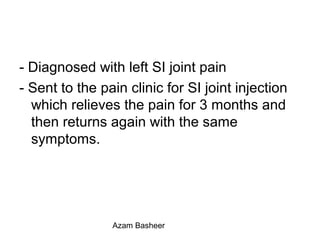
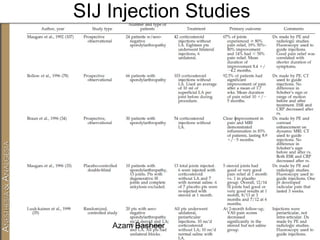
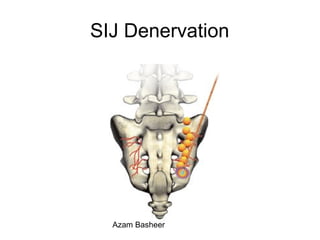
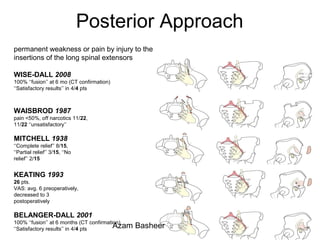
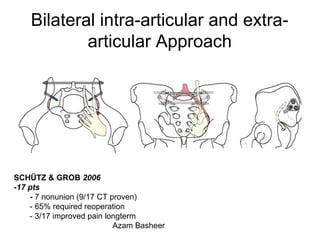
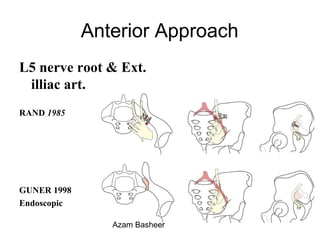
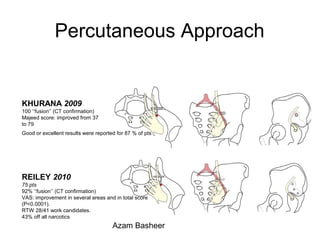
- Treatment options for SIJ pain include conservative care, injections, denervation, and fusion surgery. Per
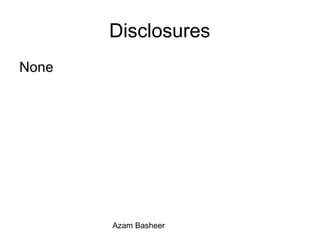

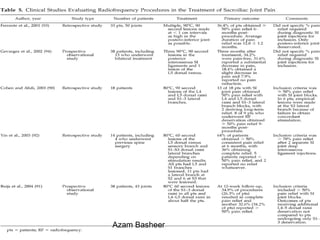


![Summary
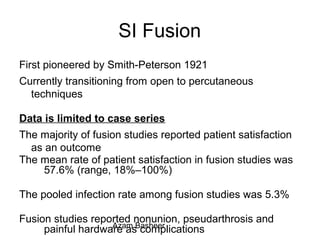
Positive provocative maneuvers combined with 75% pain
relief after image guided SI joint injection is a reliable
method for diagnosing the SI joint as the pain generator
A positive response to low-volume anesthetic injection into
the sacroiliac joint is required before considering
surgery.
Patients should have failed at least 6 months of
conservative treatment (physical therapy, nonsteroidal
anti-inflammatory drugs [NSAIDs], exercise, and
therapeutic injections) before considering surgical fusion
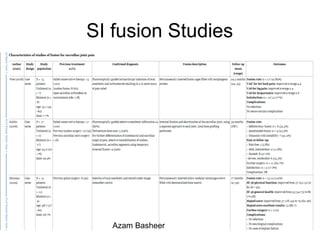
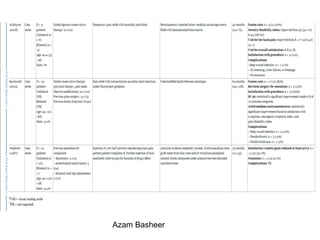
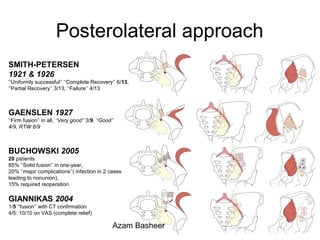
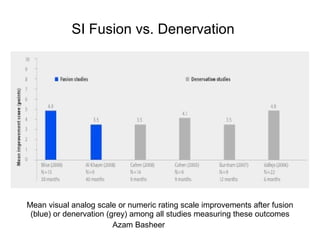
The open fusion studies reported poorer results and higher
complication rates than the percutaneous studies.
Azam Basheer](https://image.slidesharecdn.com/b3f7b43b-7cbd-4631-a627-cb95330fc14c-150401222933-conversion-gate01/85/SI-joint-Fusion-Azam-Basheer-MD-61-320.jpg)