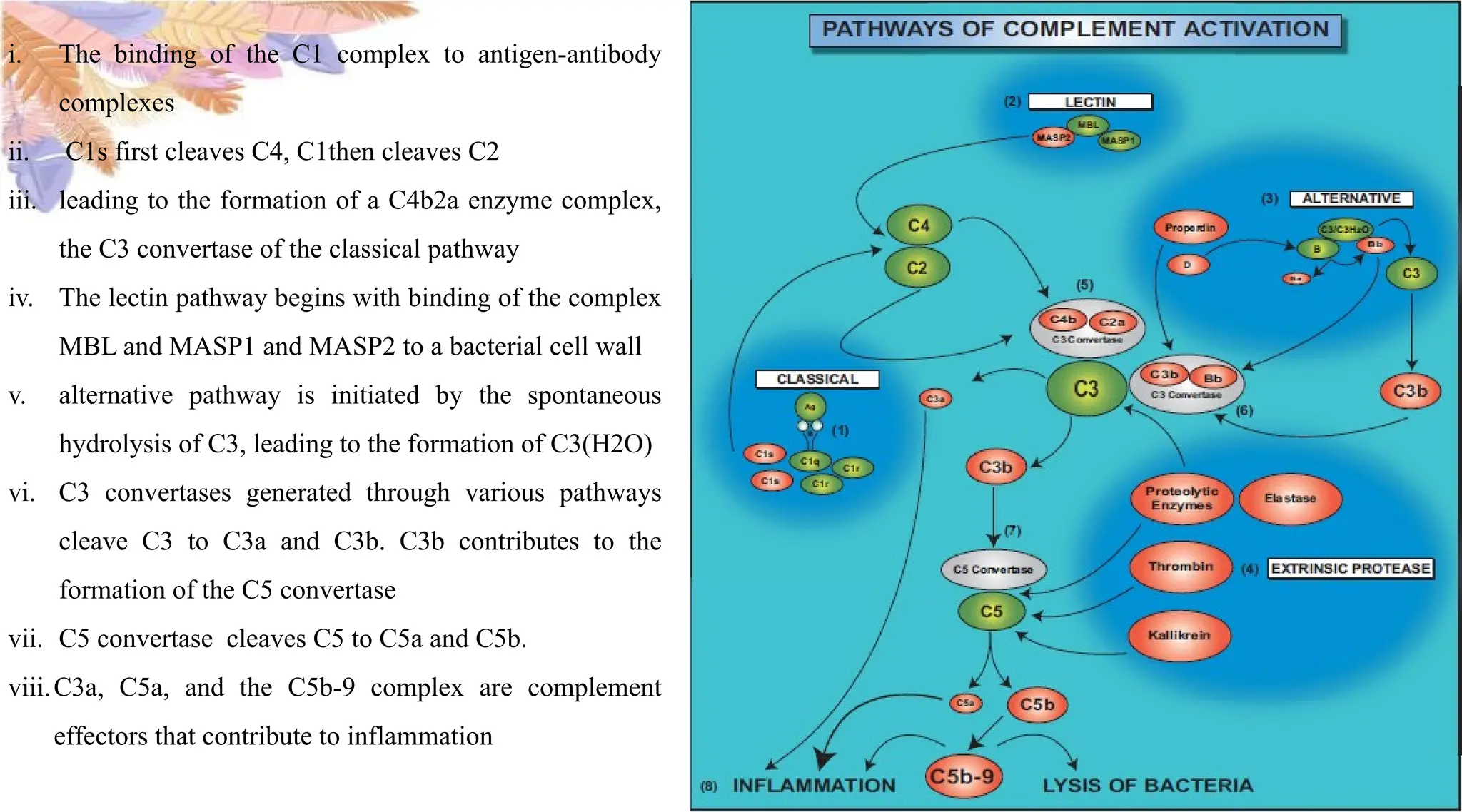
The document discusses the role of the complement system in acute inflammation, highlighting its function in defending against infections and tissue injury through various mechanisms, such as increasing vascular permeability and recruiting leukocytes. It outlines the phases of inflammation, the mediators involved, and the pathways of complement activation, emphasizing the consequences of acute inflammation, including resolution or progression to chronic inflammation. The importance of complement in regulating inflammatory responses is also addressed, demonstrating its critical contribution to both innate immunity and inflammation.