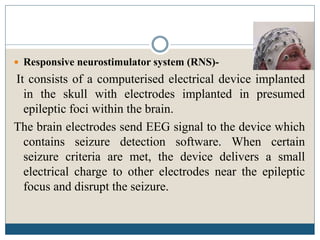
This document discusses recent strategies for treating epilepsy. It begins by introducing epilepsy and classifying seizures. The causes of epilepsy include head injuries, birth trauma, drugs, and interruptions in blood flow to the brain. Conventional antiepileptic drugs effectively control seizures in 75-80% of patients. For the remaining 20-25%, combination therapy or newer antiepileptic drugs may be used. Other treatment strategies discussed include the ketogenic diet, vagus nerve stimulation, responsive neurostimulation, and surgical removal of the seizure focus in intractable cases.