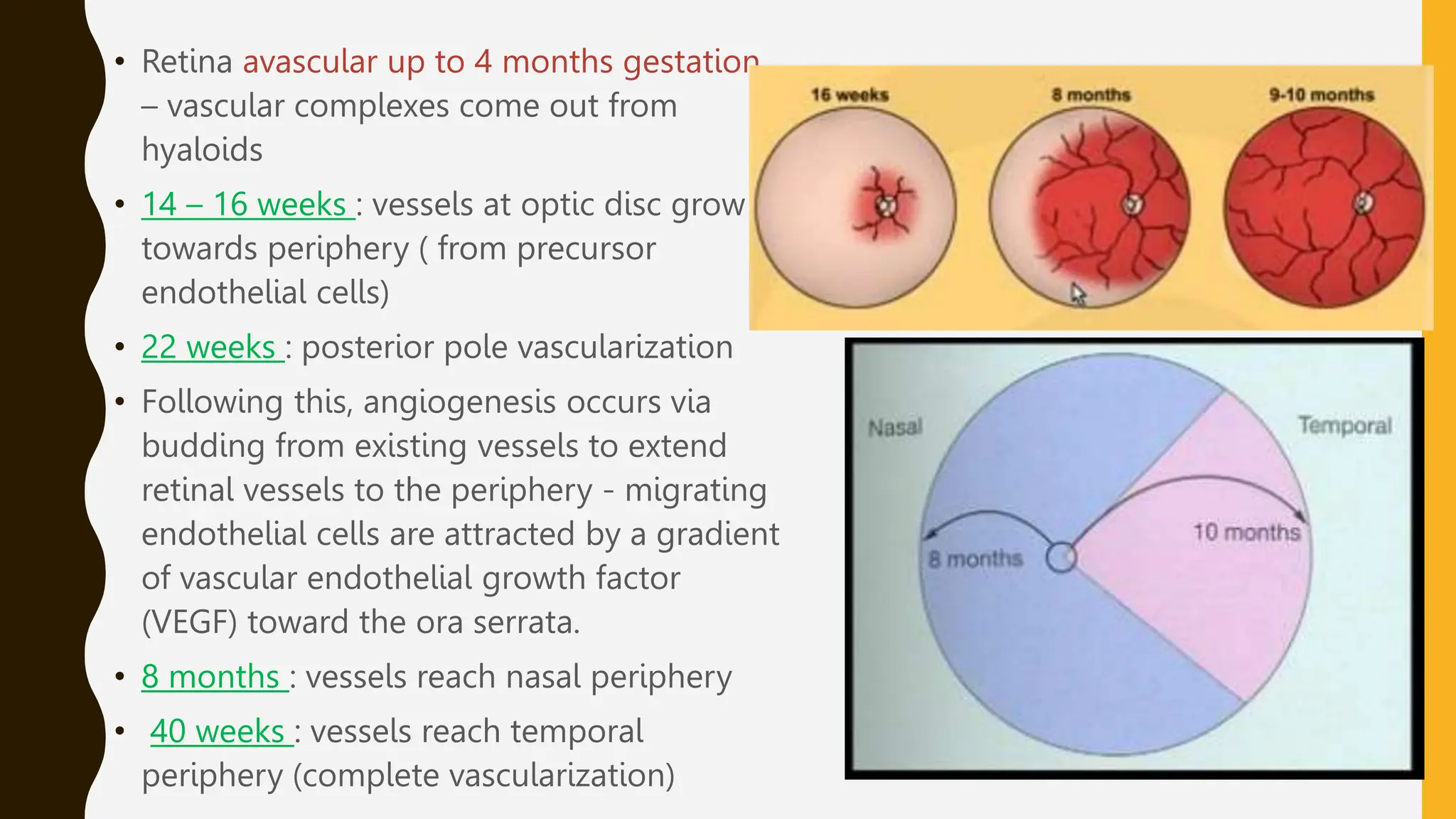
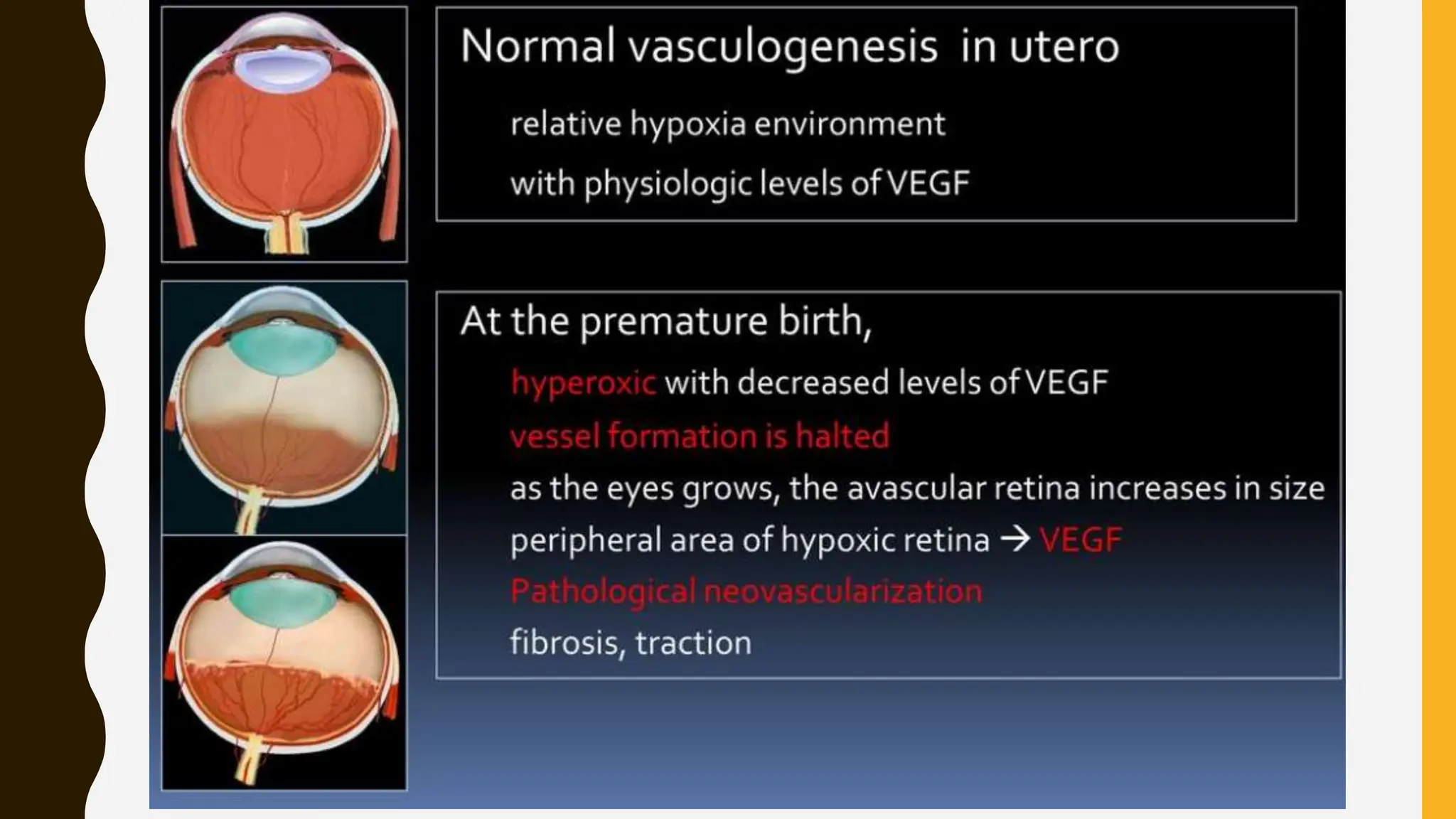
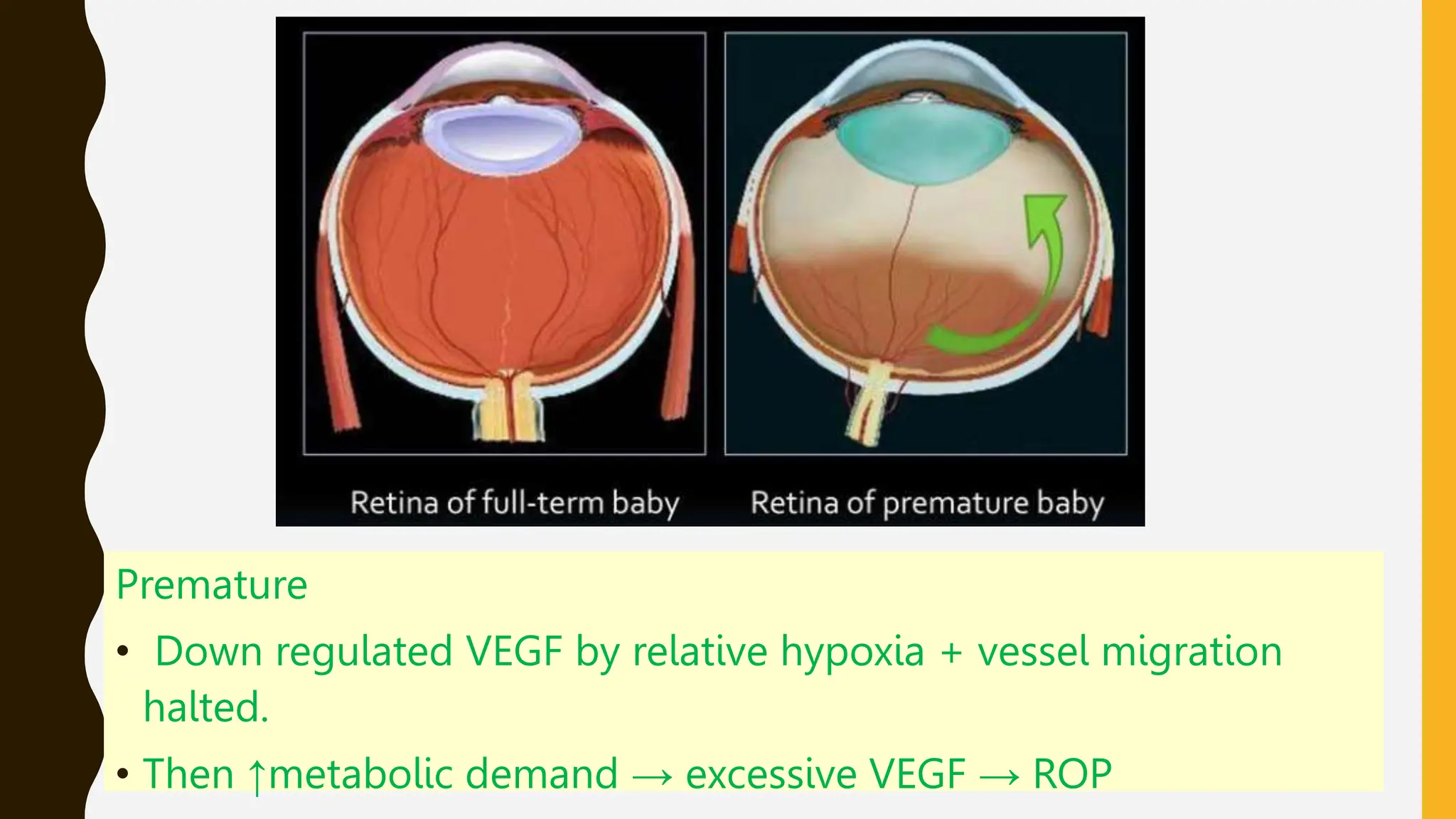
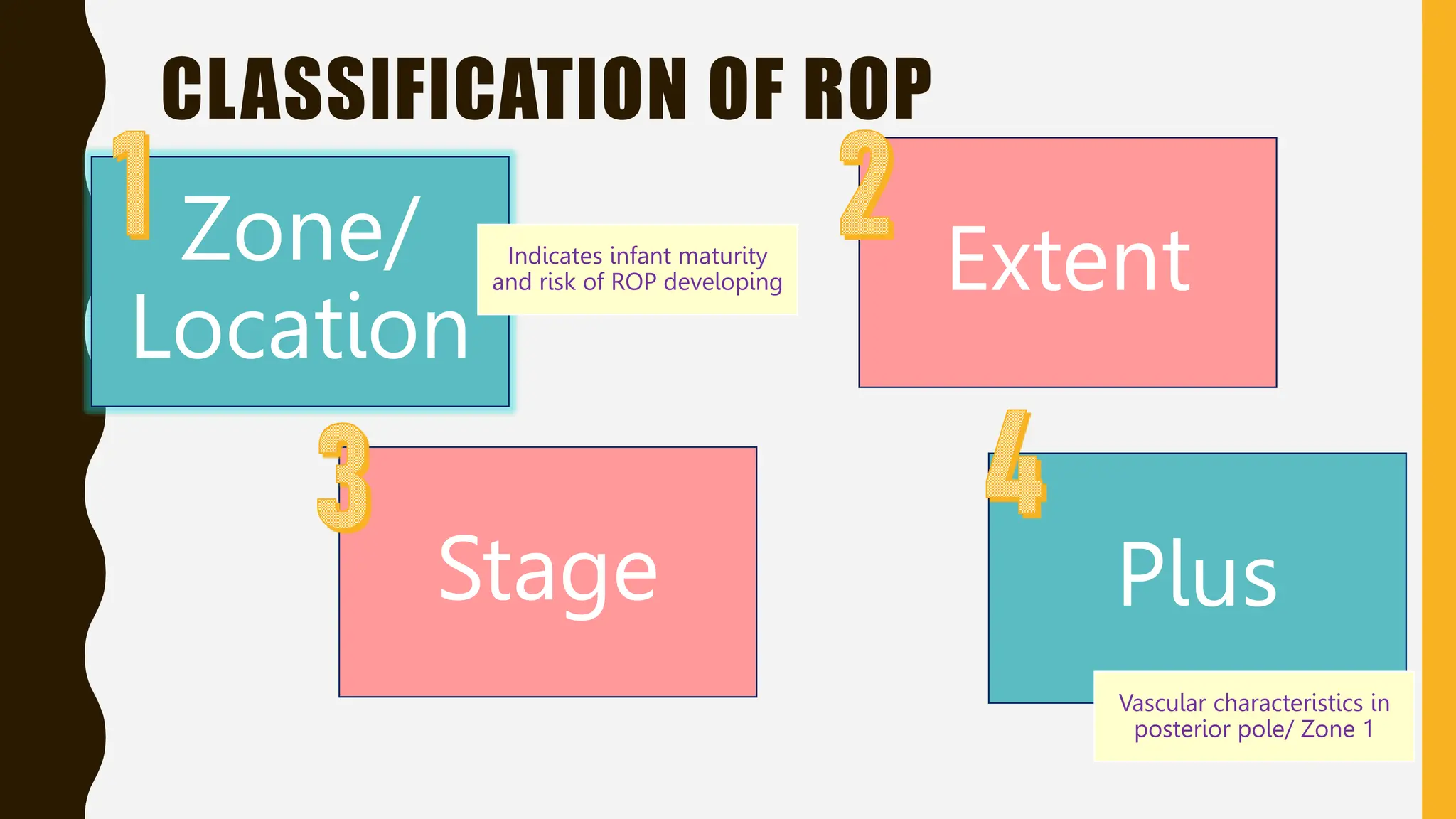
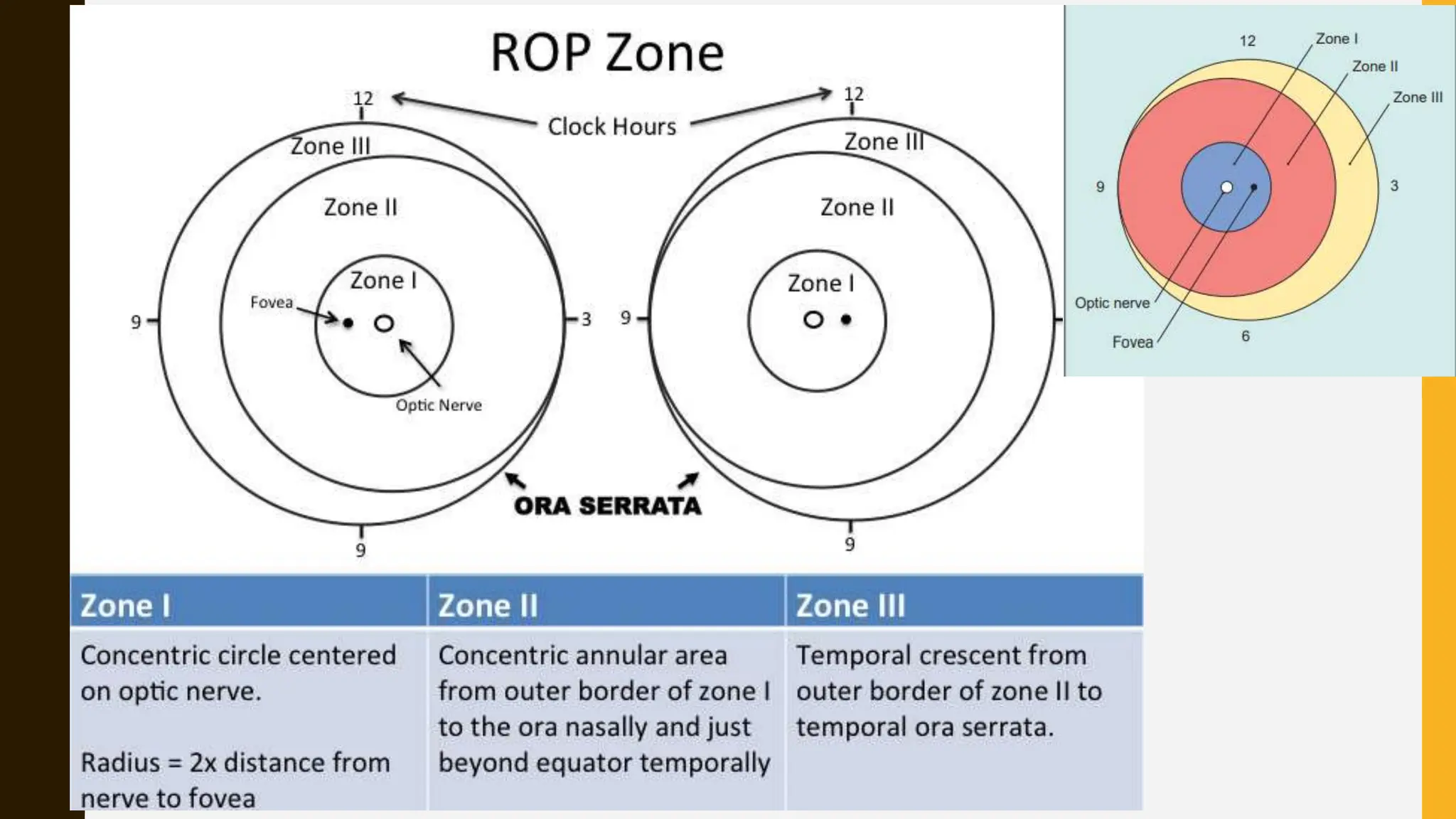
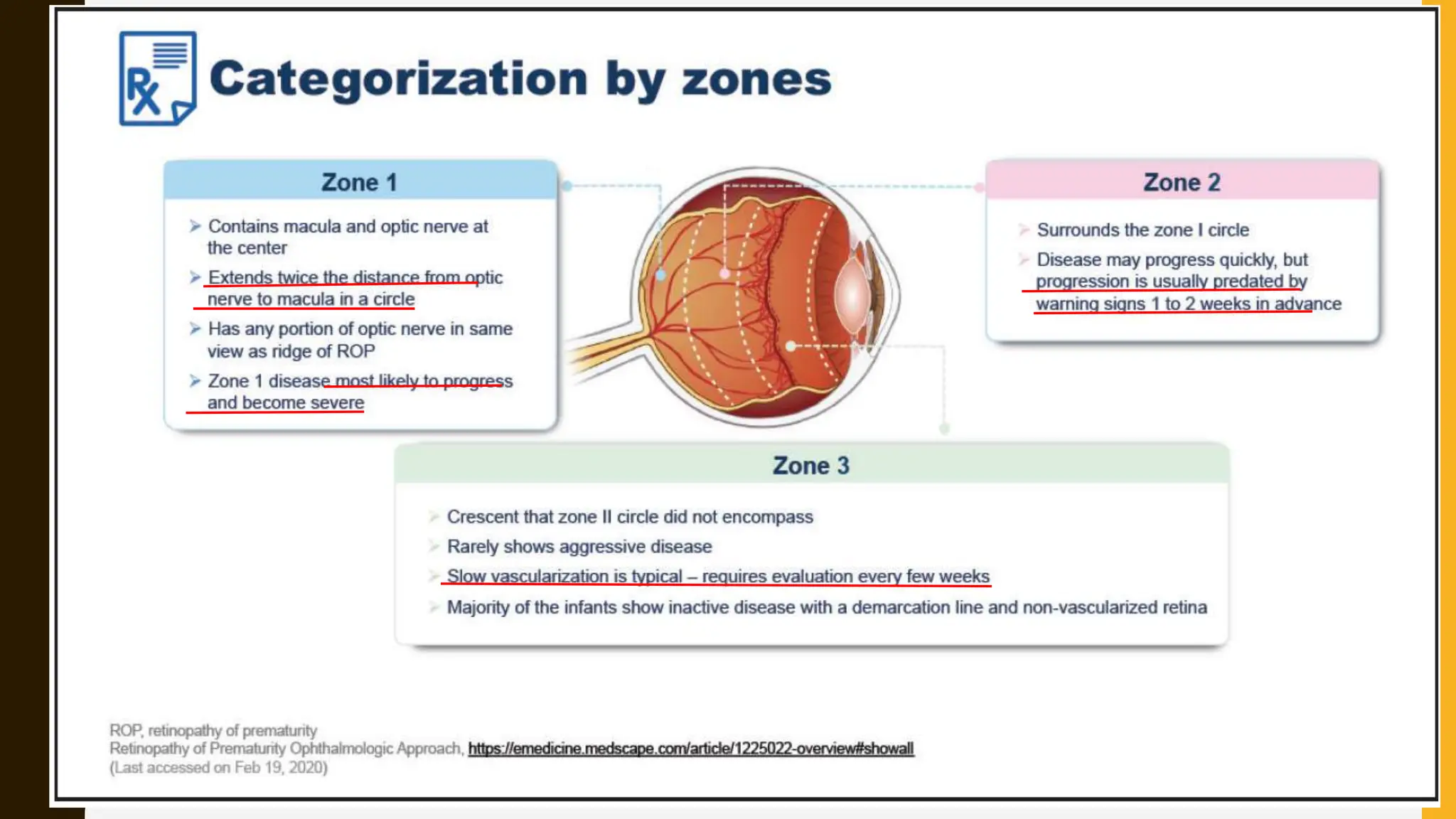
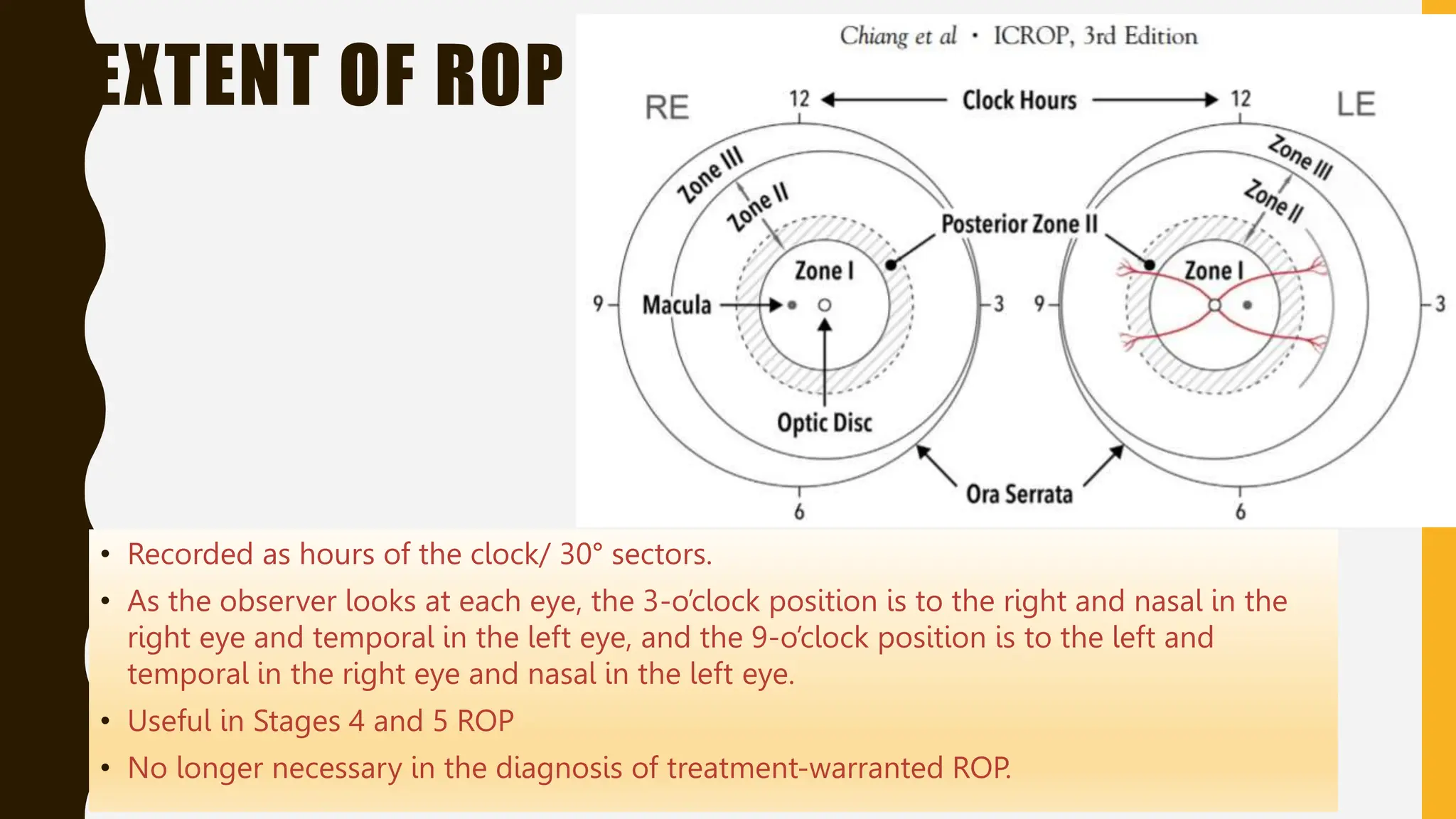
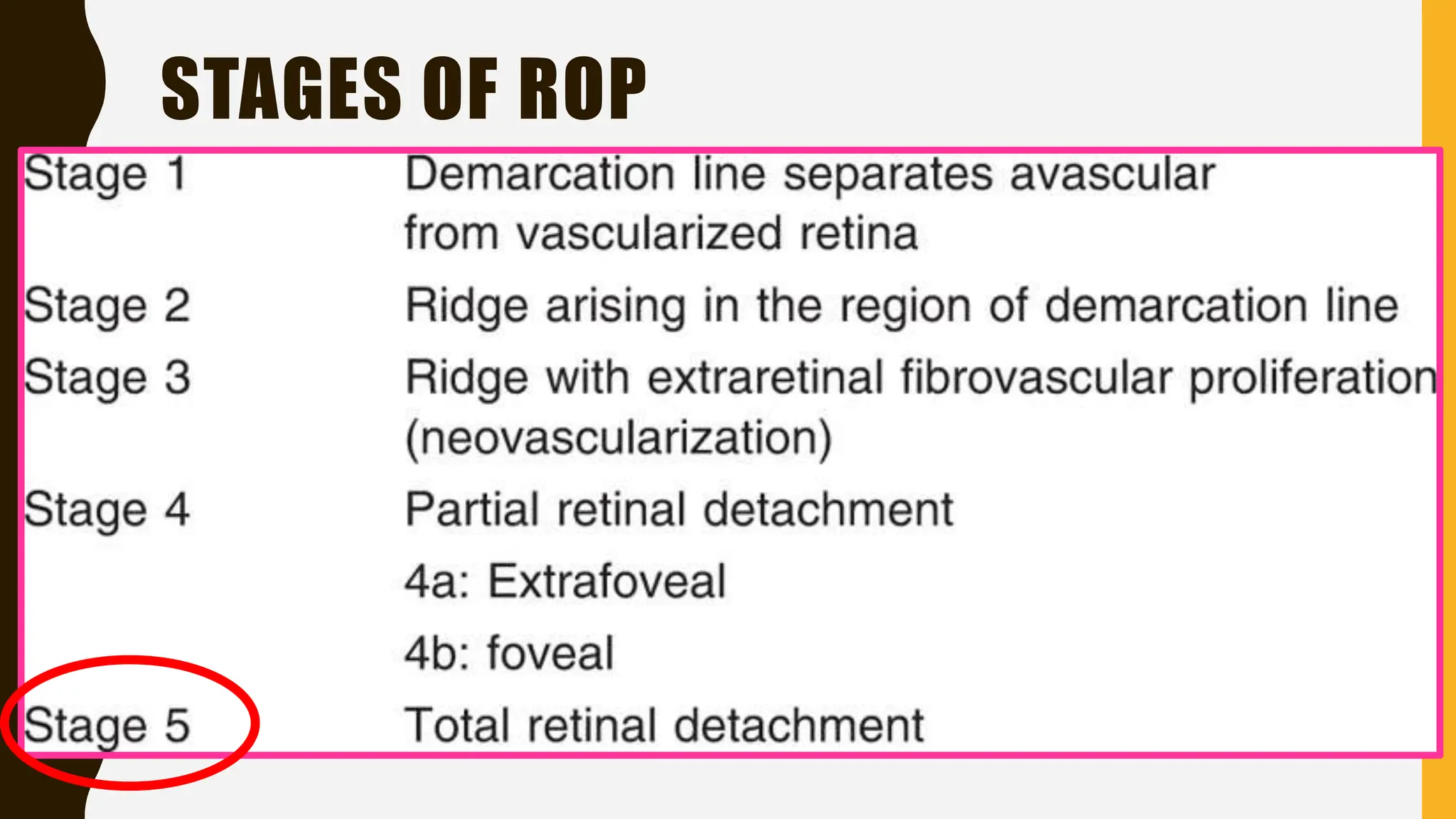
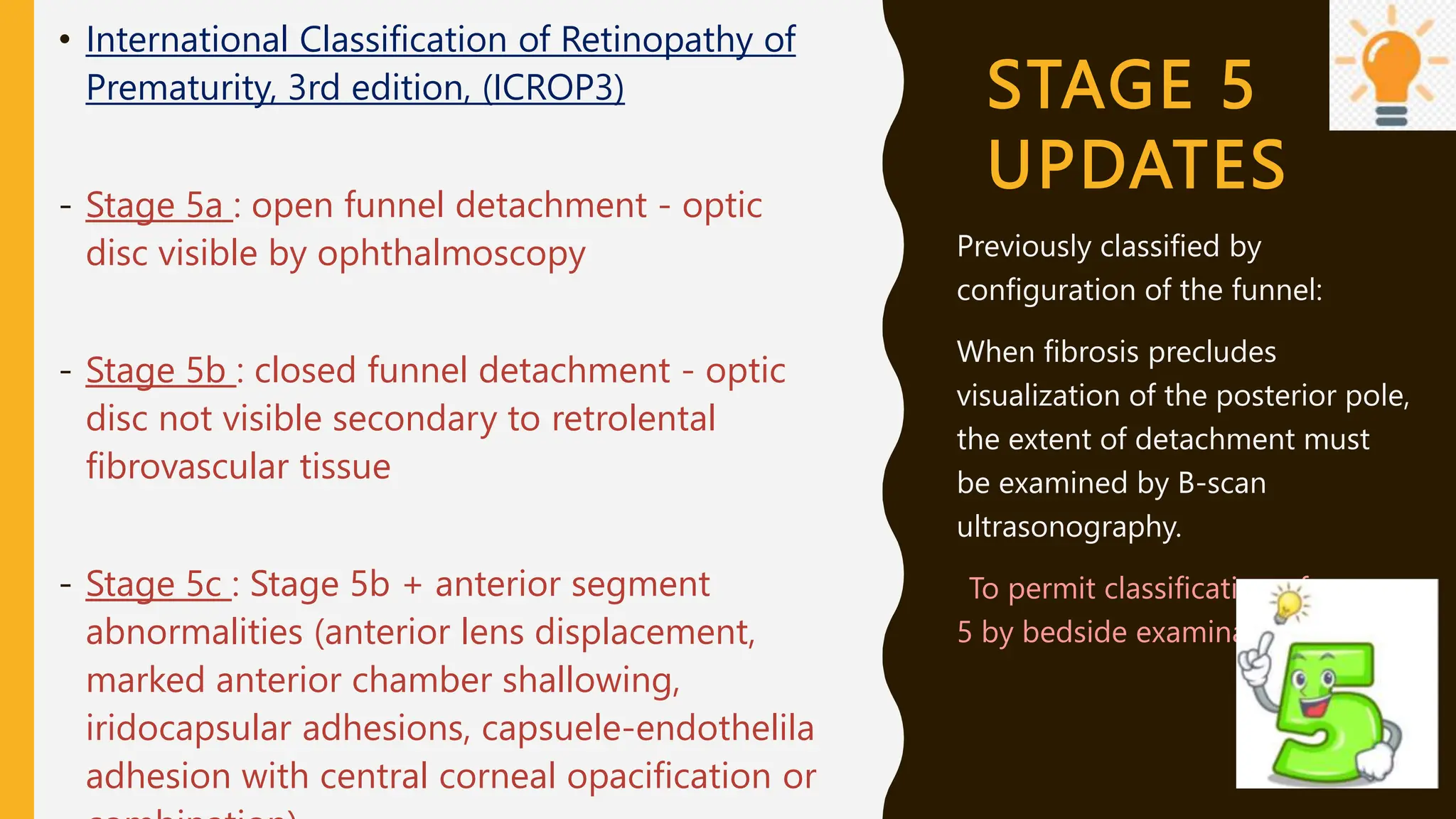
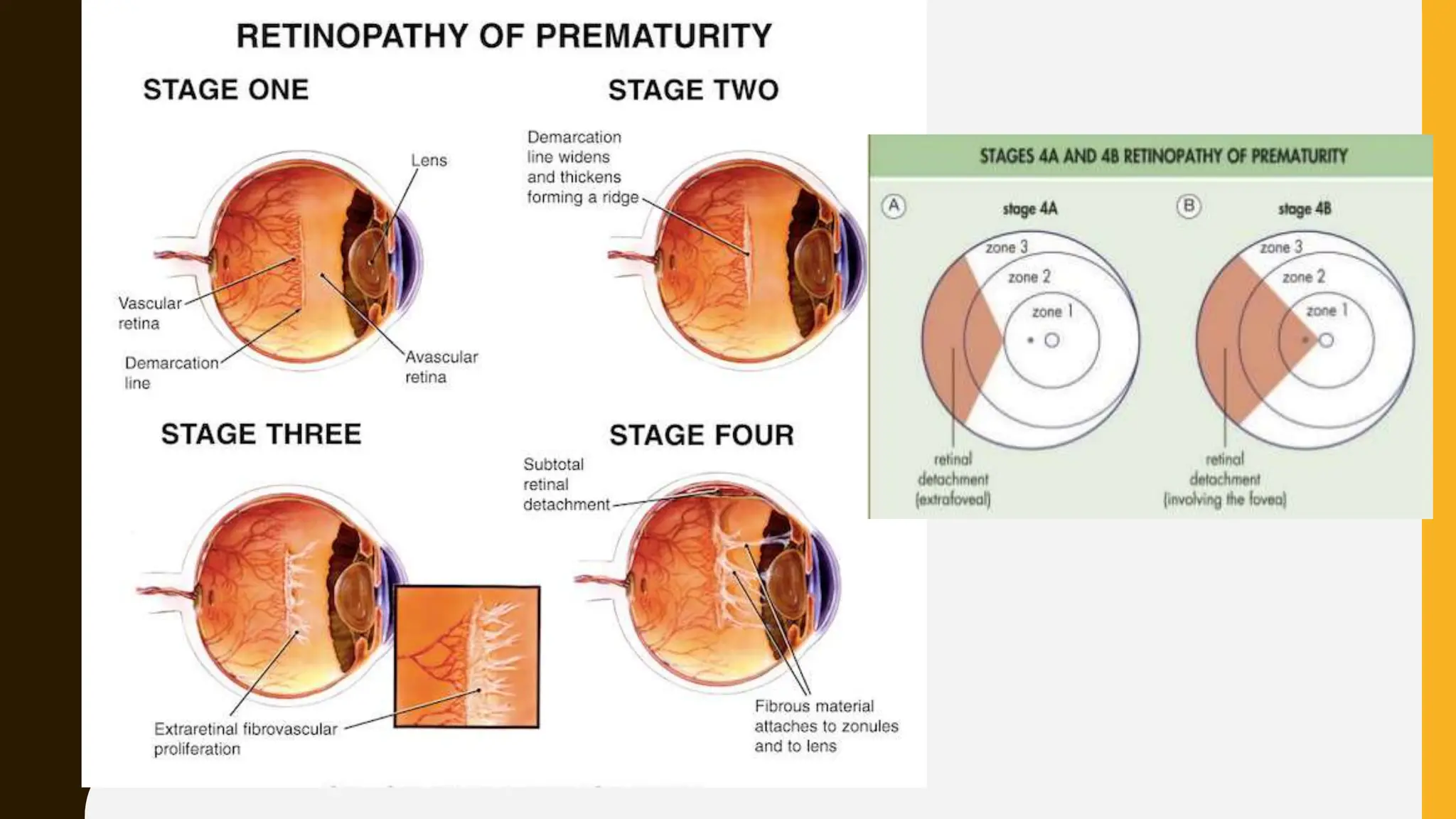
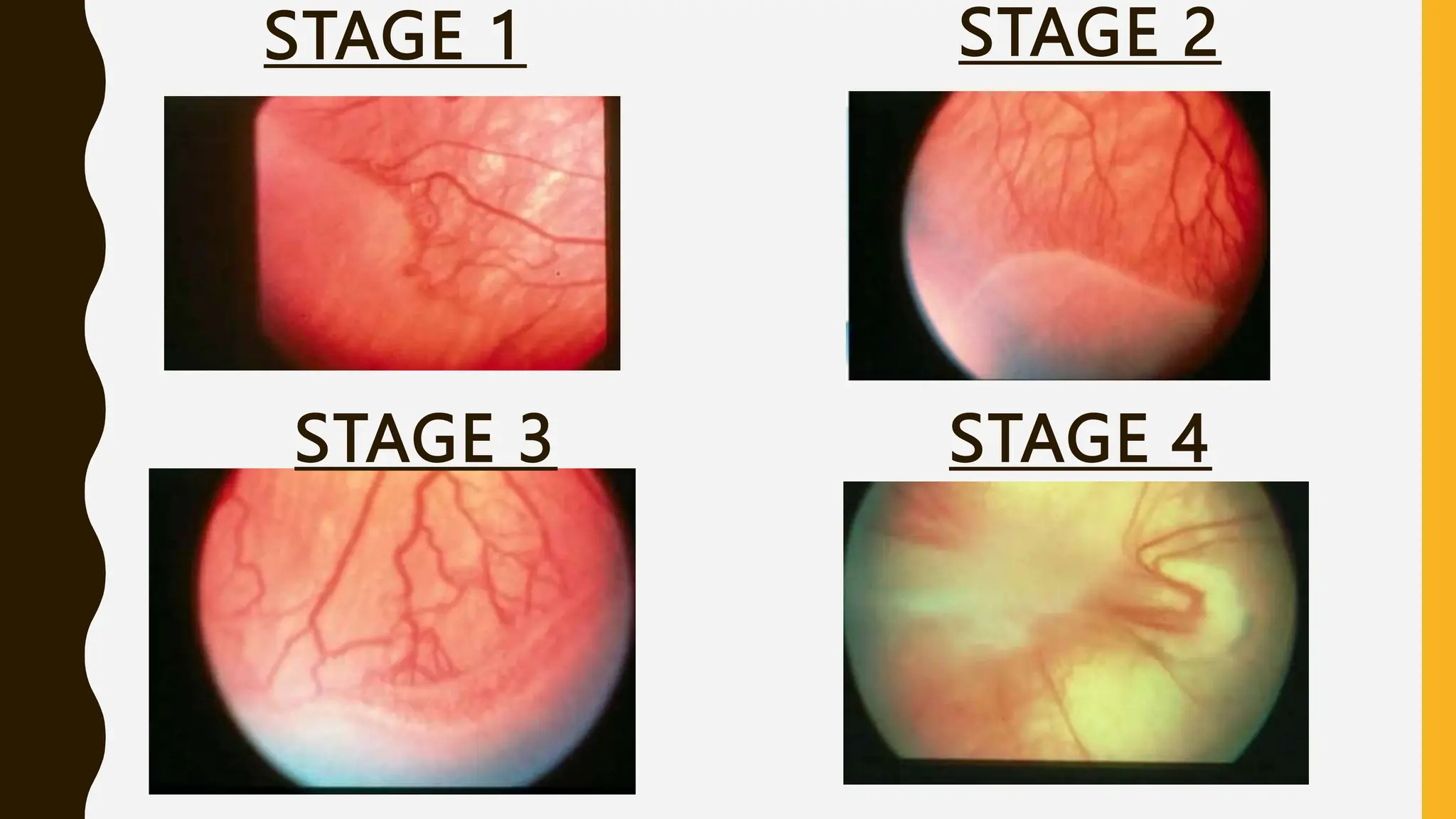
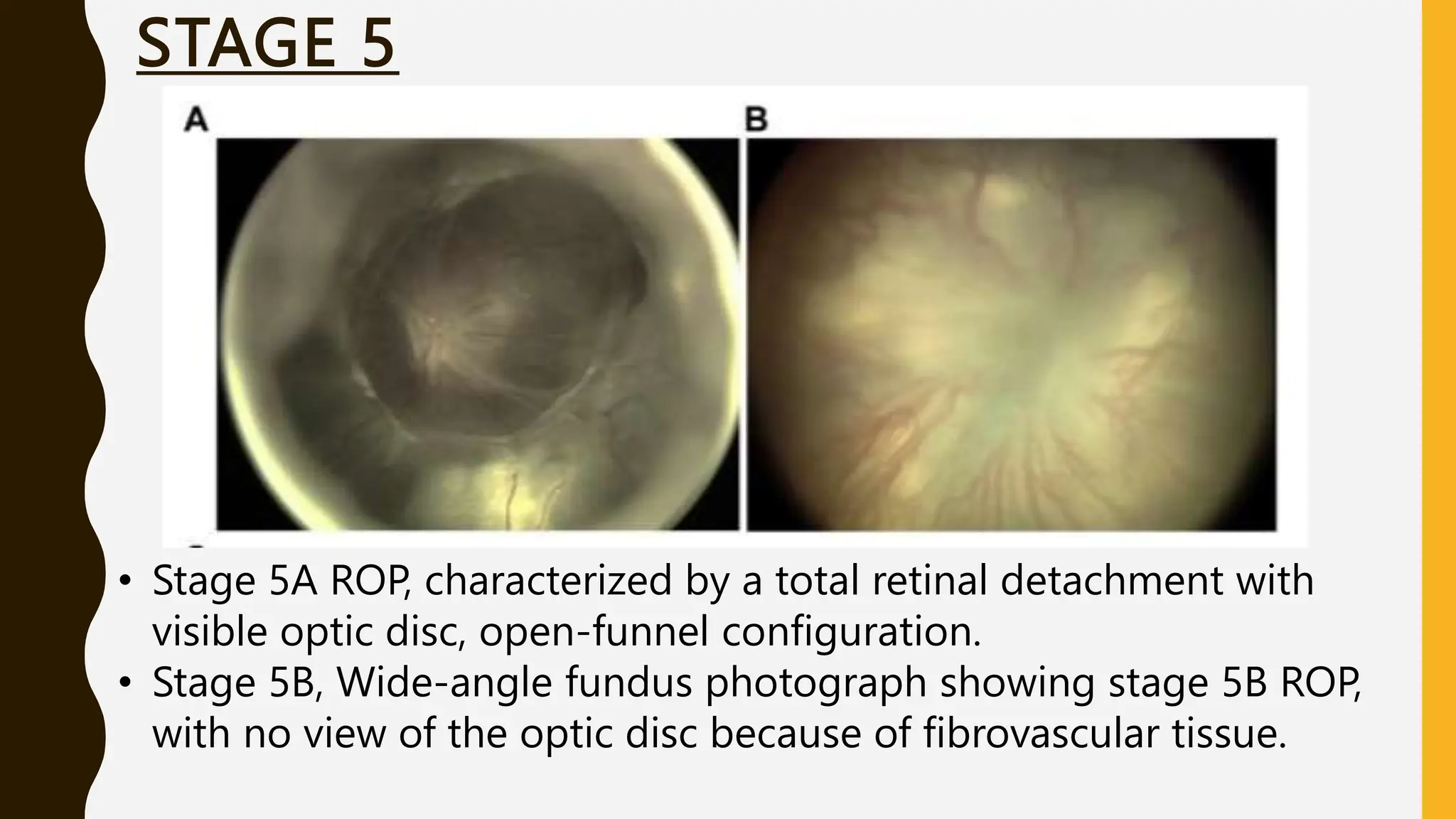
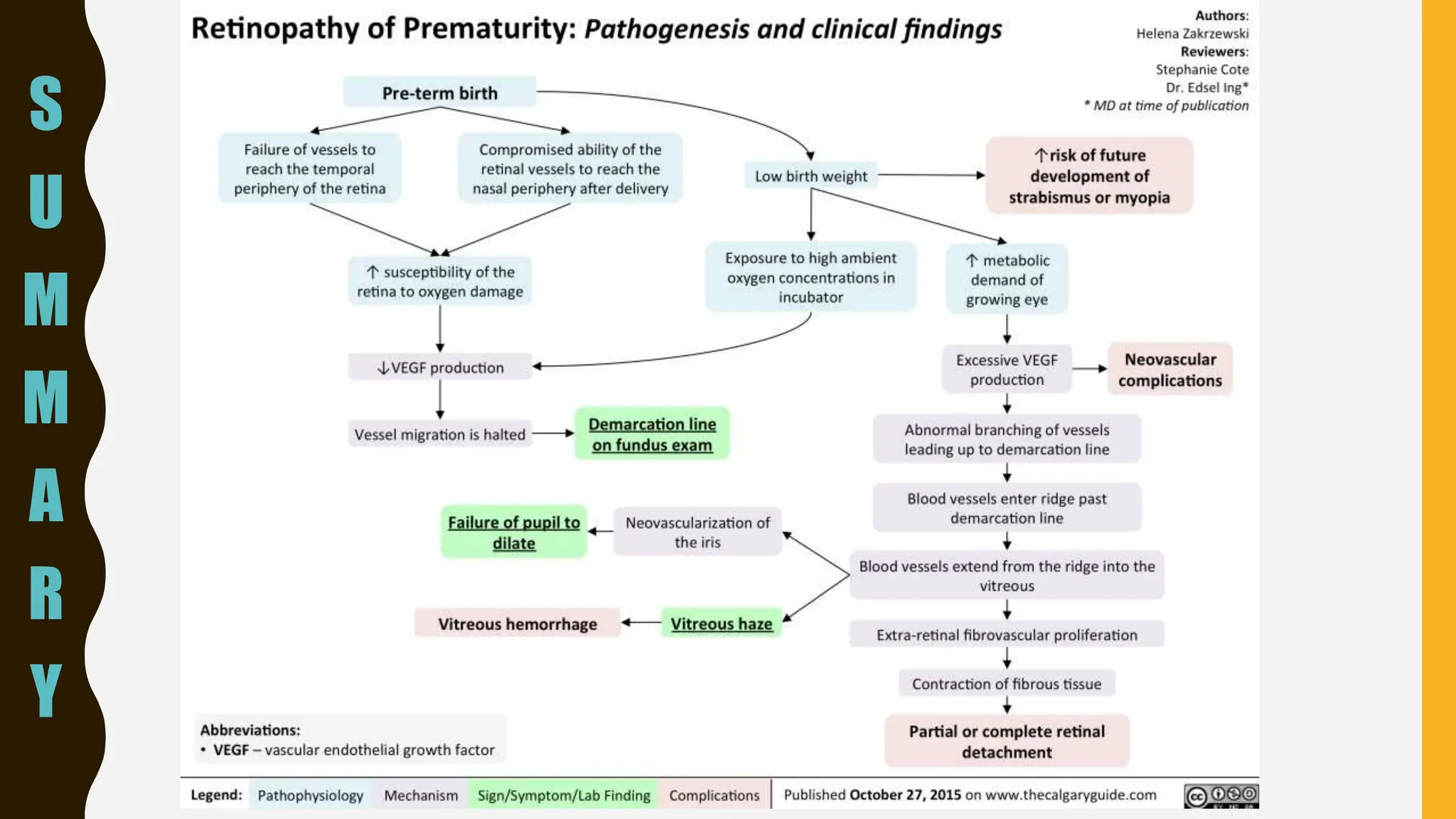
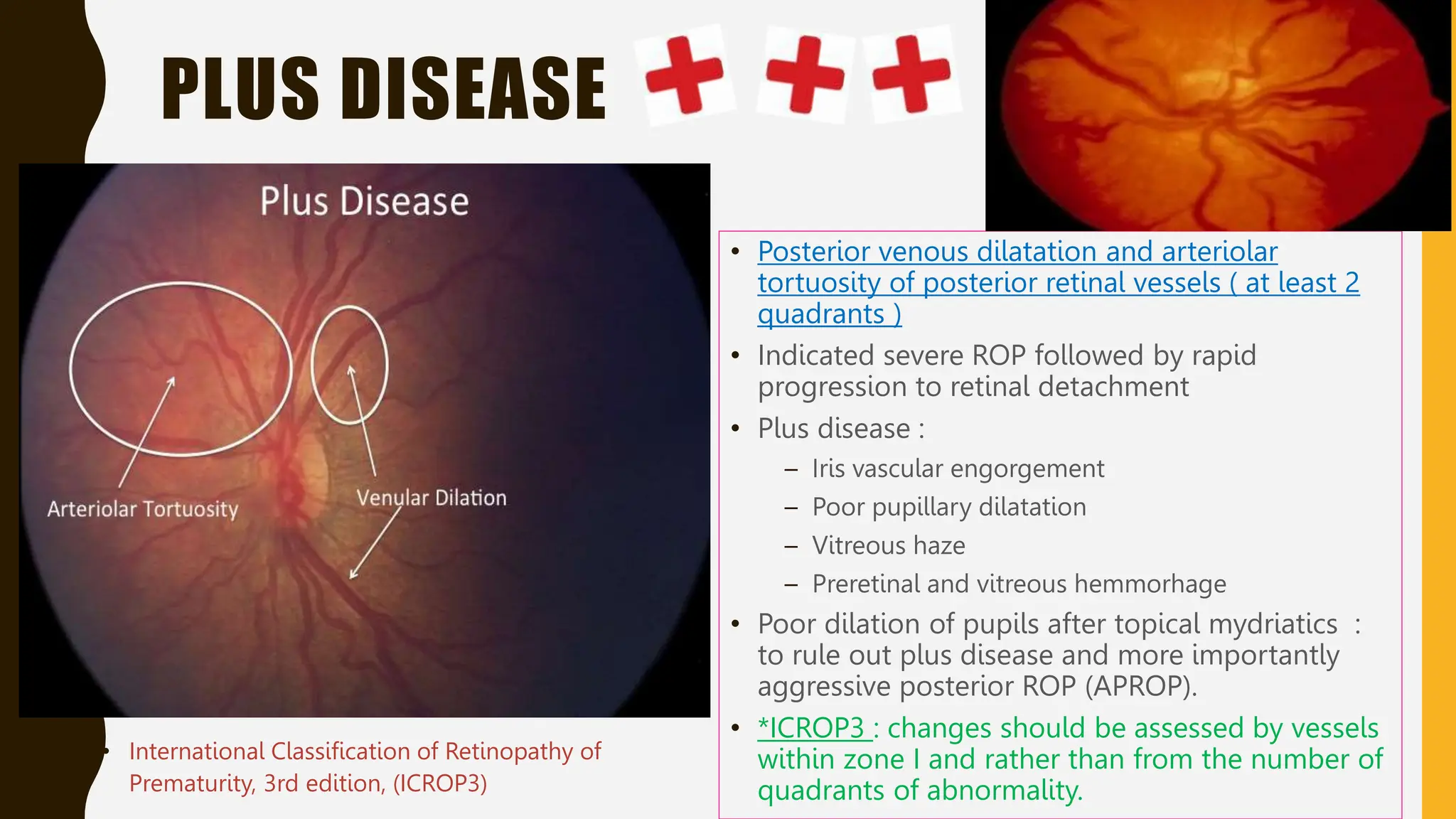
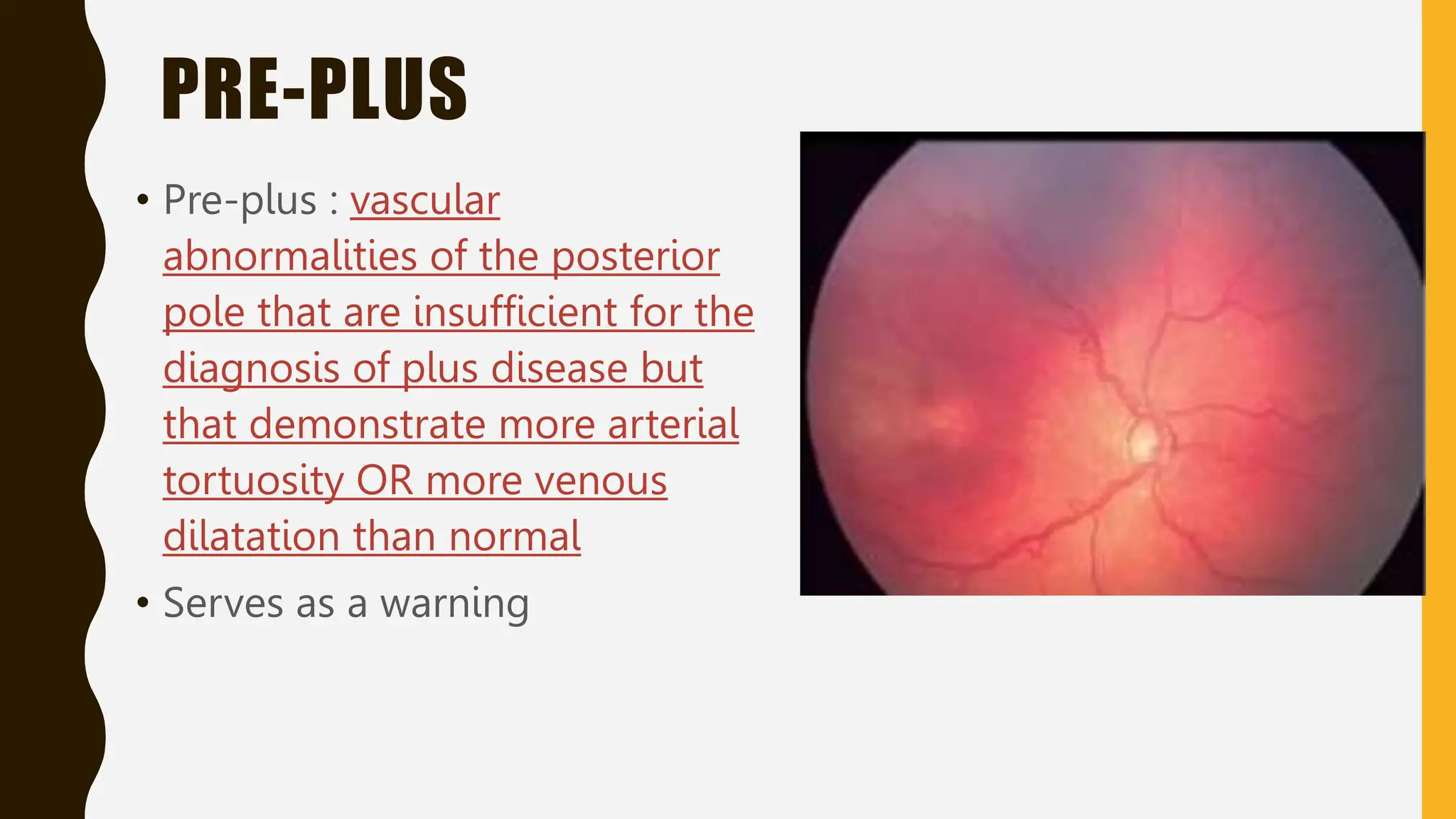
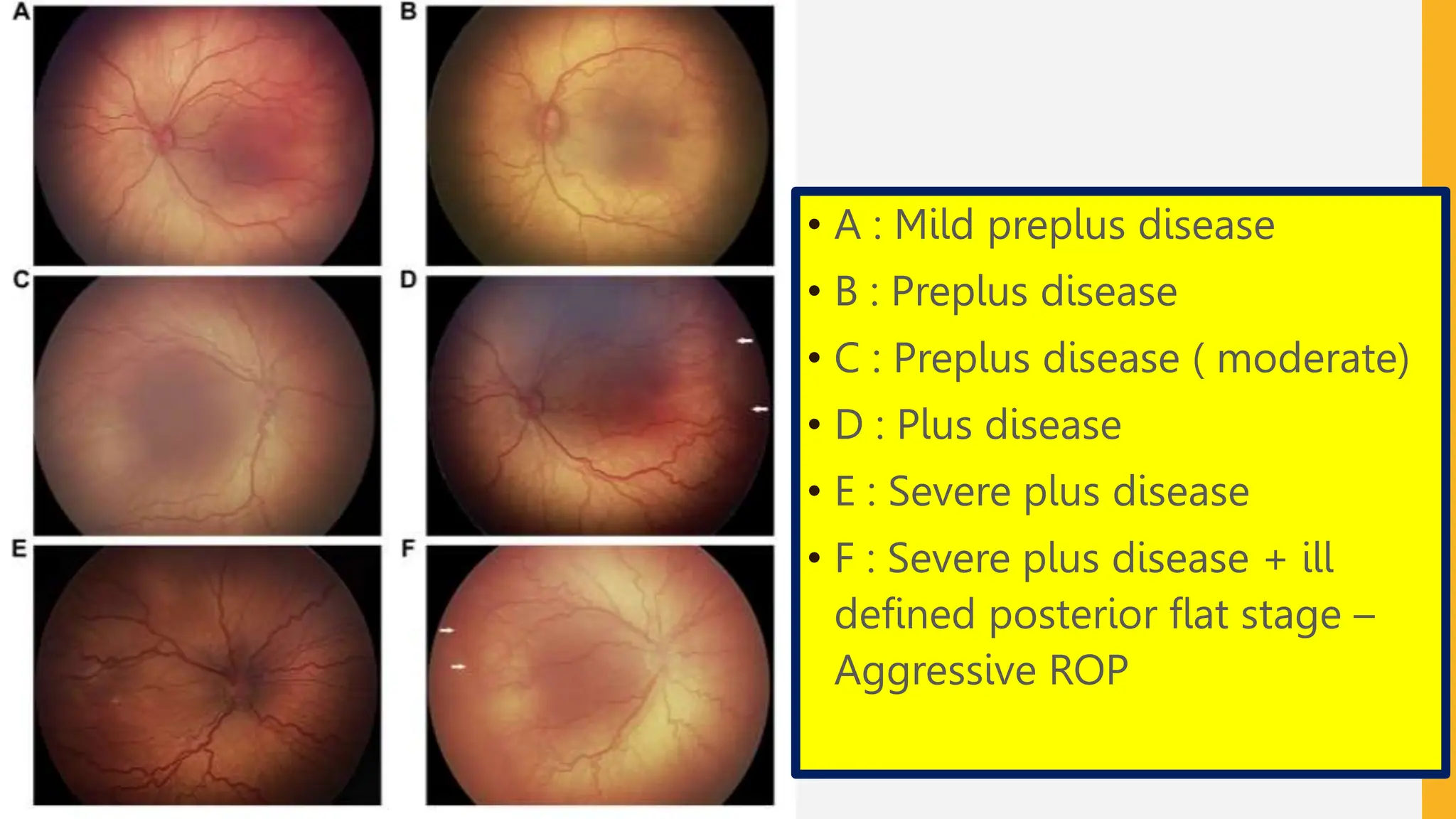
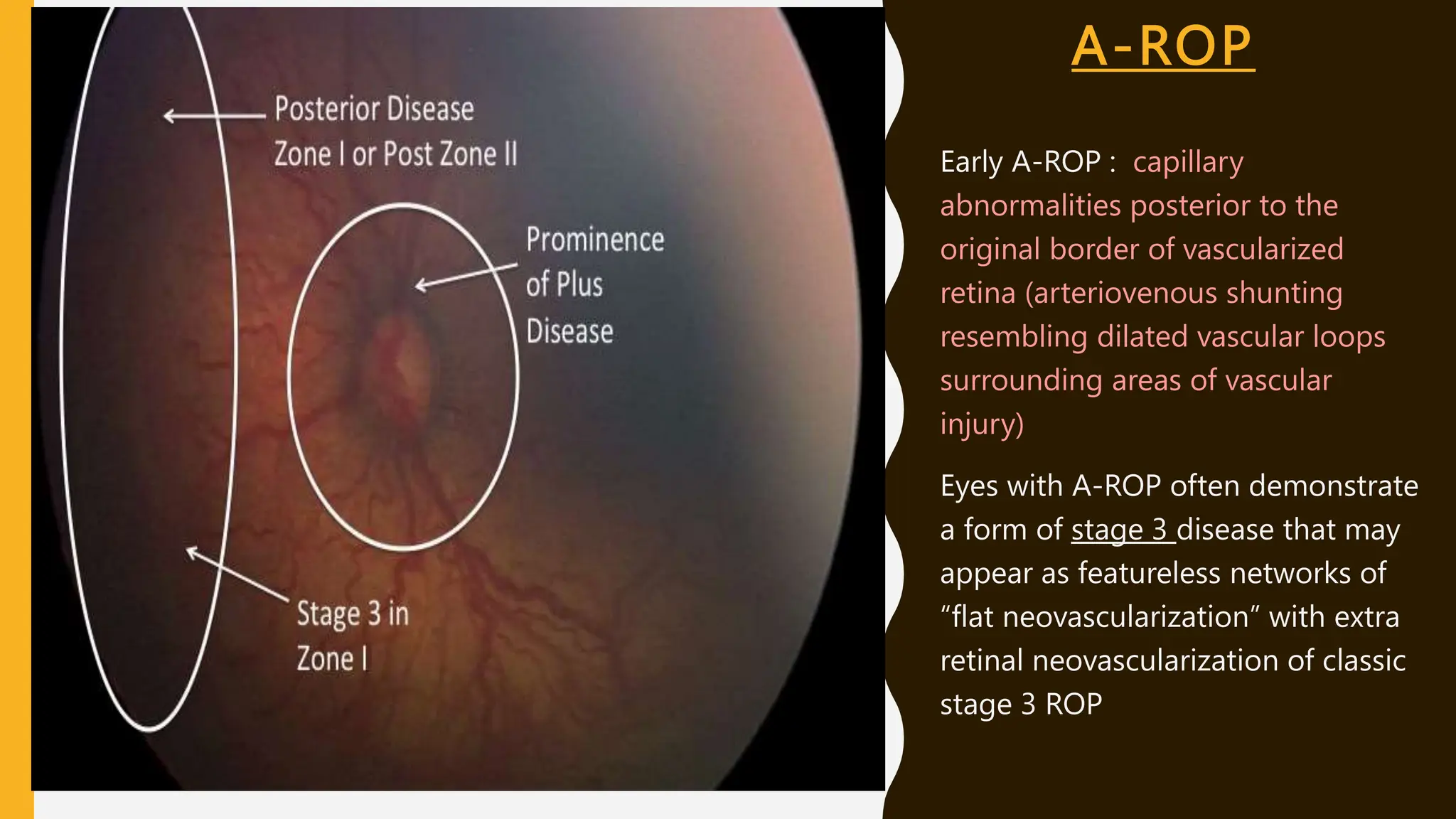
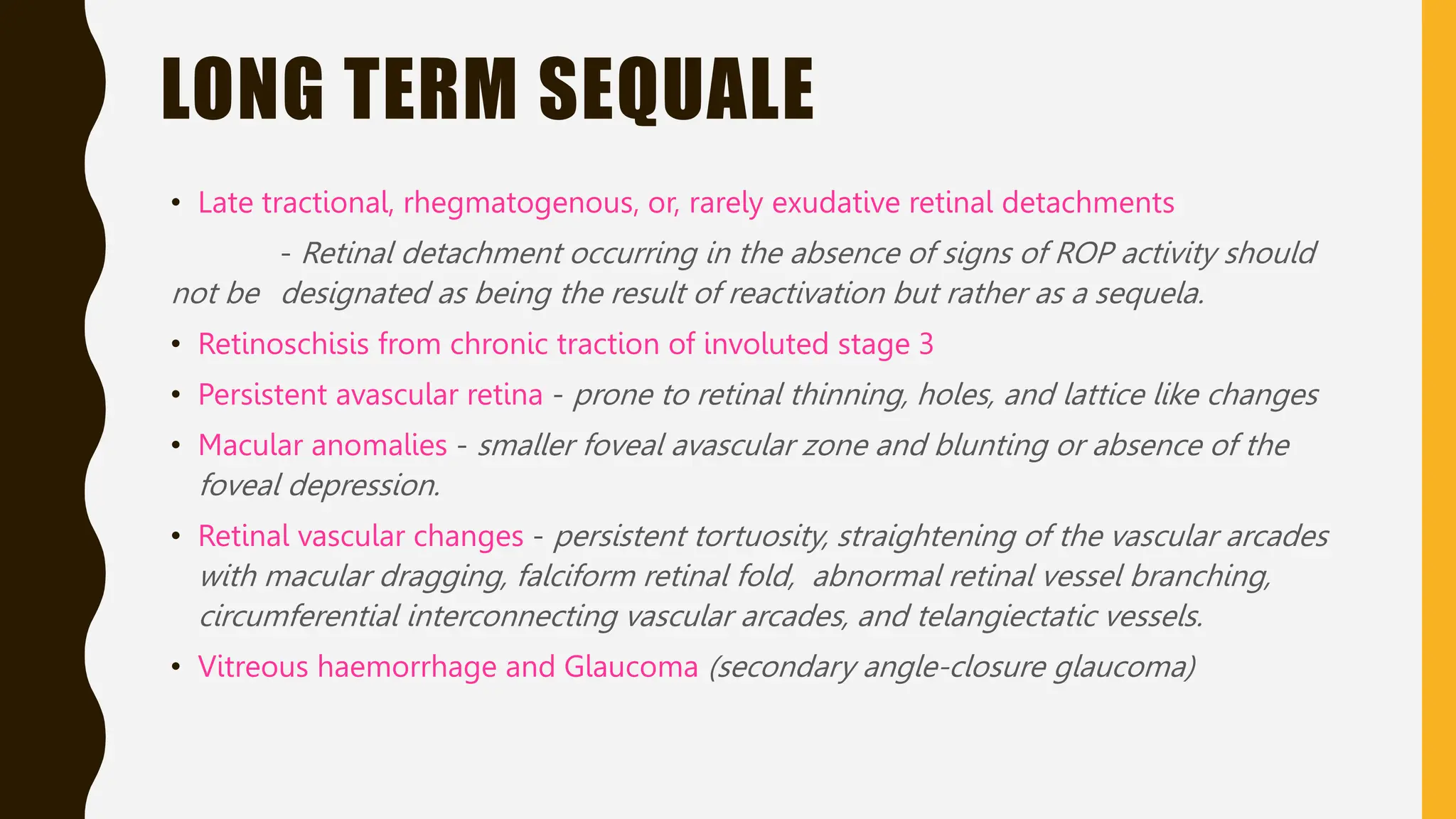
Retinopathy of prematurity (ROP) is a vasoproliferative disorder affecting primarily preterm infants, leading to potential blindness due to immature retinal vascularization. It has exhibited three epidemic waves, with significant risk factors including low birth weight and oxygen therapy. The document outlines the pathophysiology, classification, stages, and potential complications related to ROP, including aggressive forms and long-term consequences for affected infants.