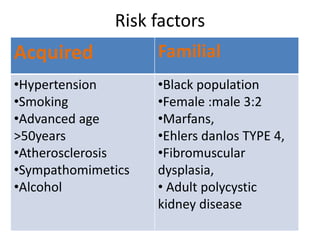
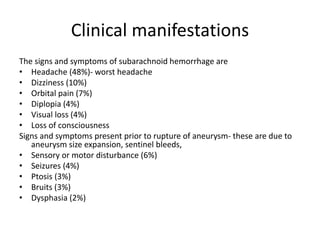
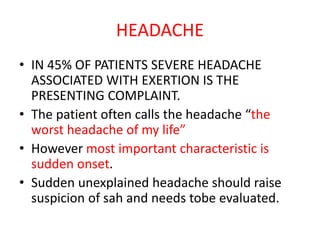
1. A 50-year-old female smoker with hypertension presented with sudden severe headache and brief loss of consciousness at work. She was found to have subarachnoid hemorrhage.
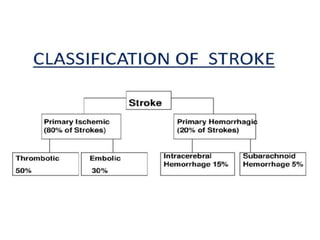
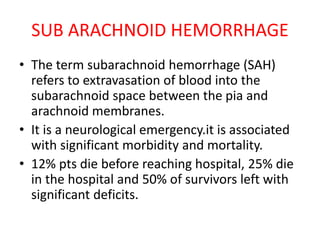
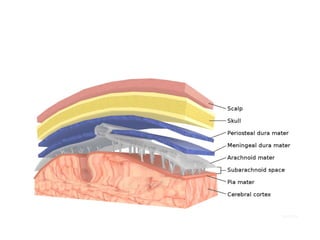
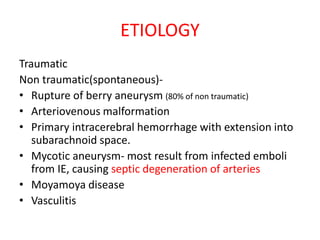
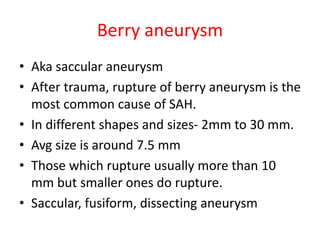
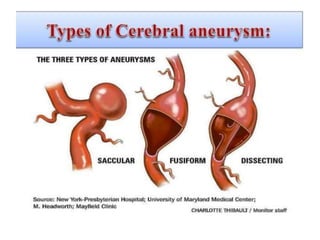
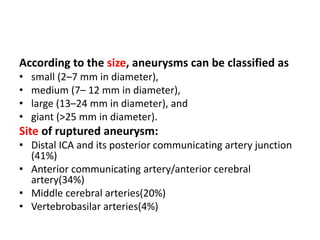
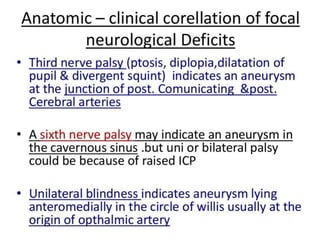
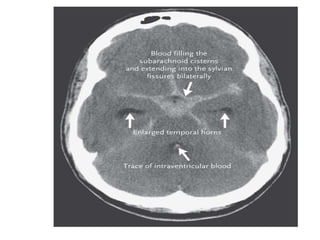
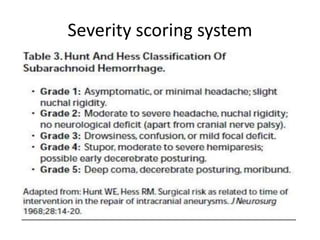
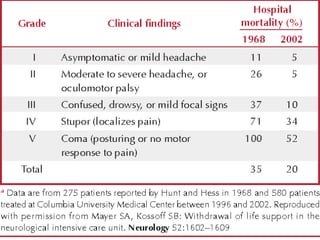
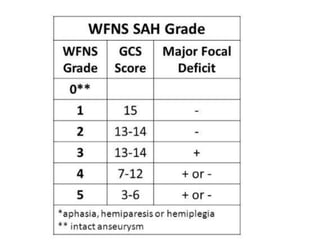
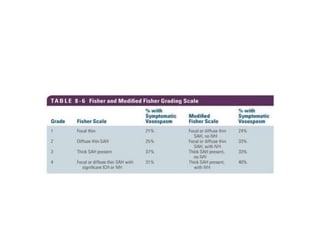
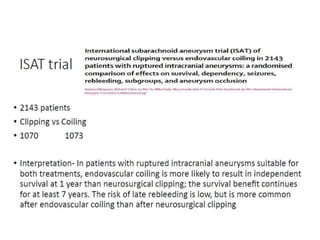
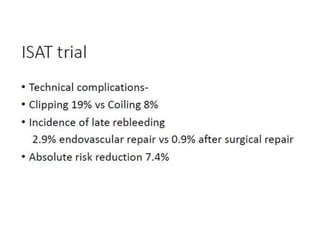
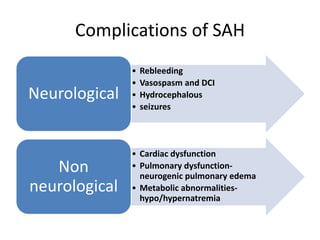
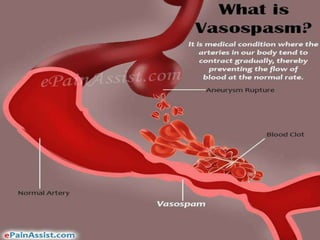
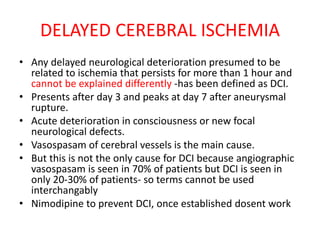
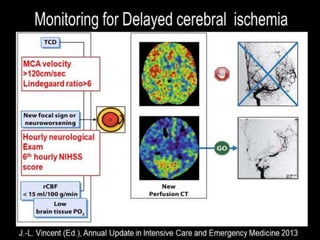
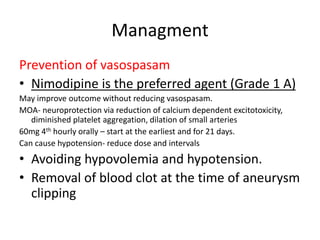
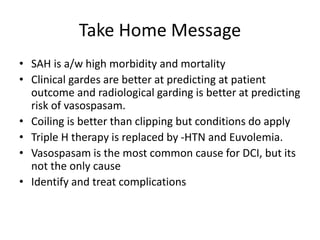
2. Subarachnoid hemorrhage is a neurological emergency caused by bleeding into the subarachnoid space, usually from a ruptured berry aneurysm. It requires rapid diagnosis and treatment to prevent rebleeding, vasospasm, and other complications.
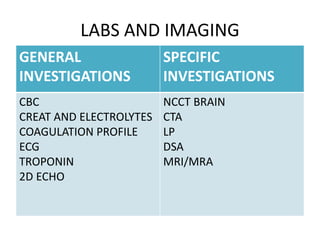
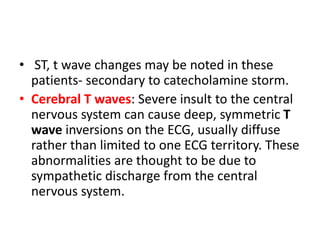
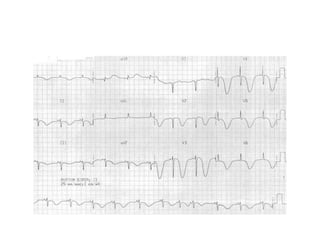
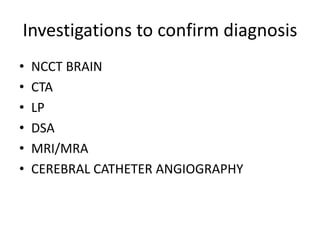
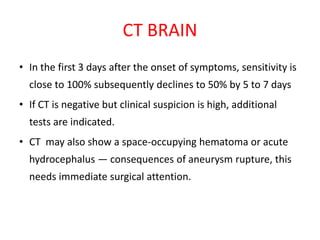
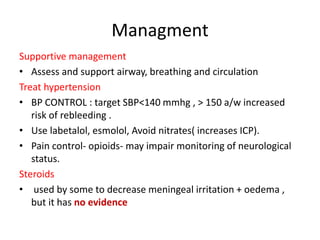
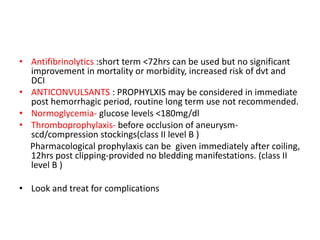
3. Diagnostic tests included a non-contrast CT, which was positive, as well as a CTA and lumbar puncture to confirm the diagnosis and identify the source of bleeding. The patient was treated supportively in the ICU to control