This document outlines the purposes and policies around records and reports maintained in hospitals. It discusses:
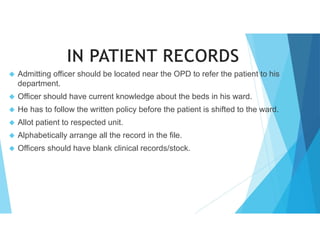
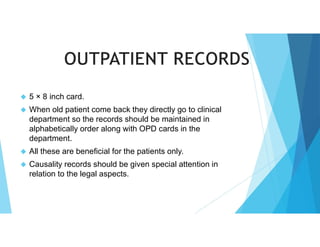
1) The definition of medical records as clinical, scientific, administrative, and legal documents that justify a patient's diagnosis and treatment.
2) The purposes of medical records which include studying patients, avoiding omissions, ensuring continuity of care, serving as legal evidence, and providing insurance information.
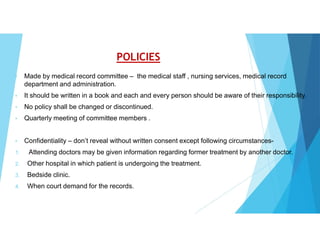
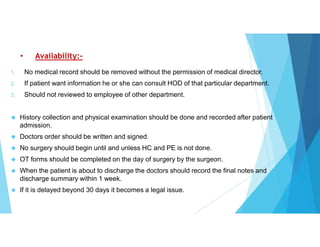
3) Hospital policies for medical records including documenting employee work, evaluating medical staff performance, and aiding future planning.