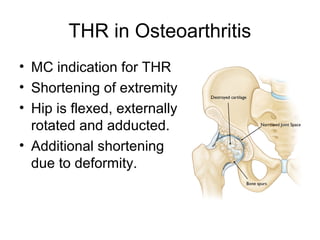
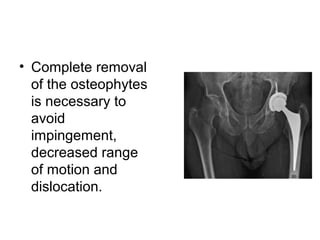
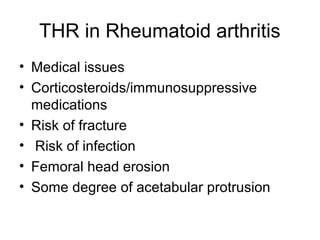
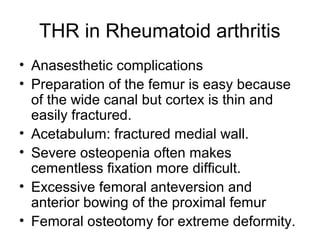
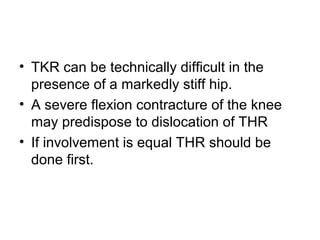
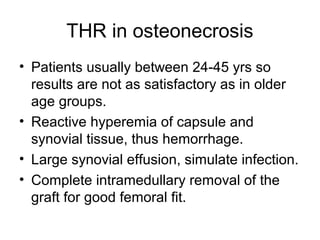
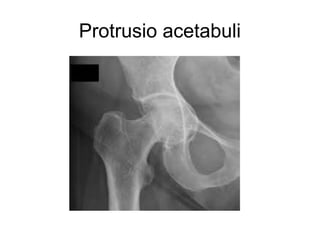
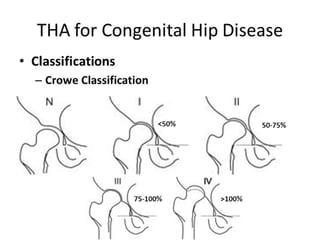
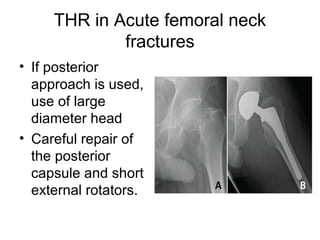
This document discusses techniques for total hip replacement in various hip disorders and conditions. It covers considerations for THR in arthritic conditions like osteoarthritis and rheumatoid arthritis, osteonecrosis, protrusio acetabuli, developmental dysplasia, post-traumatic disorders, failed reconstructive procedures, and infectious disorders. Key points emphasized include the need to modify surgical techniques based on individual conditions, risks like nerve injury or dislocation, and challenges like distorted anatomy that require special approaches.