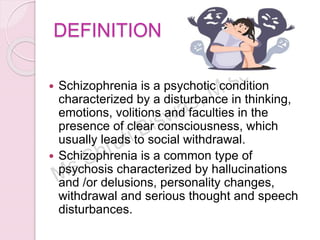
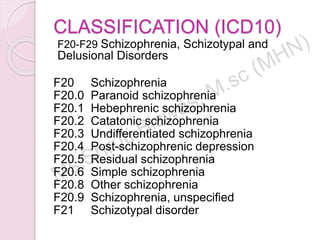
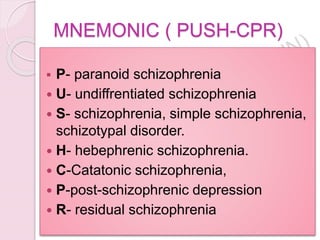
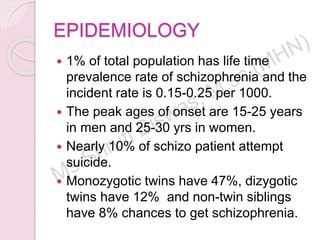
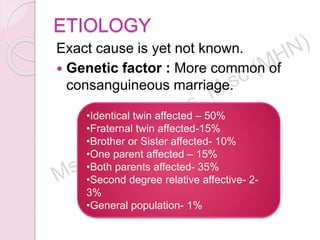
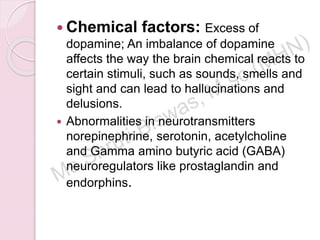
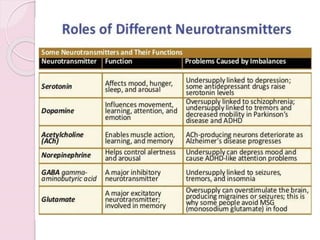
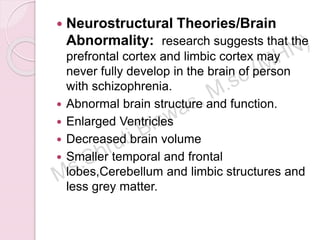
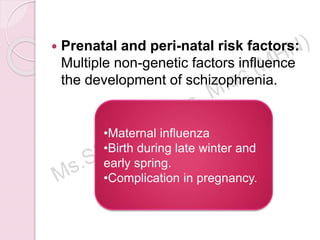
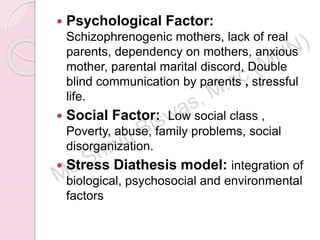
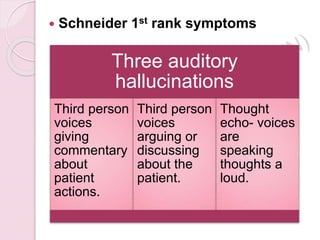
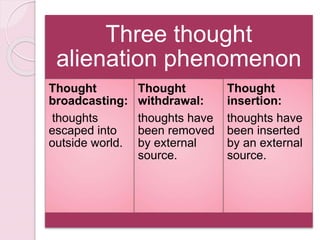
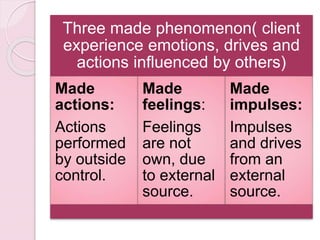
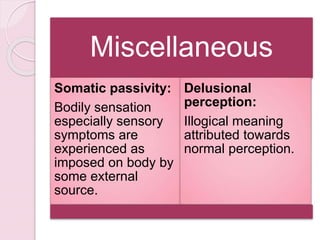
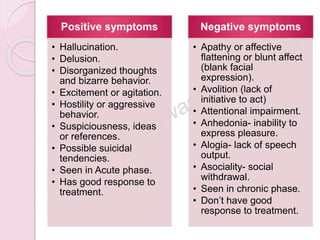
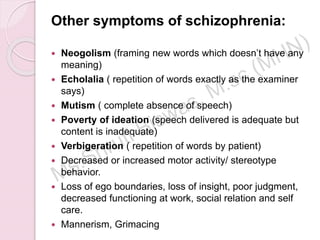
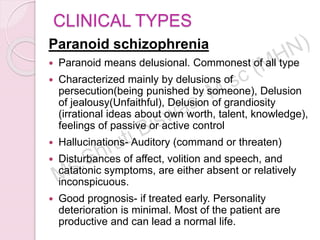
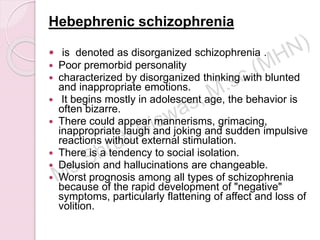
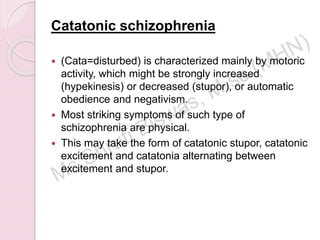
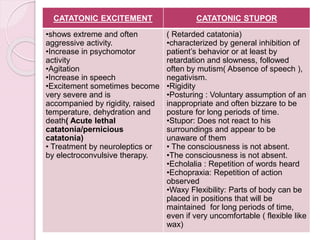
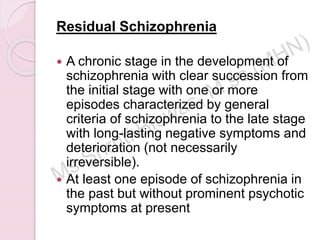
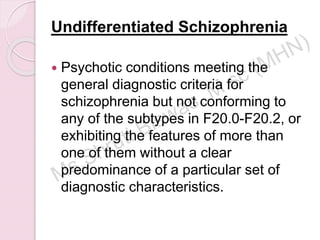
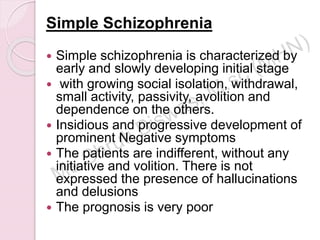
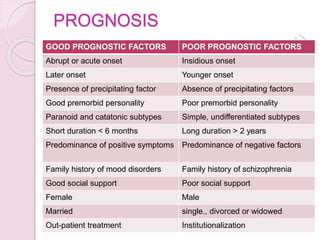
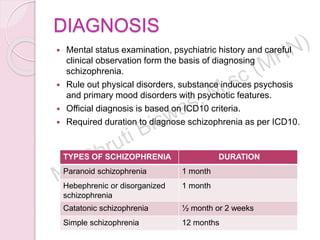
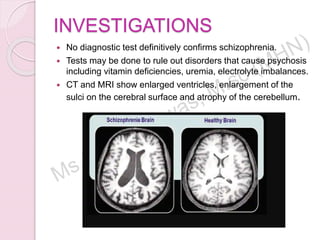
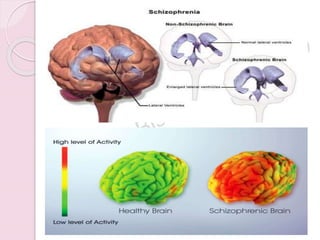
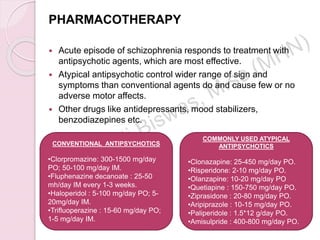
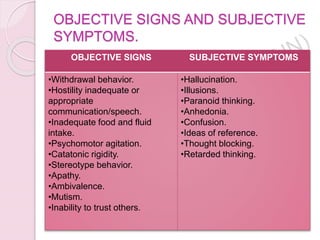
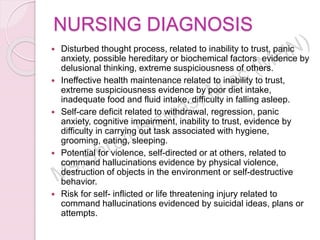
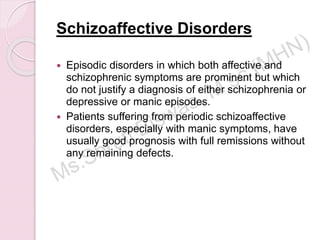
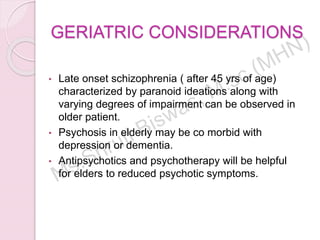
Schizophrenia is a complex psychotic disorder characterized by disturbances in thinking, emotions, and behavior, often leading to social withdrawal and various symptoms such as hallucinations and delusions. It has several subtypes classified in the ICD-10 system, with varying prognoses and treatment responses, and its etiology involves a combination of genetic, chemical, and environmental factors. Diagnosis relies on clinical observation and history, with treatment focusing on reducing symptoms through pharmacotherapy and psychosocial interventions.