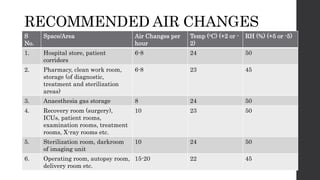
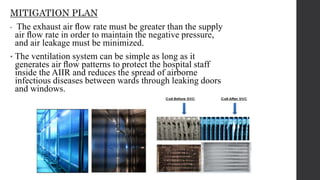
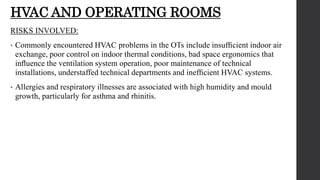
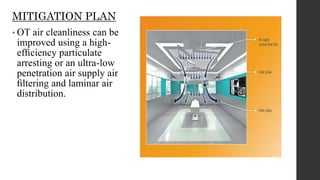
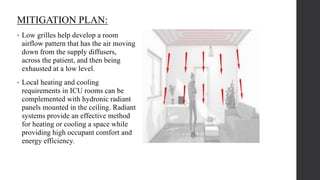
The document outlines the importance of HVAC systems in hospitals for maintaining air quality and preventing infections. It discusses risks associated with HVAC systems, including airborne diseases and contamination during surgeries, and provides mitigation plans to improve air flow, filtration, and temperature control in various hospital areas. Recommendations include specific air change rates for different spaces and measures to enhance safety in operating rooms, intensive care units, and emergency departments.
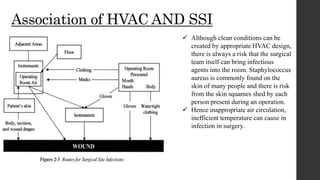
![Association of HAI and HVAC:
Some of the ways that potentially
infectious microorganisms can be spread
in a health care environment include
• sneezes and coughs
• inhalation
• Contact
• deposition in surgical site or open
wound
• water mist
• insect bite.
HVAC systems can impact HAIs by
affecting
• dilution (by ventilation)
• air quality (by filtration)
• exposure time (by air change and
pressure differential)
• temperature
• humidity
• organism viability (by ultraviolet [UV]
treatment)
• airflow patterns.](https://image.slidesharecdn.com/riskwithhvacsystemandmitigationplan-190104113949/85/Risk-with-hvac-system-and-mitigation-plan-5-320.jpg)