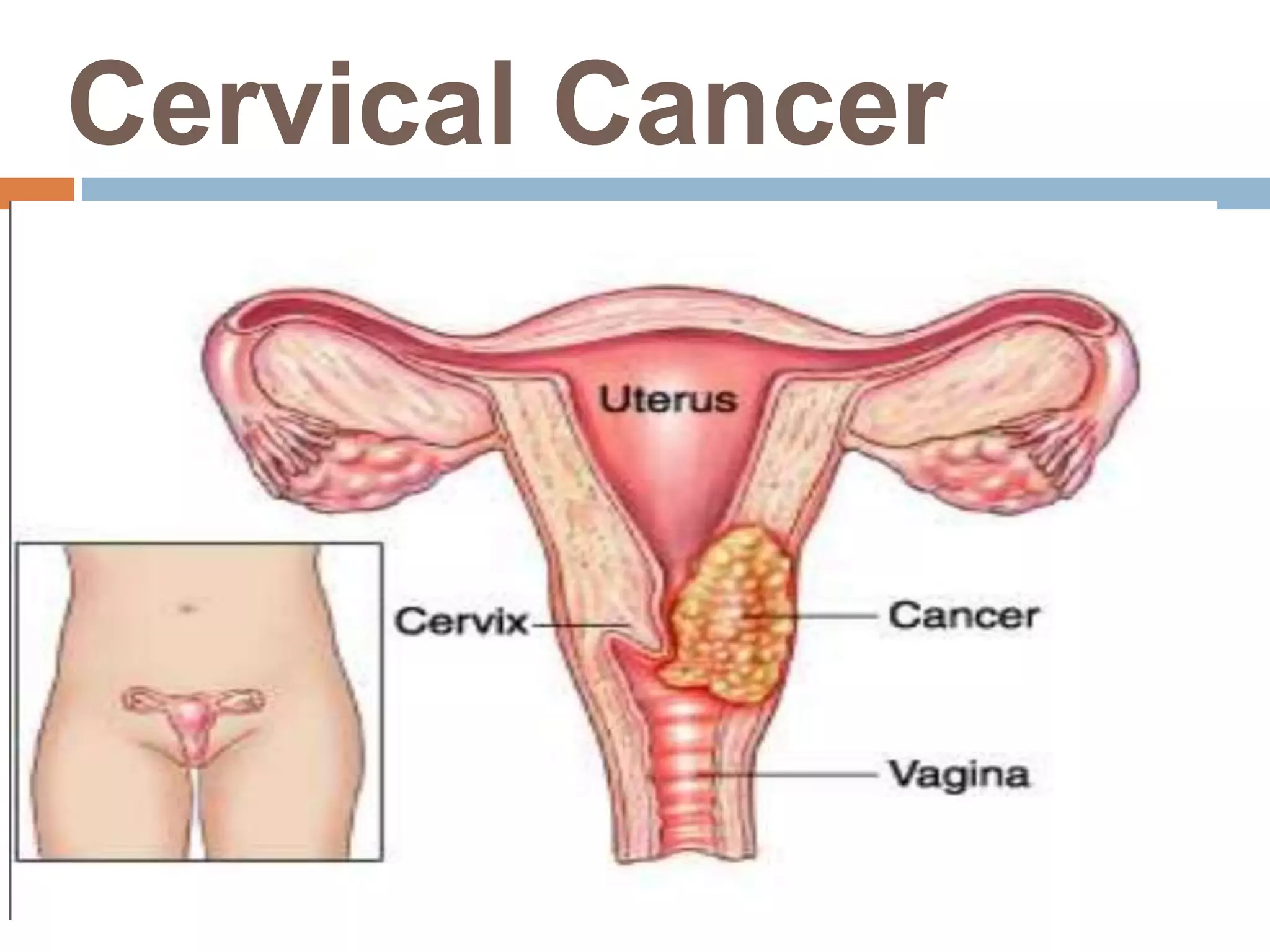
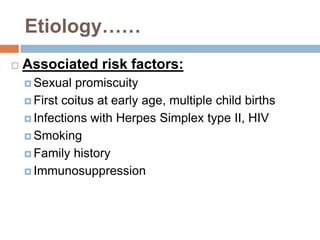
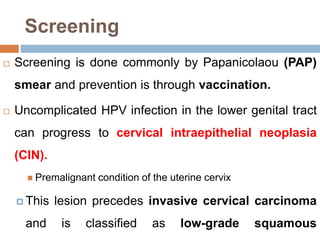
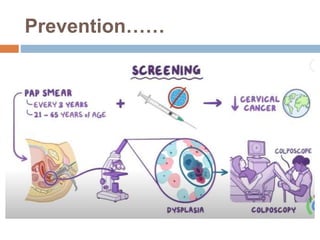
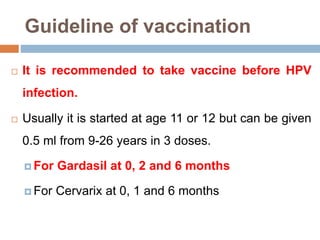
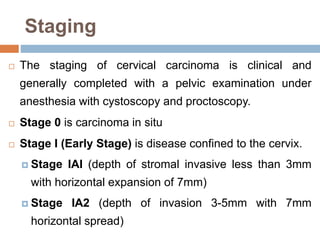
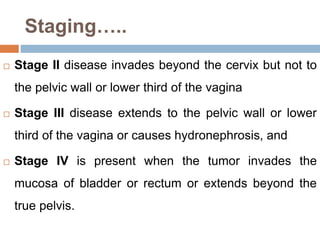
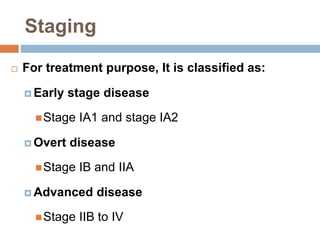
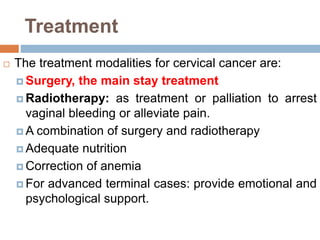
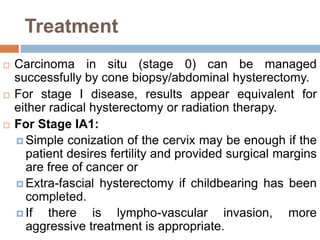
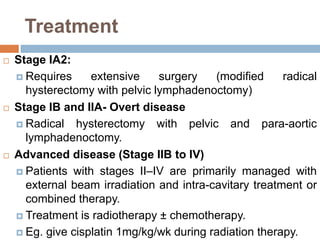
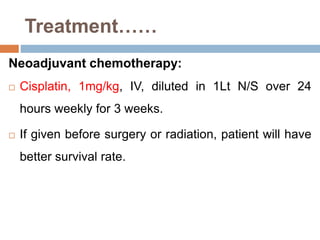
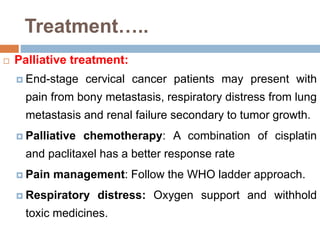
Cervical cancer is commonly caused by HPV infection and is preventable through vaccination and screening. The document discusses cervical cancer causes, risk factors, screening recommendations including Pap smears, vaccination for HPV, and treatment options depending on stage of disease. For an asymptomatic 66-year-old woman diagnosed with late stage IIB cervical cancer, investigations and staging confirmed an invasive cervical mass requiring a combination of surgery and radiotherapy or chemoradiation treatment.