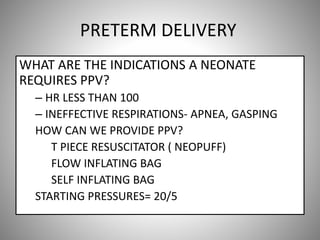
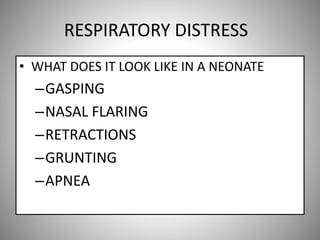
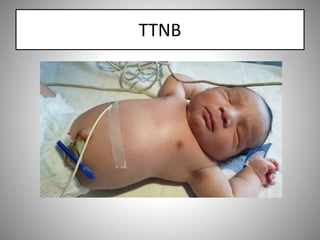
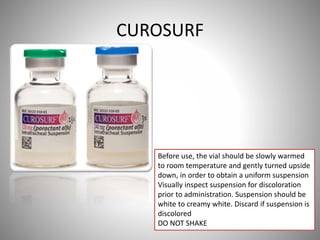
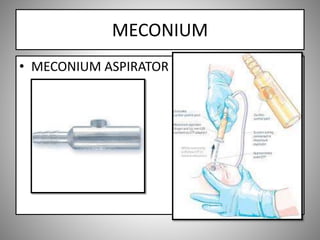
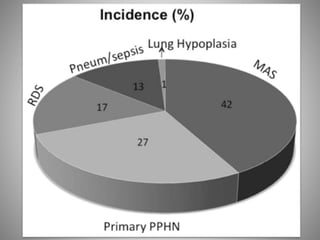
This document provides an overview of neonatal respiratory care training. It covers topics like primary team roles and responsibilities, neonatal disorders/conditions like transient tachypnea of the newborn and respiratory distress syndrome, changes to the NICU respiratory therapy department effective July 1st, and procedures like surfactant administration and meconium suctioning. Key expectations and next steps in training are also outlined.