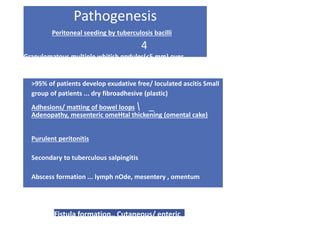
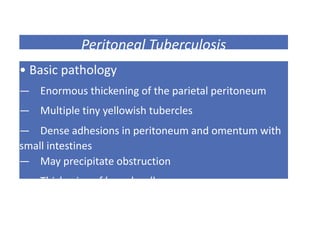
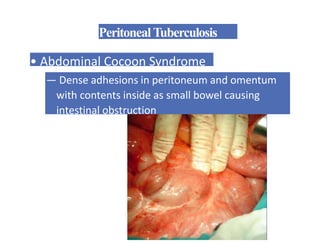
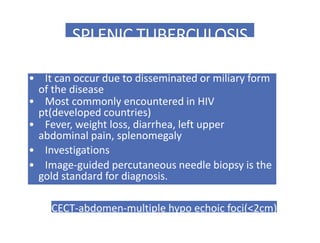
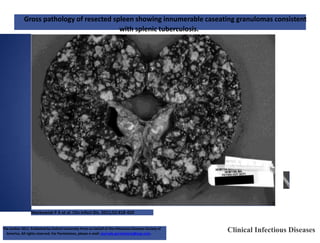
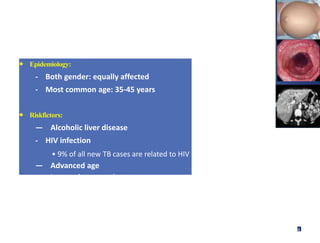
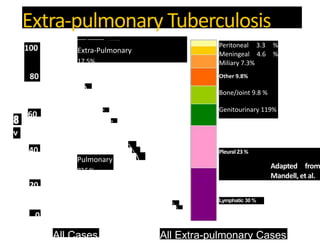
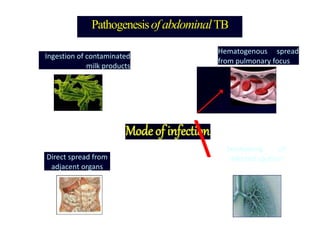
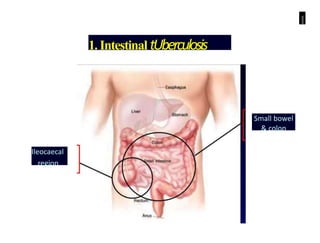
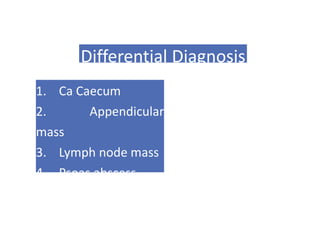
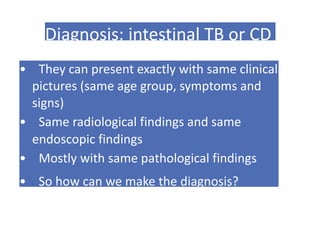
1. Abdominal tuberculosis is a common extrapulmonary manifestation of tuberculosis that can involve the intestines, peritoneum, and lymph nodes.
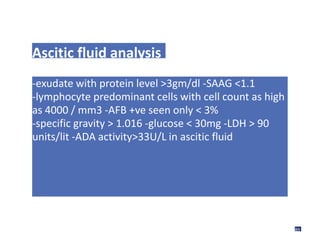
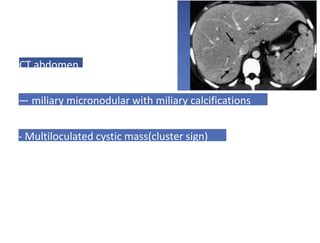
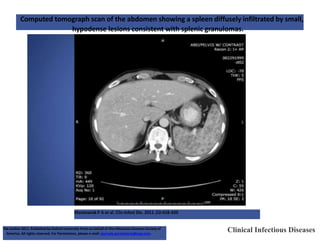
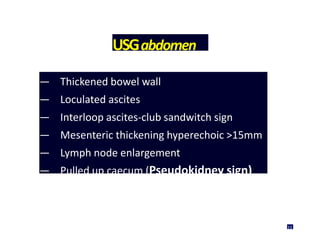
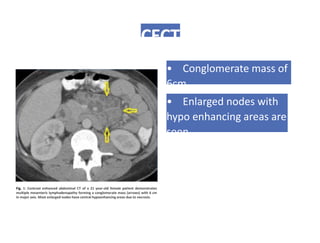
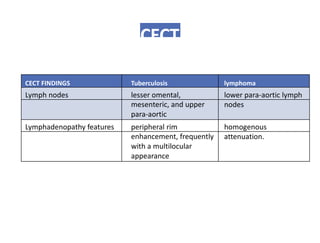
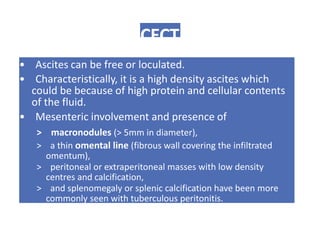
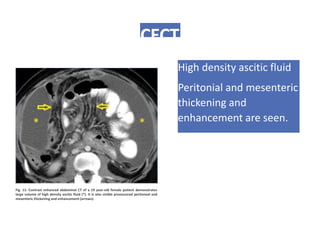
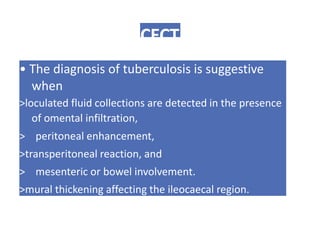
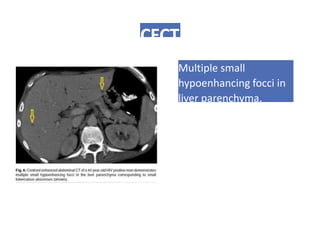
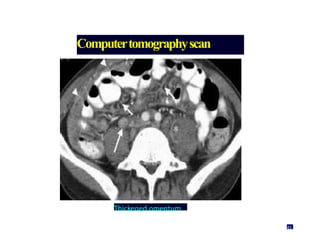
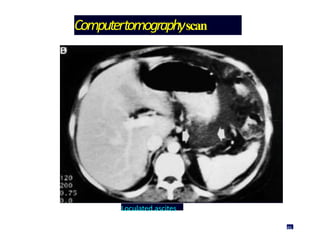
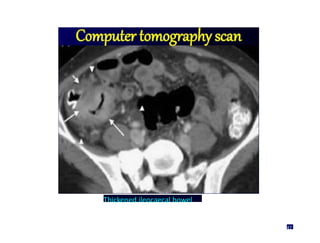
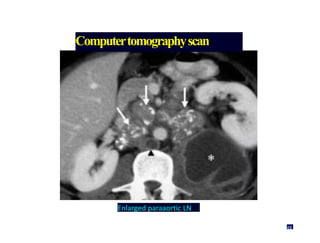
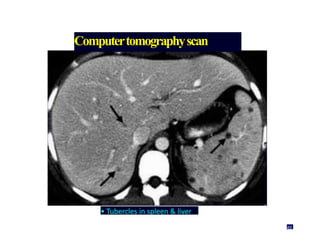
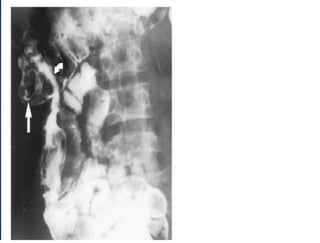
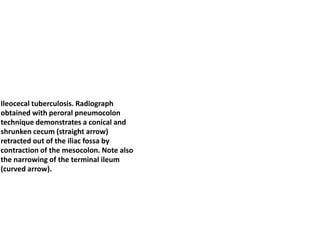
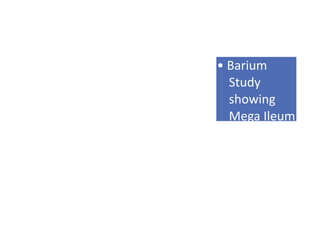
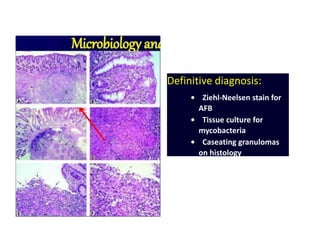
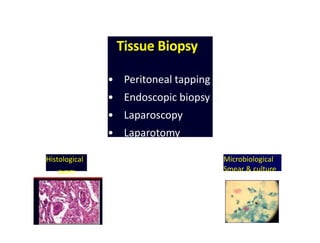
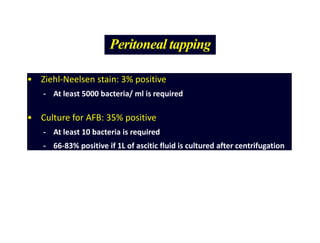
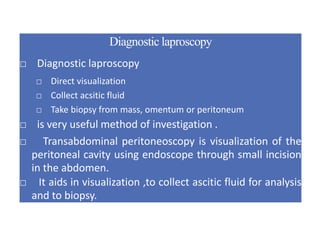
2. Diagnosis is challenging as symptoms can mimic other diseases like Crohn's disease. Imaging findings on ultrasound and CT scan include lymphadenopathy, bowel thickening, ascites, and peritoneal involvement.
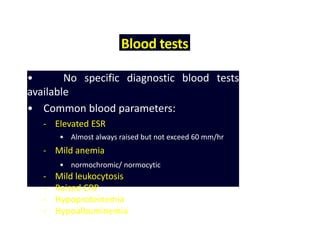
3. While blood tests are nonspecific, presence of ascites, omental thickening, and mesenteric adenopathy on CT scan are suggestive of abdominal tuberculosis.












![Antituberculosis Drugs
Drug/Form ulation Adult Dosage (Daily) Main Adverse Effects
First-Line Drugs
Hepatic toxicity,
Isoniazid (INH)[*] 5
mg/kg (max 300 mg)
PO, IM, IV peripheral
neuropathy
100, 300 mg tabs
50 mg/5 mL syrup
100 mg/mL injection
Rifampin (Rifadin,
Rimactane) 10
mg/kg (max 600
mg) PO, IV Hepatic
toxicity,
flulike syndrome,
pruritus
150, 300 mg caps
600 mg injection
powder
72](https://image.slidesharecdn.com/abdominaltuberculosis-171229125201-221213123527-bc4d15ab/85/abdominaltuberculosis-75-320.jpg)
![Pyrazinamide 500 mg tabs 20-25 mg/kg PO Arthralgias, hepatic
toxicity, hyperuricemia,
gastrointestinal upset
Ethambutol[*] (Myambutol) 100, 400
mg tabs
15-25 mg/kg PO
Decreased red-green color
discrimination, decreased
visual acuity
73](https://image.slidesharecdn.com/abdominaltuberculosis-171229125201-221213123527-bc4d15ab/85/abdominaltuberculosis-76-320.jpg)


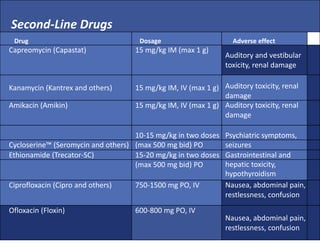
![Drug Dosage Adverse effect
Levofloxacin (Levaquin) 500-1000 mg PO, IV Nausea, abdominal pain,
restlessness, confusion
Gatifloxacin™ (Tequin) 400 mg PO, IV
Nausea, abdominal pain,
restlessness, confusion
Moxifloxacinm] (Avelox)
Aminosalicylic acid (PAS; Paser)
400 mg PO, IV 8-12 g in
2-3 doses PO
Nausea, abdominal pain,
restlessness, confusion
Gastrointestinal disturbance
76](https://image.slidesharecdn.com/abdominaltuberculosis-171229125201-221213123527-bc4d15ab/85/abdominaltuberculosis-80-320.jpg)