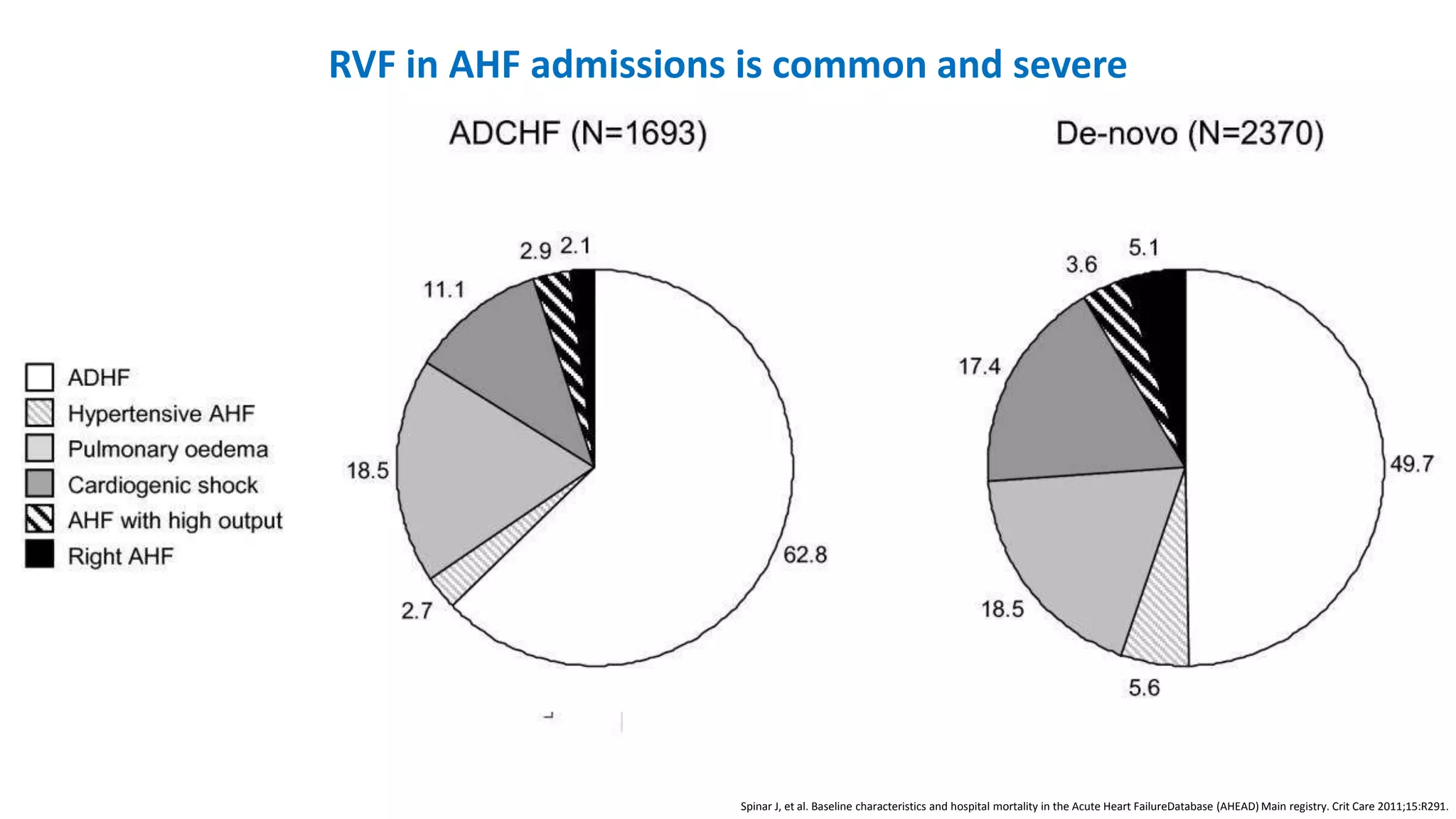
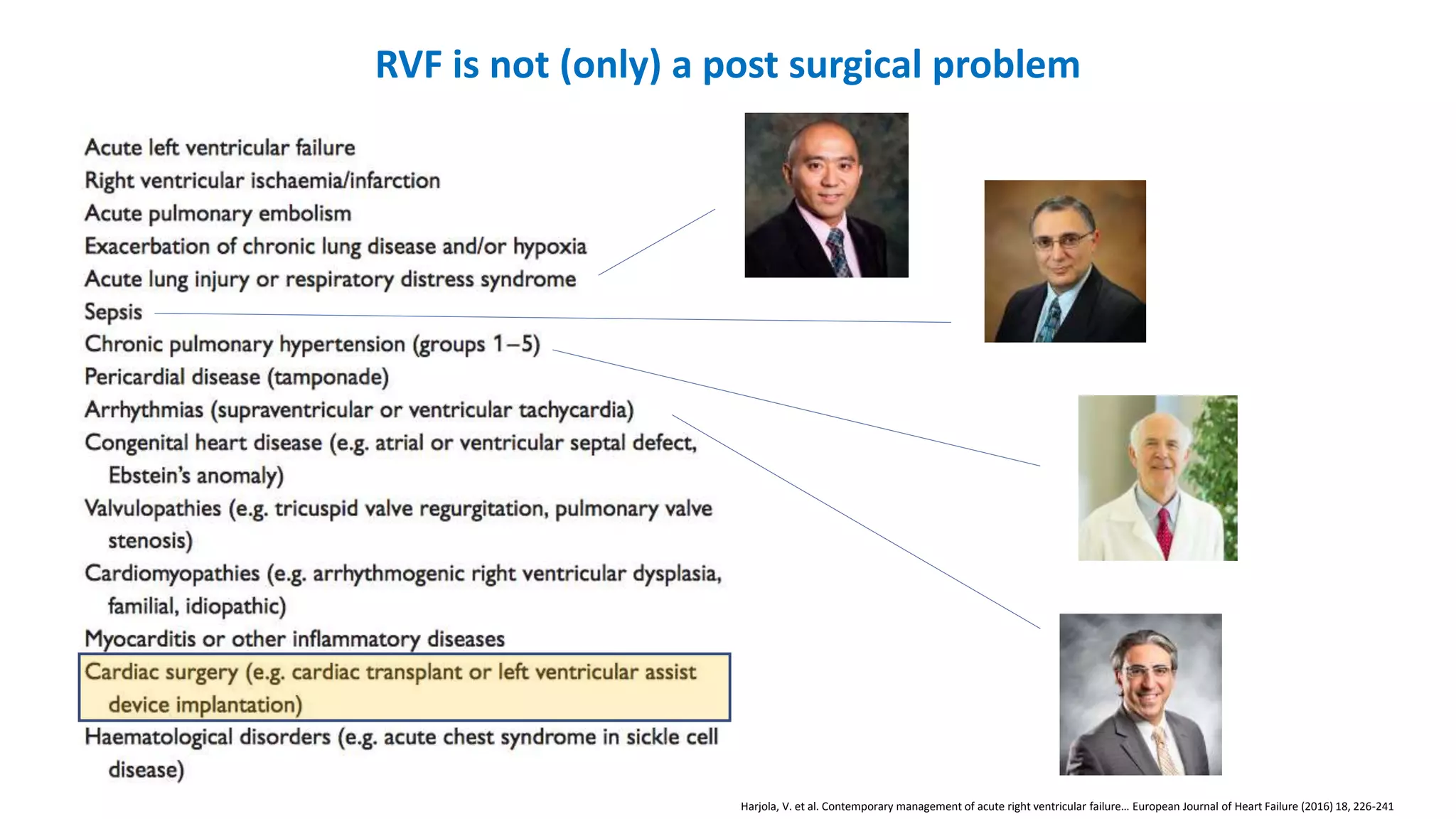
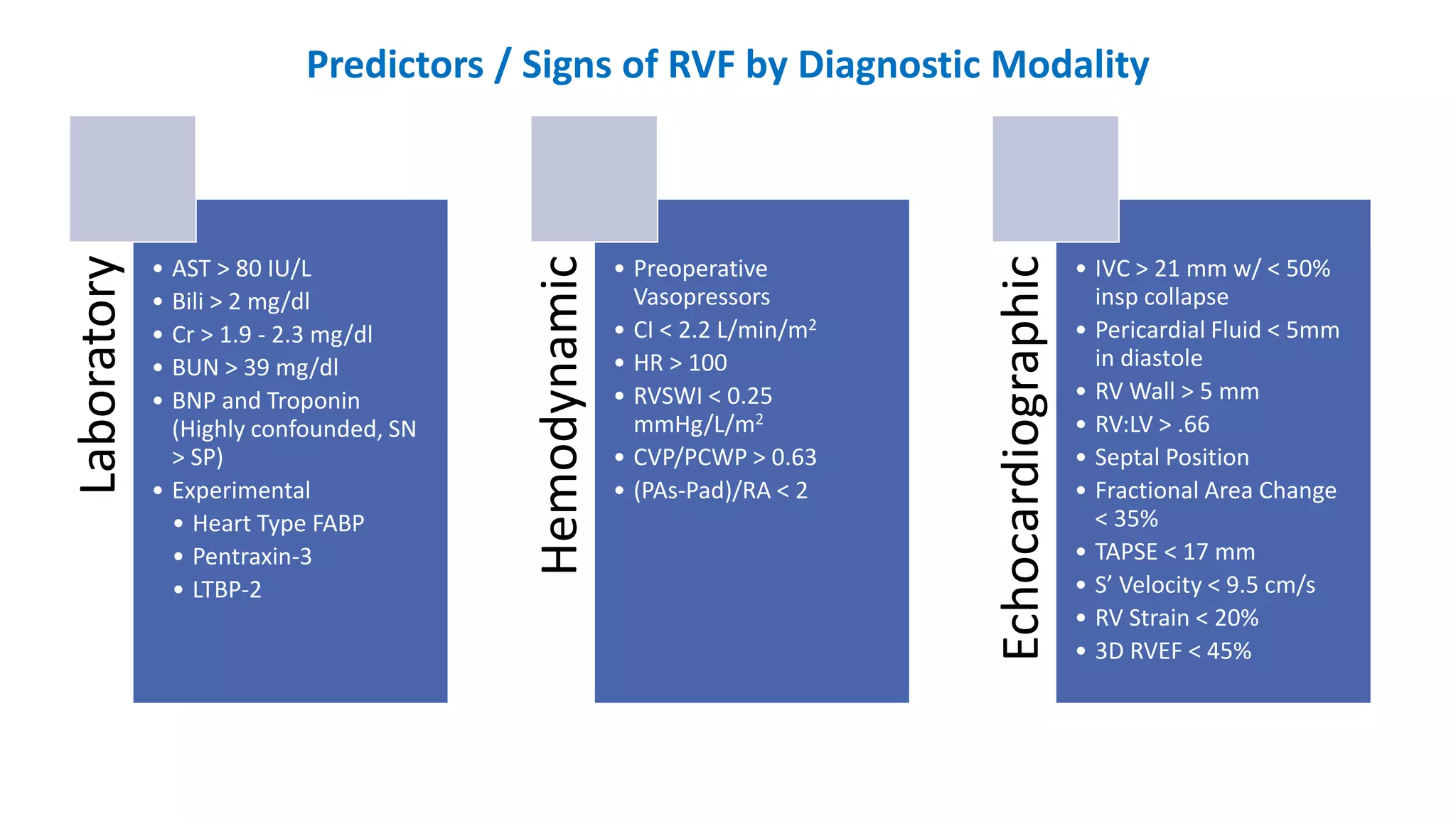
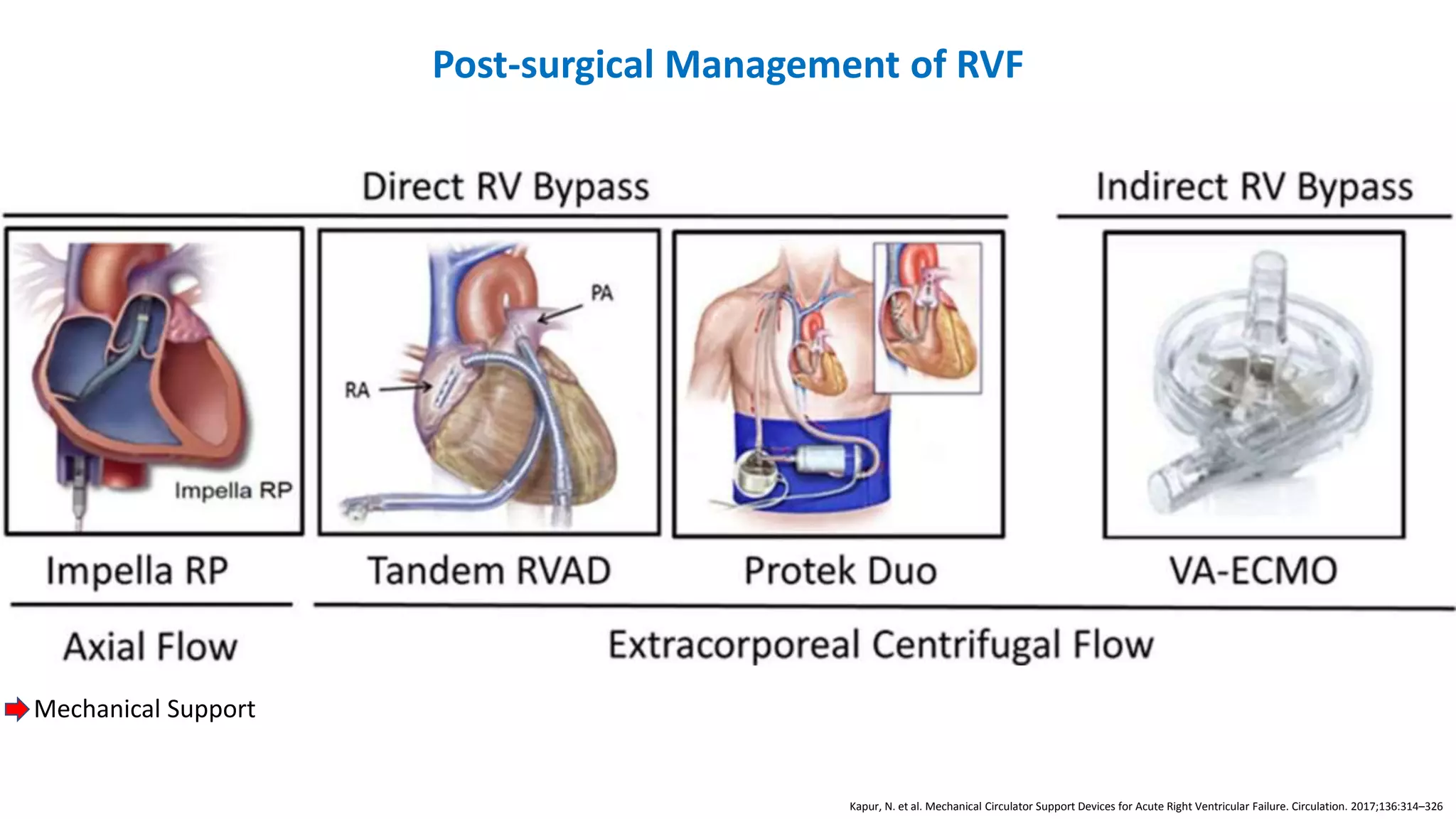
The document discusses right ventricular failure (RVF) after cardiac surgery. It begins by outlining risk factors and the dynamics that lead to RVF. It describes how to assess the severity of RVF using laboratory, hemodynamic, and echocardiographic data. The document concludes by discussing the management of RVF in postsurgical patients, which involves optimizing volume status, rhythm control, afterload reduction, RV perfusion, contractility, and the potential use of mechanical support devices if needed.