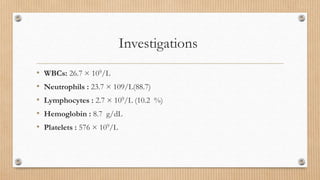
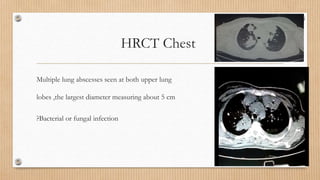
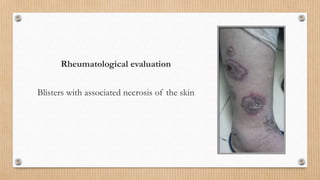
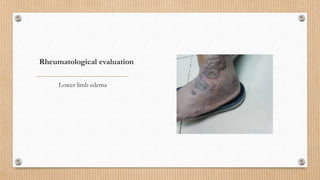
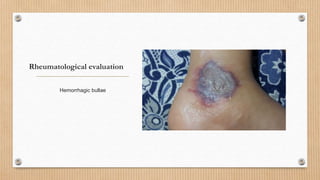
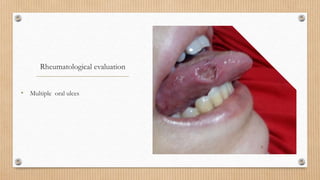
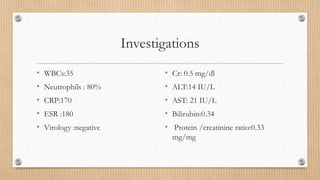
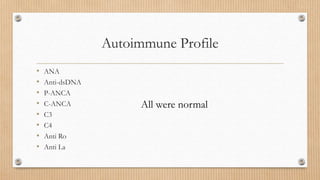
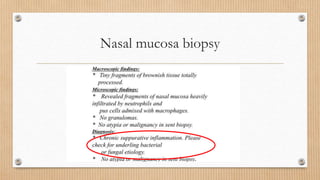
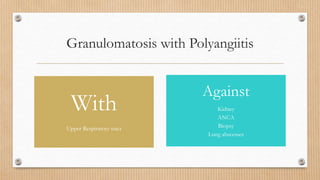
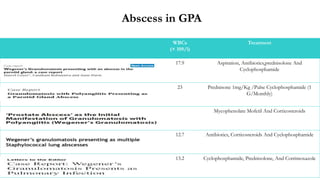
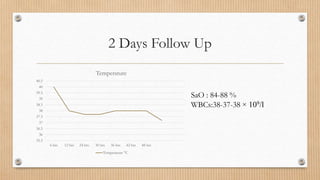
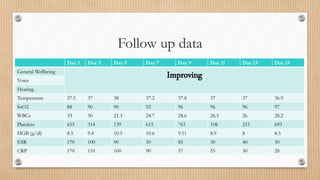
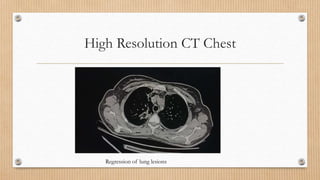
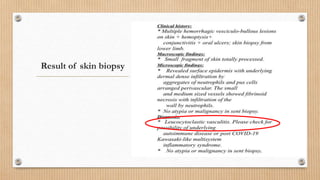
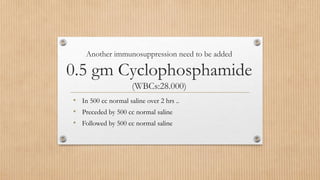
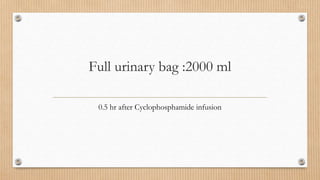
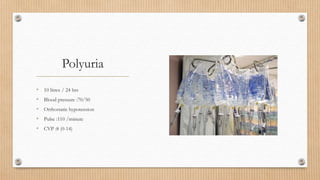
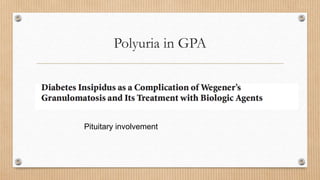
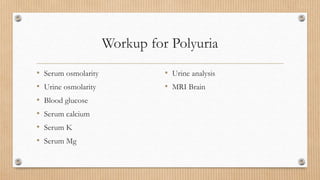
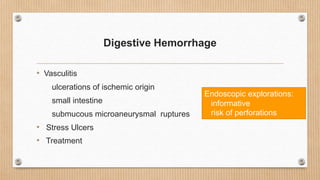
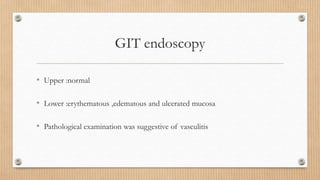
This case study describes a 37-year-old female patient who presented with fever, cough, and respiratory distress. Imaging showed multiple lung abscesses. She did not respond to antibiotic treatment and her condition deteriorated, developing skin lesions. A rheumatology consultation determined she had granulomatosis with polyangiitis (GPA) based on biopsy results. She received high-dose steroids and cyclophosphamide, with improvement. However, she developed polyuria after cyclophosphamide and bleeding after further treatment, which were complications of her GPA involving other organs. Her condition continued improving with conservative management.