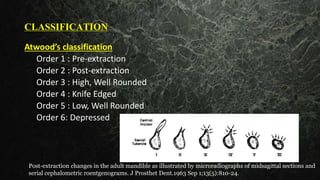
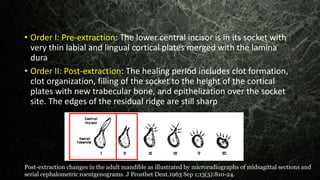
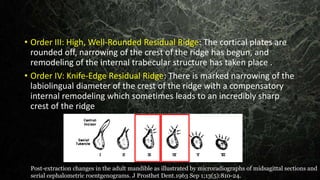
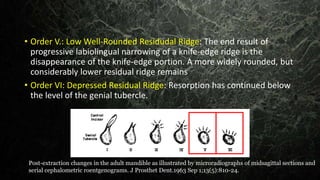
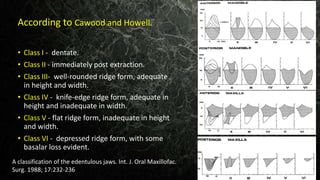
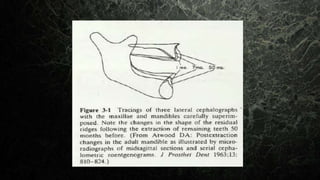
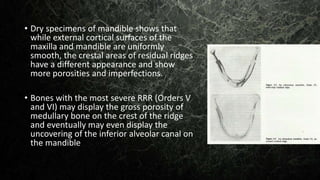
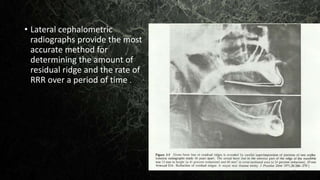
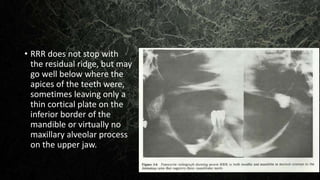
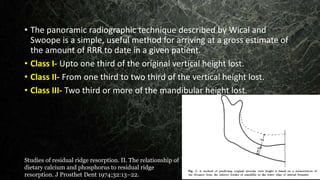
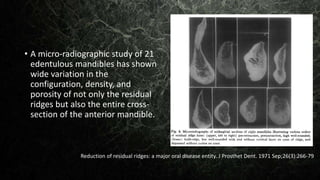
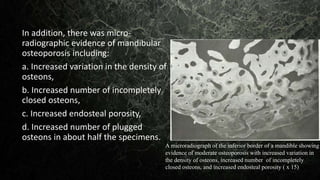
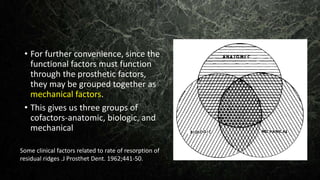
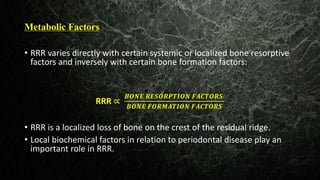
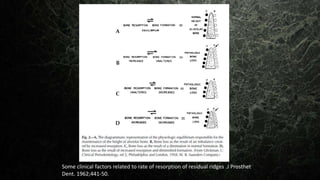
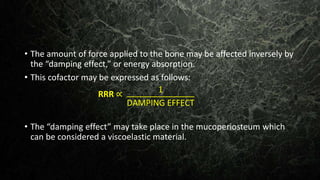
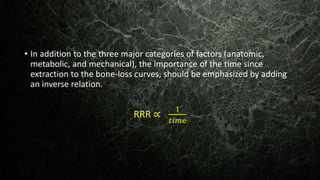
The document discusses residual ridge resorption (RRR), which is the diminishing quantity and quality of the residual ridge after tooth extraction. RRR is caused by ongoing bone resorption after healing is complete. It describes the classification of RRR orders based on ridge shape. The pathology involves microscopic evidence of osteoclastic activity and reduced bone density. The pathophysiology is an imbalance where resorption exceeds formation over time, progressively reducing the ridge.